Advances in the treatment of patients with cystic fibrosis (CF) are progressively prolonging their lives and its quality. The median life expectancy of CF patients is now 47.7 years, whereas approximately 30 years ago it was barely 27 years of age. Still respiratory failure is the most common primary cause of death in CF patients [1]. When all other therapies fail, lung transplantation remains the only viable option to prolong survival.
Various factors may influence the outcome of the lung transplant procedure. Size matching between donor and recipient is still considered to be one of the most crucial issues and in CF patients it is taken to another level as these individuals are often malnourished. As a result, this group of patients tends to have longer waiting times for transplantation [2]. Patients in need of urgent transplantation cannot wait for size-matched organs, and therefore various methods of cadaveric donor lung downsizing have been developed and successfully applied. Basically, there are three possible methods of lung tailoring – simple wedge resection, resection outside the anatomical borders and lobar transplantation. The latter is performed when there is a large size discrepancy between donor and recipient.
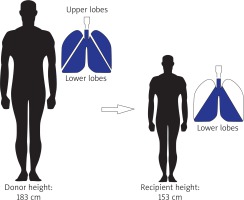
In 2017, a 23-year old female patient from Poland, of blood group A, who presented with cystic fibrosis, pulmonary hypertension and oxygen-dependent respiratory failure, was referred to our unit for further evaluation of possible lung transplantation. Since 2 years she has been experiencing the increasing frequency of exacerbations requiring antibiotic therapy and hospitalization. Preoperative chest X-ray and cpmputed tomography (CT) scanning demonstrated the presence of thick-walled bronchiectasis (Figs. 1 A, B). The patient met the lung transplantation criteria according to the ISHLT guidelines [3]. An expedited work-up was completed and the ethics committee approved the procedure. On June 19, 2017, the patient underwent the transplantation procedure. The transplanted organ was acquired from a 25-year old male patient, of blood group 0, with the height of 183 cm and weight of 107 kg, diagnosed with brain death due to intracranial injury resulting from a car accident. He had no relevant medical history. To overcome the magnitude of height disparity between the donor and the recipient, bilateral transplantation of single lower lobes was performed (Fig. 2).
Fig. 1
A – Preoperative chest X-ray. B – Preoperative CT scanning showing the presence of thick-walled bronchiectasis. C – Chest X-ray performed 6 months after the transplantation. D – CT scanning performed one year after the transplantation showing no significant pulmonary findings

Fig. 2
Bilateral lobar transplant was performed to overcome the magnitude of height disparity between the donor and the recipient
The operation was performed on veno-arterial extracorporeal membrane oxygenation (VA-ECMO) with central cannulation. The surgical exposure was via bilateral thoracotomy and transverse sternotomy through the fifth intercostal space – the “clamshell” incision. The donor lungs were divided on the side table. The recipient’s right and left lung were excised in a standard fashion. On the right side the donor’s intermediate bronchus with stapled middle lobe bronchus was sutured to the recipient’s right main bronchus. The recipient’s pulmonary arteries were sutured to the donor’s intermediate artery on the right side and to the lower lobe artery on the left. The donor’s lower pulmonary veins were sutured to the recipient’s pulmonary venous atrial cuff on both sides. Bronchial anastomoses were performed utilizing running absorbable PDS 4-0 monofilament suture and the vessels were sutured using running nonabsorbable Prolene 4-0 monofilament suture. Only 3000 IU of heparin were administered at the initiation of ECMO. The entire transplantation procedure lasted 5.5 h.
During the surgical procedure there were no complications. The patient was transferred to the intensive care unit with a stay of 4 days. A single episode of acute allograft rejection was recognized and promptly treated, with good results. Treatment included discontinuation of cyclosporine with a switch to tacrolimus. The patient was hospitalized for 16 more days, with no additional clinical events. The patient is currently under the follow-up care carried out every 6 months. No other complications have been recorded. Chest X-ray performed 6 months after the transplantation and CT scanning performed 1 year after the surgery showed no significant pulmonary findings (Figs. 1 C, D).
Cadaveric transplantation has been the basic approach since the beginning of lung transplantation, but it is still limited by the scarcity of the donor pool. As the number of patients on the transplant waiting list increases yearly, compromises must be made to provide organs for those critically ill. Sometimes additional compromises are made in terms of donor-recipient size matching, but there have been several reports that a mismatched lung graft may cause potential problems [4–6]. The oversized graft may lead to poorer gas exchange, elevated pulmonary vascular resistance, impaired diaphragm movement, atelectasis and an increased risk for secondary infection. On the other hand, an undersized graft may over-inflate and lead to persistent pleural effusion, increased breathing effort and, in extreme cases, hemodynamic instability. The use of cadaveric lobar transplantation is still not considered to be a standard procedure, in spite of the fact that it allows larger grafts to be used in urgent pediatric and small adult patients with no time to wait for an ideal size-matched donor. In our experience this procedure is safe, does not add significant morbidity and its achieved outcome rates are equivalent to those for lung transplantation with size-matched grafts. Similar conclusions have been reached by other studies [5, 6]. To the best of our knowledge, this is the first report regarding this type of lung transplantation procedure performed in Poland. Carefully selected patients with size-unmatched donors demonstrate results that are comparable to those of lung transplantation with size-matched grafts. We hope that this report will encourage other units to consider cadaveric lobar transplantation for their urgently listed patients with a smaller chest cavity.






