We describe a case of an 80-year-old male patient with symptomatic severe aortic stenosis treated with transcatheter valve implantation (TAVI). The most common and preferred type of transcatheter valve delivery is through the femoral artery. However, if transfemoral access is not possible, an alternate route may be chosen. Such routes include, but are not limited to, direct aortic access, subclavian/axillary access, or transapical access, each one having their advantages and disadvantages [1, 2]. In our patient, transfemoral access was not possible due to extreme tortuosity of both pelvic arteries revealed on preoperative angiography. Computed tomography (CT) angiography was used to assess the diameter of the subclavian, axillary and brachial arteries (Figures 1 A, B). Duplex ultrasound verified the proximal diameter of the right brachial artery to be 6.7 mm (Figure 1 C). This diameter was sufficient to perform TAVI with an Evolut R 34 mm valve via the brachial artery. This approach offers multiple benefits, primarily, relatively easy access, avoidance of preparation of an artery in the otherwise very complex axillary and subclavian region, therefore decreasing chances of iatrogenic injury, and a quick recovery after the procedure. Other benefits of transbrachial delivery are usually minimal tortuosity of the arterial segment and minimal calcification. A major limitation of this approach is the diameter of the brachial artery. Other disadvantages are the same as for subclavian/axillary access and involve the angle of the aorta from the horizontal plane, as well as the unfavorable angle of valve delivery into the left ventricular outflow tract.
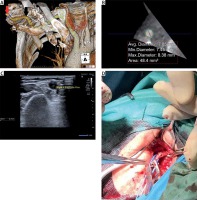
Figure 1
A – Computed tomography angiographic image of the subclavian, axillary and brachial arteries (indicated by a green line). Blue circle: approximate start of a proximal segment of the right brachial artery. Red arrow: the right brachial artery. Black arrow: the right axillary artery. B –* Cross-sectional view of the area indicated in Figure 1 A with measured diameter dimensions. C – Duplex ultrasound image of the proximal diameter of the right brachial artery. D – Brachial artery preparation
Under full general anesthesia, a 45 cm long 5F sheath was introduced through the right femoral artery, and a temporary pacemaker via the right femoral vein. Surgical preparation of the right brachial artery was conducted (Figure 1 D). Anatomically, the brachial artery is a continuation of the axillary artery beyond the lower margin of the teres major muscle. After the arteriotomy of the brachial artery, a 18F sheath was introduced. Passage of the guidewire via the brachiocephalic artery was controlled by contralateral injection of contrast dye by a Vitek catheter (Cook, Bloomington, IN, USA). The CoreValve Evolut R 34 mm (Medtronic, Minneapolis, MN, USA) was delivered through the EnVeo R delivery catheter system. At the end of the procedure, the brachial artery was closed by arterial suture. Echocardiography performed after TAVI demonstrated only a trace of paravalvular regurgitation and a mean gradient of 11 mm Hg. One-year after implantation, echocardiographic findings were unchanged compared to pre-discharge findings. The patient was completely asymptomatic and doing well, maintaining a physically active lifestyle. There was no clinical evidence of any forearm dysfunction after the procedure or at the 1-year follow-up examination. As this was our first case of transbrachial access, the decision was made to perform the procedure in full general anesthesia and with the use of surgical arteriotomy. However, performing the entire procedure percutaneously and under local anesthesia might be plausible, as in selected cases, fully percutaneous large-bore interventions are feasible [3].
To our knowledge, this is the first reported case of transbrachial TAVI.







