A patient (60-year old man) with previously diagnosed multivessel coronary disease and a reduced left ejection fraction (LVEF = 26%) was scheduled for assessment of left main artery stenosis (LM). The previous study revealed a chronic total occlusion of the left descending coronary artery and the right coronary artery. Two months previously the patient had received a drug-eluting stent to the medial segment of the circumflex artery (Cx).
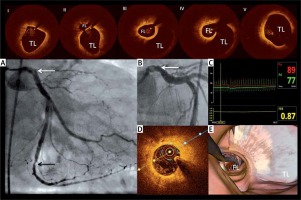
The second diagnostic angiogram presented a tandem lesion including the distal LM and the distal Cx stenoses. After the initial problems with the crossing of the LM stenosis, fractional flow reserve (FFR) wire was advanced to the distal part of the Cx. The intracoronary administration of adenosine with doses up to 200 μg revealed an FFR value of 0.87 (Figure 1). Given the difficulties with navigating through the distal LM with FFR wire, the optical coherence tomography (OCT) imaging was performed. It showed a chronic dissection of the distal LM. Both the OCT probe and FFR wire passed through the false lumen (Figure 1). The wire was repositioned to the true lumen, and the zotarolimus-eluting stent (4.5 × 26 mm) was successfully implanted in the LM/Cx.
Figure 1
Chronic dissection of the non-ischemic distal left main lesion. I – Cross-sectional optical coherence tomography (OCT) images presenting proximal left main. II – the proximal entry to the dissection. III – the OCT probe within the false lumen (FL) of dissection and presentation of the true visible lumen (TR). IV – the distal entry to the dissection. V – the distal left main; true lumen (TL). A and B the diagnostic angiogram presenting the tandem lesion in the distal left main and distal circumflex artery. The white arrow indicates the observed haziness in the left main. The black arrow indicates the distal lesion. C – FFR assessment after 200 μg of adenosine, D – OCT cross-sectional image of the fibrous lesion in the distal segment of circumflex artery. E – Three-dimensional reconstruction of the observed dissection presenting FFR wire in FL
The chronic LM dissection was probably caused by the guiding catheter during the intervention in the circumflex artery performed two months ago. This LM dissection was not diagnosed during the standard angiography, and FFR results indicated a non-invasive approach. Only such combined OCT-FFR assessment of the left main lesion provided the correct picture of the disease and led to LM stenting. It was against the current guidelines on myocardial revascularization, which do not recommend stenting of lesions with FFR > 0.80. Nevertheless, as this case showed, some non-ischemic lesions may still put the patient at risk of adverse events. Therefore, the assessment of ambiguous lesions by combined functional and morphological assessment has a strong rationale. All available tools such as FFR, the instantaneous wave-free ratio (iFR), OCT and intravascular imaging ultrasound (IVUS) may help to reduce the diagnostic uncertainty of coronary lesions.








