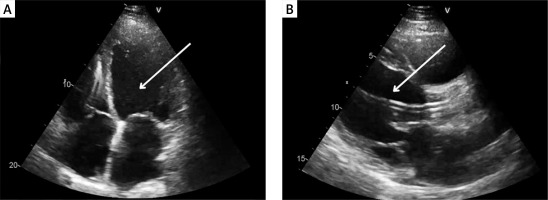
A 51-year-old male with a history of dilated cardiomyopathy, atrial fibrillation, diabetes and cardiac resynchronization therapy was admitted to the cardiology department due to another episode of decompensation of heart failure (HF). On admission, physical examination revealed peripheral oedema and abdominal pain. Blood investigations showed elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP) at 4333 pg/ml (norm 0–125 pg/ml). Echocardiography disclosed enlargement of all heart chambers, moderate mitral regurgitation and reduced left ventricular ejection fraction of 19% (Figure 1 A). Despite the standard HF treatment with loop diuretics, deterioration was observed with hypotension and an elevated lactate level of 4.1 mmol/l. The severity of cardiogenic shock was assessed as stage D in the Society for Cardiovascular Angiography and Intervention (SCAI) classification [1]. The patient required infusion of dobutamine and levosimendan. Persistent abdominal pain and increased aspartate transaminase (AST) at 198 U/l (norm < 35 U/l) and alanine transaminase (ALT) at 213 U/l (norm < 45 U/l), prompted a computed tomography scan revealing potential indicators of cholecystitis, which were subsequently confirmed through ultrasonography. The Heart Team (HT) decided on an urgent implantation of an Impella CP device, followed by a cholecystectomy, and subsequent qualification for long-term left ventricular assist device (LVAD) implantation. Impella CP was successfully implanted through the femoral artery. Four days later, an open cholecystectomy with a right subcostal Kocher incision was successfully performed. There was no necessity to modify the standard operation protocol. During the procedure, the patient was supported with dobutamine, noradrenaline and Impella CP set to P5 level. Postoperatively, inotropic agents were progressively reduced until complete discontinuation. Initially anticoagulation was conducted using unfractionated heparin under activated clotting time (ACT), however heparin-induced thrombocytopenia was detected. Heparin was subsequently switched to fondaparinux. The patient was reevaluated by the HT and qualified for LVAD therapy. Eight days after the cholecystectomy, the Impella CP was removed and a HeartMate 3 LVAD was implanted. The patient was discharged 14 days later. This case highlights the critical role of the Impella CP device in initial hemodynamic stabilization and possibility to provide temporary mechanical circulatory support (tMCS) during urgent surgical interventions, as demonstrated by Anderson et al. [2]. Furthermore, it underscores the importance of tMCS in managing cardiogenic shock prior to destination therapy such as LVAD therapy.
Journals
Advances in Dermatology and Allergology/Postępy Dermatologii i Alergologii
Advances in Interventional Cardiology/Postępy w Kardiologii Interwencyjnej
Anaesthesiology Intensive Therapy
Archives of Medical Science
Biology of Sport
Central European Journal of Immunology
Folia Neuropathologica
Forum Ortodontyczne / Orthodontic Forum
Journal of Contemporary Brachytherapy
Pediatric Endocrinology Diabetes and Metabolism
Pielęgniarstwo Chirurgiczne i Angiologiczne/Surgical and Vascular Nursing
Polish Journal of Pathology
Prenatal Cardiology