Introduction
Lymphoma is a haematological malignancy arising from the clonal proliferation of lymphocytes (B, T, or NK cells) at different maturation stages. It often presents with night sweats, fatigue, enlarged painless lymph nodes, and weight loss, and it is categorized into 2 large subgroups: Hodgkin (10%) and non-Hodgkin lymphoma (90%) [1, 2]. Diagnosis of lymphoma is confirmed by tissue biopsy and further evaluated by PET/CT scans to measure uptake of radiolabelled fluorodeoxyglucose to assess the biological activity of lymphoma in different sites. Pericardial involvement in systemic malignancies is common and is seen in around 1-20% of autopsies in cancer patients [3, 4]. Pericardial involvement includes various degrees of pathologies such as pericarditis, pericardial effusion, pericardial tamponade, and constrictive pericarditis.
Pericardial effusion is the accumulation of fluid in the pericardial sac. Normally, there are between 10 and 50 ml of pericardial fluid produced by ultrafiltration of plasma from the epicardial capillaries and effusion of interstitial fluid from the underlying myocardium. Large symptomatic pericardial effusions are often the initial clinical presentation of many systemic malignancies [5]. Symptomatic effusion often presents with dyspnoea, tachycardia, and echocardiographic features of right heart impairment [5, 6]. Pericardial effusion stems mainly from blockage of the lymphatic and venous drainage of the pericardium by malignant seeds or via compression from neighbouring enlarged lymph nodes. Importantly, pericardial effusions in cancer patients can also be triggered by chemotherapy and radiotherapy [7–11]. Other causes of effusion, such as infections and autoimmune diseases, are also seen in these patients.
Cardiac tamponade is an accumulation of pericardial fluid with compression of all cardiac chambers due to increased pericardial pressure [12, 13]. Under normal conditions, the pericardium can accommodate physiological changes in cardiac volume. However, after its reserve volume is exceeded, or in cases of acute effusions, impairment of the underlying haemodynamics of the left and right heart chambers occurs. Venous return and (subsequently) cardiac output are compromised.
Multiple case reports have been published including cases of Hodgkin and non-Hodgkin Lymphoma patients presenting with pericardial effusion [14–18]. However, pericardial effusion leading to cardiac tamponade as an initial presentation of lymphoma is rare. Moreover, the chronological relationship between lymphoma and pericardial tamponade is not very well understood. In this review, we aimed to compile all the relevant studies of patients presenting with pericardial tamponade before or after diagnosis of lymphoma, describe the clinical presentations of patients with lymphoma and cardiac tamponade, and assess the difference in overall survival based on the timing of cardiac tamponade diagnosis.
Material and methods
Literature search
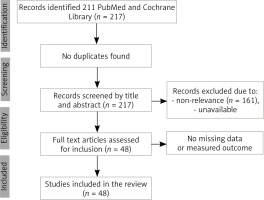
A comprehensive search strategy was conducted in the following databases: PubMed and Cochrane Library, using the following keywords: Lymphoma AND Cardiac Tamponade. The search was performed on 10 January 2020, and there was no restriction identified in terms of the publication period. The literature search was done in compliance with PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analysis). All clinical studies were then extracted using the title and abstract of each study. The criteria for eligibility included cases with a confirmed diagnosis of lymphoma and cardiac tamponade, human studies, and publication in English language. The exclusion criteria entailed unconfirmed diagnosis of lymphoma, presence of pericardial effusion without cardiac tamponade, and lack of full texts or measured outcomes.
Quality assessment
The first 3 autvhors independently examined the retrieved the search items and ensured there were no major discrepancies or duplicates. The quality assessment tool that was developed by Murad et al. was utilized to evaluate the quality of each case study. This tool assesses each study in 4 domains: selection, ascertainment, causality, and reporting. Each domain carries 1 point, and hence, each case is scored out of 4. Scores of 1 and 2 represent poor quality, 3 is considered fair, and 4 indicates good quality. Questions about drug events were removed due to the lack of their application in the present study.
Data extraction
The following information was extracted from each study: age, gender, clinical presentation and duration of illness, the timing of cardiac tamponade diagnosis (whether before or after diagnosis of lymphoma), and associated comorbid conditions or infections, in addition to the presence of any other cancer. Information regarding diagnostic studies, management strategies, and prognosis was also gathered from these reports.
Statistical analysis
The descriptive statistics were performed by addressing the number and percentage of cases for each measured categorical variable. Data were reported for continuous variables as mean followed by standard deviation, or median followed by a range or 95% confidence interval. Survival analysis was processed using Kaplan-Meyer curves, and the results were reported in graphs, in addition to median survival and its 95% confidence interval. The log-rank test was used to examine the difference in median survivals of 2 independent groups. A p-value of less than 0.05 was considered statistically significant. The statistical analysis was processed using IBM Statistical Package for Social Sciences (SPSS) version 20.
Results
The literature search of identified terms in PubMed and Cochrane Library yielded a total of 217 research articles, and no systematic review was found. After reviewing each study’s title and abstract, 161 studies were excluded due to non-relevance, and 7 other studies were also removed due to the unavailability of abstracts and full texts. The final number of eligible studies for analysis was 48 research articles with adequate reporting of measured outcomes. These studies consisted of case reports and case series and described a total of 52 cases (Figure 1).
A quality assessment tool was utilised to examine each enrolled case study’s quality, and, when applying this method, 23 cases were identified as good quality, 19 cases were marked as fair quality, while 10 cases were reported to be of poor quality. The median age of the patients was 52 years, ranging between 9 and 94 years. Around 73% of cases were reported in male patients, and 14 cases were described in female patients. Most of the patients did not report any comorbid condition (75%). However, 5 patients had chronic arrhythmias: 3 had a history of third-degree atrioventricular block and had a pacemaker in place, while 2 patients had chronic atrial fibrillation. Moreover, 3 patients were diagnosed with other cancers in the past, including hepatocellular carcinoma, basal cell cancer, and squamous cell carcinoma of the vocal cords (Table 1).
Table 1
Characteristics of patients in the study (n = 52)
* Comorbid conditions – abdominal aortic aneurysm, asthma, Barret’s oesophagus, chronic renal disease, congestive heart failure, coronary artery disease, diabetes mellitus, haemolytic anaemia, hyperlipidaemia, hypertension, hypothyroidism, obesity, obstructive sleep apnoea, peripheral neuropathy, pulmonary fibrosis
Most of the patients were diagnosed with lymphoma prior to hospital presentation (80.8%). Only 6 patients were noted to have primary cardiac lymphoma, while the majority of cases were considered to have secondary cardiac lymphoma (88.5%). Upon reviewing the type of lymphoma through cytology and immunohistochemistry, 49 patients were diagnosed with non-Hodgkin lymphoma, and of these cases, the most common subtype was large B-cell lymphoma (42.9%).
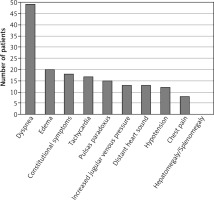
A large majority of patients presented to the hospital complaining of increased shortness of breath (94.2%), and around 35% of the cases presented with constitutional symptoms, including fever, chills, night sweat, myalgia, or fatigue. Overall, the average duration of illness was 14 days with a standard deviation of 23 days. A total of 13 patients had distant heart sounds, 12 cases were noted to be hypotensive, and 13 subjects were found to have increased jugular venous pressure (Figure 2).
About 65.4% of cardiac tamponade patients in the present study underwent a transthoracic echocardiogram, and four of them had a subsequent transoesophageal echocardiogram. The common echocardiogram finding was pericardial effusion (82.4%) followed by right atrial mass or collapse (32.4%). Furthermore, right ventricular diastolic collapse was noted in 10 case studies, while left ventricular collapse was demonstrated in 3 cases. However, there was no reporting of inferior vena cava dilation. Chest X-ray, on the other hand, was obtained in 30 cases, and chest computed tomography was performed in around 54% of the cases (Table 2). The most common radiographic finding was cardiomegaly or pericardial effusion, with or without pleural effusion (61.5%). Moreover, an electrocardiogram was performed in 15 patients, which revealed sinus tachycardia in half of the tested cases. Low-voltage QRS complexes were depicted in 3 cases, but there was no reporting of electrical alternans. In terms of laboratory workup, elevated lactate dehydrogenase (LDH) was found in 23% of the cases, and leukocytosis was noted in 6 patients. Cytology and immunohistochemistry results varied depending on the type of lymphoma.
Table 2
Diagnosis and management of patients with lymphoma and cardiac tamponade
The most common therapeutic option that was offered to these patients for the management of cardiac tamponade was pericardiocentesis (63.5%), followed by the pericardial window (15.4%). The amount of aspirated pericardial fluid was reported in 14 studies with an average of 862 ± 930 ml, and all fluid analyses revealed exudative fluid. Some patients had concomitant pleural effusion, and these cases underwent thoracentesis, which showed similar fluid analysis results (9.6%). Meanwhile, 34 patients were administered chemotherapy for the management of lymphoma (65.4%), and 7 patients underwent surgical resection (13.5%).
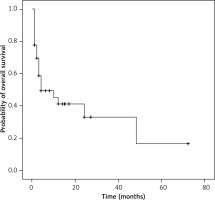
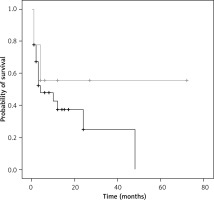
The median overall survival of patients with lymphoma and cardiac tamponade is 4 months, with a 95% confidence interval of 0 to 12 months (Figure 3). As stated earlier, compared to patients who were known to have lymphoma prior to presenting with cardiac tamponade, only 10 patients were diagnosed with lymphoma after diagnosis of cardiac tamponade. To explore if this was a potential influencing factor on the overall survival curve, the log-rank test was utilized. The test demonstrated no significant difference between median survivals of the 2 groups (p = 0.24) (Figure 4). Due to the small sample size of patients who had lymphoma diagnosis after cardiac tamponade (n = 10) and thus fewer deaths, the median survival could not be computed in that group.
Discussion
The incidence of haematological malignancies is on the rise in Africa. The number of new lymphoma cases is expected to nearly double over the next 2 decades, from approximately 25 000 in 2012 to more than 48 000 by 2035 [19]. A large part of this is because of the human immunodeficiency virus (HIV) epidemic, as well as population growth and aging. Lymphoma diagnosis and classification are heavily reliant on flow cytometry, immunohistochemistry, and cytogenetics, which are expensive and largely unavailable in most African countries, especially sub-Saharan Africa. Likewise, intensive cytotoxic chemotherapy regimens are often not tolerable in settings with limited supportive care. Delay in diagnosis and treatment of lymphoma leads to presentation with late symptoms of metastasis. It has been suggested that one of the early signs of metastasis is effusions in endothelial-lined sacs, such as pleural and pericardial effusions [20, 21].
Cardiac tamponade is a pericardial effusion in which the pressure from the accumulating fluid equalizes with intracardiac pressures, with subsequent impairment of ventricular filling and decreased cardiac output [12, 13]. The pericardium’s involvement is often the first manifestation of malignancy and may necessitate a further evaluation of occult cancer. This should be reserved for patients who present with persistent acute or recurrent pericarditis, unresponsiveness to anti-inflammatory therapy, concern for malignancy (e.g. weight loss), and new large pericardial effusion or cardiac tamponade.
Occult malignancies in patients initially presenting with a large pericardial effusion or cardiac tamponade are common. In a case series of 57 patients with a new large effusion, pericardial biopsy was found about 25% of undiagnosed malignancy patients [22]. In another report of 450 patients with acute pericardial disease, 7% of patients had a neoplastic cause with significant association with cardiac tamponade at presentation and lack of response to anti-inflammatory drugs [23]. In our review of 52 cases, most patients (80.8%) were diagnosed with lymphoma before hospital presentation and were considered to have secondary cardiac lymphoma (88.5%). Non-Hodgkin B-cell lymphoma was the most common type (42.9%).
In our review, patients mostly presented with dyspnoea (94.2%), oedema (35%), and constitutional symptoms (35%). Clinical presentation of cardiac tamponade usually depends upon how quickly fluid accumulates inside the pericardial sac [24]. Acute cardiac tamponade happens when there is a small but sudden life-threatening accumulation of fluid. In this scenario, the parietal pericardium fails to accommodate the increase in volume, and an acute rise in pericardial pressure ensues [12]. Subacute or haemodynamically insignificant pericardial effusion presents with no specific symptoms, but patients may still have symptoms related to the underlying cause (e.g. fever due to pericarditis). Subacute cardiac tamponade is a less dramatic process in which fluid accumulates slowly, and thus the pericardium can accommodate the growing volume [25]. Patients may be asymptomatic or complain of dyspnoea or fatigue. Cardiac tamponade is usually subacute in the setting of malignancy.
The initial workup for pericardial effusion includes an ECG, chest radiograph, and echocardiogram, with or without cross-sectional imaging of the chest as part of staging or restaging of malignancy [26]. Electrocardiography shows decreased QRS voltage and, occasionally, electrical alternans. Chest radiography (CXR) shows an enlarged cardiac silhouette with clear lung fields. CXRs are useful for detecting a concomitant pleural effusion. Echocardiography is warranted on suspicion of pericardial disease. It is necessary to detect the presence and estimate the pericardial effusion quantity and evaluate its haemodynamic impact on the heart. In the data from our study, about 65.4% of cardiac tamponade underwent a transthoracic echocardiogram, with the most common finding being pericardial effusion (82.4%) followed by right atrial mass or collapse (32.4%).
Determination of signs or symptoms suspicious for cardiac tamponade is critical in the case of effusion findings on echocardiography. Urgent pericardial drainage is recommended in the case of tamponade [27]. The most common therapeutic option that was offered to patients in our study was pericardiocentesis (63.5%), followed by pericardial window (15.4%). If there is no evidence of tamponade, pericardial fluid sampling or biopsy may still be needed to document the potential spread of malignant seeds to the pericardium. Cross-sectional imaging may help assess pericardial involvement and is necessary for staging lymphoma [28, 29].
Pericardiocentesis with cytologic and flow cytometric examination of the pericardial fluid is important if haemorrhagic effusion is present and if there is any reason to suspect malignancies [30]. The cytology’s sensitivity for diagnosing a malignant effusion is about 67% in lymphoma [31, 32]. Flow cytometry of pericardial fluid is critical in lymphoma patients [33, 34]. Pericardial biopsy or pericardioscopy may be required if cytology is negative and there is still high suspicion of malignancy [28, 29]. Cardiac catheterization can assess the haemodynamics of the right and left heart and the impact of pericardial disease upon cardiac filling and performance, particularly if echocardiography is inconclusive.
In terms of pericardial effusion therapeutic intervention, prolonged survival is the main target. Most patients presenting with a malignant pericardial effusion have a short life expectancy (median 2-4 months) [35–40]. However, the prognosis is better in haematological rather than solid tumours and in candidates for systemic chemotherapy [41, 42].
Generally, conservative observation is enough for asymptomatic or minimally symptomatic pericardial effusions. On the other hand, urgent fluid removal is warranted in highly symptomatic patients or those with evidence of haemodynamic compromise (tamponade) [5]. This is usually accomplished by percutaneous pericardiocentesis under echocardiographic guidance or by a pericardial window. Pericardiocentesis is an effective and rapid symptom in these patients, even if clinical or echocardiographic signs of cardiac tamponade persist.
Although pericardiocentesis initially relieves symptoms and improves haemodynamics, fluid accumulates in as many as 60% of cases [39, 43]. Recurrent accumulation can be managed by catheter drainage and by creating a permanent pericardial window allowing drainage of fluid into the pleural or peritoneal cavity. In multiple case series, catheter drainage relieved tamponade in 70-90% of cases [44–46]. In a case series, recurrent fluid accumulation was recorded in 30% of cases in 3 months of follow-up, while another series recorded a 13% rate of recurrent effusion with 1 year of follow-up [40, 47]. In a recent systematic review of 31 nonrandomized studies, any intervention other than isolated pericardiocentesis (38.3% recurrence rate) was associated with significantly lower recurrence rates. Pericardiocentesis with extended catheter drainage (486 patients) and balloon pericardiotomy (157 patients) showed recurrence rates of 12.1 and 10.3%, respectively.
Surgical decompression of the pericardium (e.g. pericardiotomy, pericardiostomy, and window pericardiectomy) is performed using various surgical techniques (e.g. open surgery, video-assisted thoracoscopy). While no randomized trials have been done to compare surgical and percutaneous drainage of pericardial effusions, retrospective studies demonstrated immediate haemodynamic benefit in almost all patients with minimal post-procedural morbidity and mortality [31, 40, 48, 49]. In the data reviewed in our study, only 7 patients required surgical resection (13.5%). A systematic review including data from 59 nonrandomised studies suggested a higher likelihood of successful control of effusion with surgical intervention as compared to a percutaneous approach [50]. However, the lack of randomized trials for this problem and likely selection bias in these reports limit the power of any recommendation.
Compared to patients known to have lymphoma before presenting with cardiac tamponade, only 10 patients were diagnosed with lymphoma after cardiac tamponade diagnosis. When assessing overall survival, tamponade timing either before or after lymphoma diagnosis was not a potential influencing factor.
Our study was limited by the scarcity of clinical trials, which necessitated the compiling of only case reports. Case reports are not generally representative of the population, because they usually represent outliers with no possibility of establishing cause-effect relationships and publication bias. Moreover, the low number of patients [10] in our study made it difficult to calculate the median survival of patients with lymphoma diagnosis after cardiac tamponade.
Conclusions
Our study of the published data demonstrates that most patients presented with pericardial tamponade after lymphoma diagnosis, and those were mostly secondary cardiac lymphoma of the non-Hodgkin type, with large B-cell as the most common subtype. Dyspnoea, oedema, and constitutional symptoms were the most common presenting signs. Most patients underwent echocardiography with subsequent pericardiocentesis. The median overall survival of patients with lymphoma and cardiac tamponade is 4 months, with no significant difference in mortality in the presentation timing before and after the diagnosis of lymphoma. Further, well-designed longitudinal studies are required to investigate the association between lymphoma and cardiac tamponade.