Introduction
Mortality during the acute phase of myocardial infarction (MI) has steadily decreased over the past 3 decades [1, 2]. The main impact of MI is shifting from acute mortality to adverse remodeling, chronic left ventricle (LV) dysfunction and eventually clinically apparent heart failure [1, 3]. Occurrence of adverse remodeling increases long-term mortality after MI [4]. Several biomarkers are screened in order to identify patients who are at risk of LV remodeling development. Biomarker testing is a very attractive idea, since it is non-invasive, not operator-dependent and widely available. However, because of the complex pathophysiology of remodeling, selecting one ideal marker is challenging.
The aim of this narrative review was to assess and discuss data about circulating biomarkers of remodeling in patients after MI.
Data assessment
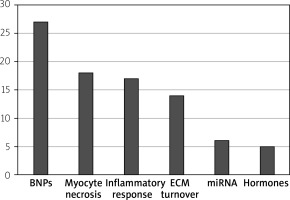
We performed a Medline search of articles published in the years 2005–2020 using the keywords: “myocardial infarction AND ventricular remodeling AND biomarkers”. We examined original studies of patients, admitted with acute MI, reporting measurement of ≥ 1 circulating biomarker. Articles with a follow-up of LV imaging and presenting LV volumes as an indicator of remodeling were analyzed. Studies with sample size of less than 30 patients and with follow-up of < 1 month were excluded. Finally, we selected and assessed 53 studies, which examined 160 relations between biomarkers and remodeling. In Table I we present details about examined publications. Main groups of assessed biomarkers included: B-type natriuretic peptides (BNPs); markers of cardiomyocyte injury and necrosis (troponin, creatinine kinase); markers of inflammatory response including C-reactive protein (CRP), white blood count (WBC), soluble ST2 and galetctin-3; markers of extracellular matrix turnover including matrix metalloproteinases (MMPs), tissue inhibitors of matrix metalloproteinases (TIMPs) and collagen propeptides; microRNAs and hormones (aldosterone, cortisol, norepinephrine, copeptin) (Figure 1).
Table I
Studies of circulating biomarkers associated with left ventricle adverse remodeling after myocardial infarction in chronological order of publication date
| Article details | Biomarkers | Patient no. main incl. criteria | LVAR assessment method | LVAR definition | Time of serum collection | LVAR evaluation time | Correlationwith LVAR |
|---|---|---|---|---|---|---|---|
| Jirmar et al. Int Heart J 2005 [22] | PIIINP PICP | 35 STEMI PCI | Echocardiography | LVEDV | Admission, day 2, 4, 7, 1 month | Day 1, 4, 1, 6 months | Positive Positive |
| Matsunaga et al. Int J Cardiol 2005 [23] | MMP-2 + MMP-9 | 52 STEMI PCI | Echocardiography | LVEDVI LVESVI | Week 2 | Admission, week 2, 6 months | Positive |
| Wagner et al. J Card Fail 2006 [24] | MMP-9 | 109 STEMI PCI | Echocardiography Ventriculography | LVEDV LVESV | Admission | Admission, 6 months | Positive |
| Hirayama et al. Am J Cardiol 2006 [25] | BNP | 106 First anterior MI PCI | Ventriculography | LVEDV | 1, 6 months | 1, 6 months | Positive |
| Webb et al. Circulation 2006 [26] | MMP-9 Other biomarkers: MMP-2 MMP-7 MMP-8 TIMP-1 TIMP-2 | 32 STEMI NSTEMI | Echocardiography | LVEDV | Day 1, 2–5, 1, 3, 6 months | Day 1, 5, 1, 3, 6 months | Positive Not associated Not associated Not associated Not associated Not associated |
| Orn et al. J Card Fail 2007 [27] | MMP-2 MMP-9 NT-proBNP | 52 STEMI NSTEMI PCI Fibrinolysis | CMR | LVEDVI | Admission, 1 month, 1, 4 years | 4 years | Not associated Positive Positive |
| Kelly et al. Eur Heart J 2008 [28] | TIMP-1 MMP-9 NT-proBNP | 404 STEMI NSTEMI Fibrinolyis Conservative | Echocardiography | LVEDV LVESV | Day 1, discharge | Discharge, 6 months | Positive Positive Positive |
| Kelly et al. J Card Fail 2008 [29] | Copeptin | 274 STEMI NSTEMI PCI Fibrinolysis | Echocardiography | LVEDV LVESV | Discharge | Discharge, mean of 155 days | Positive |
| Kuribara et al. J Cardiol 2009 [30] | DNaseI | 45 STEMI NSTEMI PCI | Echocardiography | LVEDV LVESV | Admission, day 2, 3, 7, 14, 6 months | Admission, 6 months | Positive |
| Garcia-Alvarez et al. Am J Cardiol 2009 [31] | BNP | 82 STEMI PCI Fibrinolysis | Echocardiography CMR | > 20% increase in LVEDV | Day 4, 1, 6 months | 6 months | Positive |
| Weir et al. Eur J Heart Fail 2009 [32] | Apelin Other biomarkers: NT-proBNP Norepinephrine | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVEDVI LVESVI | Day 2, 6 months | Discharge, 6 months | Not associated Positive Positive |
| Fertin et al. Am J Cardiol 2010 [33] | BNP TnI CRP | 246 First anterior Q-wave MI PCI Fibrinolysis | Echocardiography | > 20% increase in LVEDV | Discharge, 1, 3, 12 months | Discharge, 3, 12 months | Positive Positive Not associated |
| Weir et al. Cytokine 2010 [34] | MCP-1 | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVESVI | Day 2, 3, 6 months | Day 2, 3, 6 months | Negative |
| Weir et al. J Am Coll Cardiol 2010 [35] | ST2 protein Other biomarkers: NT-proBNP Aldosterone Norepinephrine | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVEDVI LVESVI | Admission, 3, 6 months | Admission, 3, 6 months | Positive Positive Positive Positive |
| Weir et al. J Thromb Thrombolysis 2010 [36] | t-PA vWF MMP-2 MMP-3 MMP-9 BNP | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVESVI | Day 2, 3, 6 months | Day 2, 3, 6 months | Positive Positive Not associated Positive Not associated Positive |
| Kelly et al. Biomarkers 2010 [37] | Procalcitonin | 273 STEMI NSTEMI Fibrinolysis Conservative | Echocardiography | LVEDV LVESV | Discharge | Discharge, 4 months | Positive |
| Hallén et al. Heart 2010 [38] | TnI | 132 STEMI PCI | CMR | LVEDVI LVESVI | Day 1, 2 | Day 5, 4 months | Positive |
| Lamblin et al. Eur J Heart Fail 2011 [39] | Hepatocyte growth factor | 246 First anterior Q-wave MI PCI Fibrinolysis | Echocardiography | LVEDV LVESV | Discharge, 1, 3, 12 months | Discharge, 3, 12 months | Positive |
| Weir et al. Eur J Heart Fail 2011 [40] | Aldosterone Cortisol metabolites | 50 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVESVI | Admission | Admission, 6 months | Positive Positive |
| Dominguez-Rodriguez et al. Am J Cardiol 2011 [41] | GDF15 Other biomarkers: TnI BNP | 97 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Day 1 | First 4 days, 12 months | Positive Not associated Not associated |
| Aoki et al. J Cardiol 2011 [42] | Peak PBMC FPG Peak WBC Peak monocyte | 131 STEMI PCI | Ventriculography | > 10% increase in LVEDVI | Day 1–5 | Admission, 6 months | Positive Positive Positive Positive |
| Erkol et al. Atherosclerosis 2012 [43] | Osteoprotegerin Other biomarkers: Peak TnI | 92 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Admission | Day 1, 6 months | Positive Positive |
| Wyderka et al. Mediators Inflamm 2012 [44] | CD34+/CXCR4+ | 50 STEMI PCI | Echocardiography | LVEF | Admission, 12 months | Admission, 12 months | Negative |
| Devaux et al. J Card Fail 2012 [45] | VEGFB | 290 STEMI PCI | Echocardiography | LVEDV | Day 4 | Discharge, 6 months | Negative |
| Fertin et al. J Cardiol 2012 [46] | sFas ligand Other biomarkers: BNP | 246 First anterior Q-wave MI PCI Fibrinolysis | Echocardiography | LVEDV LVESV | 1 month | Discharge, 3, 12 months | Not associated Positive |
| Urbano-Moral et al. Heart 2012 [47] | NT-proBNP TnT hsCRP MMP-9 PINP | 112 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Discharge | Discharge, 6 months | Positive Positive Positive Positive Not associated |
| Weir et al. Cytokine 2012 [48] | IL-21 Other biomarkers: MMP-2 MMP-3 MMP-9 TIMP-1 TIMP-2 TIMP-4 MCP-1 BNP | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVESVI LVEDVI | Admission, 6 months | Admission, 6 months | Positive Not associated Positive Negative Negative Positive Positive Positive Positive |
| Devaux et al. Cir Cardiovasc Genet 2013 [49] | miR-150 | 90 First STEMI Fibrinolysis Conservative | Echocardiography | LVEDV | Day 3–4 | Discharge, 6 months | Negative |
| Bauters et al. Int J Cardiol 2013 [50] | miR-133a miR-423-5p | 246 Anterior Q-wave MI PCI Fibrinolysis | Echocardiography | LVEDV | Admission, 1, 3, 12 months | Discharge, 3, 12 months | Not associated Not associated |
| Mather et al. Int J Cardiol 2013 [51] | hsCRP TnI NT-proBNP H-FABP | 48 First STEMI PCI | CMR | LVEDVI LVESVI | Day 2, 1 week, 1, 3 months | Day 2, 1 week, 1, 3 months | Positive Positive Positive Not associated |
| Meng et al. Postgrad Med J 2013 [52] | Catestatin Other biomarkers: BNP | 31 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Admission, day 3, 7, 3 months | Week 1, 3 months | Positive Positive |
| Weir et al. Circ Heart Fail 2013 [53] | Galectin 3 | 100 LVEF < 40% STEMI NSTEMI PCI Fibrinolysis | CMR | LVESVI | Admission, 6 months | Admission, 6 months | Not associated |
| Eschalier et al. Circ Heart Fail 2013 [54] | PINP PIIINP PICP Other biomarkers: BNP TnI CRP | 246 First anterior Q-wave MI PCI Fibrinolysis | Echocardiography | > 20% increase in LVEDV | 1 month | Discharge, 12 months | Not associated Not associated Positive Positive Positive Not associated |
| Reinstadler et al. Heart 2013 [55] | Copeptin | 54 STEMI PCI | CMR | LVEDV LVESV | Day 2 | Admission, 4 months | Positive |
| Kleczynski et al. Dis Markers 2013 [56] | NT-proBNP | 45 STEMI PCI | CMR | LVEDV LVESV | Admission, 6 months | 6 months | Positive |
| Fertin et al. PLoS One 2013 [57] | MMP-1 MMP-2 MMP-3 MMP-8 MMP-9 MMP-13 TIMP1 TIMP-2 TIMP-3 TIMP-4 | 246 First anterior MI PCI Fibrinolysis | Echocardiography | > 20% increase in LVEDV | Admission, 3 months, 1 year | Discharge, 1, 3, months, 1 year | Not associated Not associated Not associated Not associated Positive Positive Not associated Not associated Not associated Not associated |
| Lv et al. Int J Mol Sci 2014 [58] | miR-208b miR-34a Other biomarkers: TnT Peak CK BNP | 359 PCI Fibrinolysis | Echocardiography | > 10% increase in LVEDV | Admission | Baseline, 6 months | Positive Positive Positive Not associated Positive |
| Kumarswamy et al. Circ Res 2014 [59] | Mitochondrial long noncoding RNA uc022bqs.1 | 246 First anterior Q-wave MI PCI Fibrinolysis | Echocardiography | > 20% increase in LVEDV | Day 3–7, 1, 3, 12 months | Day 3–7, 3, 12 months | Positive |
| Manhenke et al. Eur Heart J 2014 [60] | PINP MMP-2 MMP-3 Other biomarkers: TnT hsCRP NT-proBNP | 42 First STEMI PCI | CMR | LVEDVI LVSVI | Admission, day 2, 7, 2, 12 months | Day 2, 7, 2, 12 months | Negative Negative Positive Positive Positive Positive |
| Liu et al. Cardiology 2015 [61] | miR-146a miR-21 Other biomarkers: NT-proBNP CRP TnI CK-MB | 198 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Admission | Day 5, 1 year | Positive Positive Positive Positive Not associated Positive |
| Abdel Hamid et al. J Interv Cardiol 2016 [62] | Circulating endothelial cells | 78 PCI Fibrinolysis | Echocardiography | > 20% increase in LVEDV | Day 1 | Day 2, 1 month | Positive |
| Türkoğlu et al. Coron Artery Dis 2016 [63] | M30 antigen M60 antigen Other biomarkers: BNP | 255 STEMI PCI | Echocardiography | > 20% increase in LVEDV | Day 1 | Day 1, 6 months | Positive Positive Positive |
| Reindl et al. Heart 2017 [64] | FGF 23 Other biomarkers: cTnT hsCRP NTproBNP | 88 STEMI PCI | CMR | > 20% increase in LVEDV | Day 2 | Day 2, 4 months | Positive Positive Positive Positive |
| Grabmaier et al. Int J Cardiol 2017 [65] | miR-1 miR-29b miR-21 | 44 STEMI PCI | CMR | LVEDV | Day 4, 9, 6 months | Day 4, 6 months | Not associated Negative Not associated |
| Hendriks et al. Int J Cardiovasc Imaging 2017 [66] | Peak CK Peak CK-MB Peak TnT NT-proBNp | 271 First STEMI PCI | CMR | LVEDVI LVESVI | Admission, week 2, 6 | 4 months | Positive Positive Positive Positive |
| Hsu et al. Int J Med Sci 2017 [67] | BNP decrease ratio Peak CK-MB Peak TnI CRP | 97 STEMI NSTEMI PCI | Echocardiography | > 20% increase in LVEDV | Day 2, 7, 3 months | Day 2, 7, 3 months | Negative Positive Not associated Not associated |
| Di Tano et al. Heart 2017 [68] | Galectin 3 Other biomarkers: NT-proBNP | 103 First STEMI LAD culprit PCI | Echocardiography | > 15% increase in LVESV | Day 2, 1, 6 months | Day 2, 1, 6 months | Positive Not associated |
| Miñana et al. Int J Cardiol 2018 [69] | ST2 protein Other biomarkers: TnT NT-proBNP | 109 First STEMI PCI | CMR | LVEDVI LVESVI | Day 1 | 1 week, 6 months | Positive Not associated Not associated |
| de Gonzalo-Calvo et al. Sci Rep 2018 [70] | miR-1254 | 70 First STEMI PCI | CMR | LVESVI | Admission | Week 1, 6 months | Negative |
| Orrem et al. Int J Cardiol 2018 [71] | IL-1Ra sIL-1RAcP sIL-1R2 sIL1-R1 Other biomarkers: Peak TnT Peak CRP NTproBNP | 320 STEMI PCI | CMR | LVEDVI LVESVI | Admission, day 1, 4, 12 months | Day 2, 4 months | Not associated Not associated Positive Not associated Positive Positive Not associated |
| Padoan et al. Int J Cardiol 2019 [72] | Vitamin D Other biomarkers: CRP Peak TnI | 253 STEMI NSTEMI PCI CABG | Echocardiography | > 15% increase in LVESV | During hospitalization | During hospitalization, 4 months | Negative Positive Positive |
| Garcia et al. Int J Mol Sci 2019 [73] | Peak CK TnI NT-proBNP CRP WBC Neutrophil count Creatinine | 64 STEMI PCI Fibrinolysis | CMR | > 10% increase in LVESV | Day 2 | Admission, 3, 12 months | Positive Not associated Not associated Positive Positive Positive Not associated |
| Reindl et al. Eur Heart J Acute Cardiovasc Care 2019 [74] | TSH Other biomarkers: Peak TnT Peak CRP | 102 STEMI PCI | CMR | > 20% increase in LVEDV | Day 1, 4 months | Week 1, 4 months | Negative Positive Positive |
[i] PIIINP – type III procollagen propeptide, PICP – carboxy terminal propeptide of type I collagen, MMP – matrix metalloproteinases, BNP – B-type natriuretic peptide, TIMP – tissue inhibitor of MMP, Tn – troponin, CRP – C reactive protein, MCP – monocyte chemoattractant protein, tPA – tissue plasminogen activator, vWF – von Willebrand Factor, GDF – growth differentiating factor, PBMC – peripheral blood mononuclear count, FPG – fasting plasma glucose, WBC – white blood count, VEGFB – vascular endothelial growth factor B, PINP – procollagen type I amino terminal propeptide, Il – interleukin, miR – micro RNA, HFABP – heart type fatty acid binding protein, CK – creatinine kinase, FGF – fibroblast growth factor, TSH – thyroid stimulating hormone, Incl – inclusion, MI – myocardial infarction, STEMI – ST elevation MI, NSTEMI – non-ST elevation MI, PCI – percutaneous coronary intervention, LAD – left anterior descending, LVEF – left ventricle ejection fraction, LVAR – left ventricular adverse remodeling, CMR – cardiac magnetic resonance, LVEDV(i) – left ventricle end diastolic volume (index), LVESV(i) – left ventricle end systolic volume (index).
Figure 1
Groups of most commonly assessed biomarkers. Data are shown as number of studies evaluating groups of biomarkers
BNP – B type natriuretic peptide, ECM – extracellular matrix.
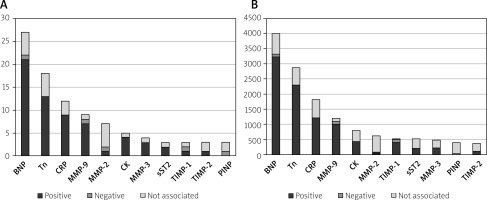
A positive correlation between examined biomarkers and remodeling was found in 101 (63%), a negative correlation was found in 13 (8%) and no significant association was found in 46 (29%) cases. Figure 2 presents the relationships between the most common individual biomarkers and remodeling. BNPs, troponin, CRP and creatinine kinase were the most frequent biomarkers and they were positively correlated with remodeling. MMP-9 was the most commonly analyzed member of metalloproteinases. It occurred in 9 studies and in 7 a positive correlation with remodeling was reported. MMP-2 was assessed in 7 studies, but in 5 reports no significant association with remodeling was found. MMP-3 was analyzed in 4 studies and in 3 it was positively correlated with remodeling. Less frequent biomarkers included soluble ST2, TIMPs and procollagen type I amino terminal propeptide (PINP).
Figure 2
Relationships between individual biomarkers and remodeling. A – Data are shown as number of studies evaluating specific biomarkers. B – Data are shown as number of patients enrolled in studies evaluating biomarkers
BNP – B type natriuretic peptide, Tn – troponin, CRP – C reactive protein, MMP – matrix metalloproteinase, CK – creatinine kinase, TIMP – tissue inhibitor of MMP, PINP – procollagen type I amino terminal propeptide.
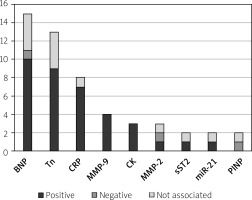
The majority of presented studies (68%) included ST-elevation MI (STEMI) patients exclusively. In most studies (57%) patients were treated with primary percutaneous coronary intervention (PCI). In 38% of studies patients underwent PCI and fibrinolysis and in 5% of studies patients underwent fibrinolysis or conservative treatment only. In Figure 3 we show the most commonly assessed biomarkers in patients treated exclusively with primary PCI. We observed that TIMPs were less frequently and microRNA-21 was relatively more frequently assessed in studies which included patients treated exclusively with primary PCI.
Figure 3
Relationships between individual biomarkers and remodeling in patients treated exclusively with primary percutaneous coronary intervention. Data are shown as number of studies evaluating specific biomarkers
BNP – B type natriuretic peptide, Tn – troponin, CRP – C reactive protein, MMP – matrix metalloproteinase, CK – creatinine kinase, miR – microRNA, PINP – procollagen type I amino terminal propeptide.
In the presented articles remodeling was defined as an increase in LV end diastolic volume (LVEDV) or less often LV end systolic volume (LVESV) during follow-up. Twenty (38%) studies utilized specific cut-off values for LV volume increase. Most commonly it was a 20% increase in LVEDV. Echocardiography and cardiac magnetic resonance (CMR) were the most common methods of remodeling assessment. Echocardiography was used in 57% and CMR was used in 41% of studies. In more recent studies, from the years 2015–2019, CMR was used in 57% of cases and echocardiography in 43%. Time points of LVAR assessment differed vastly among analyzed papers. The shortest period of LVAR evaluation after MI was 1 month (1 study), the longest was 4 years (also in 1 study). The most frequent time point for LVAR assessment was 6 months (73% of studies).
Description of biomarkers
The present analysis shows that a relatively large number of circulating biomarkers were tested, which reflects the complex pathophysiology of remodeling. Main groups of assessed biomarkers included BNPs, markers of cardiomyocyte injury and necrosis, markers of inflammatory response, markers of extracellular matrix turnover and microRNAs.
B-type natriuretic peptides
BNP is secreted predominantly from heart ventricles. It is a marker of volume overload and high filling pressure. In response to myocardial wall stretch, pre-proBNP is synthesized and processed to proBNP, which is further processed to the biologically inactive N-terminal prohormone fragment (NT-proBNP) and biologically active BNP [5]. Biological effects of BNP include diuresis, natriuresis, vasodilatation and inhibition of the renin-angiotensin system. BNP is an established biomarker of LV systolic dysfunction and heart failure progression [6]. Higher BNP concentrations in patients after MI were reported to predict long-term mortality [6]. According to ESC guidelines BNP and NT-proBNP provide prognostic information regarding the risk of death and acute heart failure in MI patients [7]. Although the cut-off values are different for BNP and NT-proBNP, the guidelines give no indication which marker presents better accuracy for heart failure [7]. In the present analysis NT-proBNP was analyzed in 13 studies and BNP was assessed in 14 reports. Both markers were positively correlated with remodeling.
Cardiac troponins
The cardiac troponin complex consists of 3 subunits: troponin C, troponin T and troponin I. Troponin I and T form an actin-myosin complex and are released into peripheral blood after myocyte injury. Elevated concentration of troponin I and T is a diagnostic marker of acute coronary syndromes. Peak levels of both troponin I and T are predictive for mortality, recurrent MI and newly developed post-MI heart failure. Early troponin measurement provides an estimate of infarct size [5]. Although both troponins present comparable diagnostic accuracy for MI, troponin T provides greater prognostic value [7]. Currently, high sensitivity (hs) troponin assays are recommended for diagnosis and prognosis of MI instead of conventional assays. In the present analysis troponin I was examined in 10 studies and troponin T was assessed in 8 studies. Both troponins were positively correlated with remodeling.
Markers of inflammatory response
C-reactive protein is an acute phase protein of hepatic origin. Myocardial ischemia is associated with the systemic inflammatory response with increased production of acute phase proteins including CRP, partly as a response to stimulation by interleukin-6, which is released from the infarct zone. Levels of CRP increase in the first hours of MI and peak approximately at day 2. Elevated CRP concentrations are associated with adverse clinical outcome after MI, larger infarct size, microvascular obstruction and higher mortality in patients with heart failure [8]. In the present analysis CRP was assessed in 12 publications. In 9 studies, it was positively correlated with remodeling. Several studies assessed high-sensitivity (hs) CRP, which was also positively associated with remodeling.
Soluble suppression of tumorigenicity-2 (sST2) is the soluble form of interleukin-1 receptor-like 1 and is a protein biomarker of cardiac stress. Serum levels of sST2 were reported to be higher in patients with heart failure. In patients with MI, higher concentrations of sST2 predicted mortality and occurrence of post-MI heart failure [5]. In the present analysis sST2 was assessed in 3 studies and in 2 it was positively correlated with remodeling.
Extracellular matrix turnover
Extracellular matrix (ECM) surrounds cardiomyocytes and forms a scaffold which maintains the LV shape and geometry. ECM rearrangement corresponds to a balance between degradation and synthesis of extracellular components, regulated by MMPs and TIMPs [9]. MMPs are members of zinc-dependent endopeptidases, which degrade several ECM proteins and thus modulate physiological and pathological processes including MI and congestive heart failure. MMPs consist of 25 enzymes which are endogenously inhibited by TIMPs, a family comprising 4 members (TIMP-1, -2, - 3 and -4) [10]. The ECM turnover during remodeling is regulated through the balance of MMPs and TIMPs, levels of both of which rise after MI. In the present analysis MMP-9 was the most frequent analyzed member of MMPs. It was assessed in 9 studies and in 7 a positive correlation with remodeling was reported. The second most commonly assessed biomarker from this group was MMP-3, which appeared in 4 studies and in 3 a positive correlation with remodeling was observed. The relationship between levels of TIMPs and remodeling was inconclusive in the present analysis.
Collagen synthesis begins in fibroblasts which produce procollagen. In the ECM, the amino-terminal and carboxy-terminal propeptides are separated by endopeptidases and released into the circulation. They can be used as markers of collagen synthesis. Collagen type I and III are principal structural proteins found in the myocardium. PINP is a marker of type I collagen synthesis. It was reported to be associated with reverse remodeling and inversely correlated with LV volumes in patients undergoing resynchronization therapy [11]. In the present analysis PINP was assessed in 3 studies and in 1 it was negatively correlated with remodeling. In 2 studies, no significant association with remodeling was reported.
MicroRNAs
MicroRNAs are small noncoding RNA molecules with regulatory functions. They participate in various cardiovascular processes through post-transcriptional regulation of gene expression. MicroRNAs are related to the regulation of cardiomyocyte apoptosis and fibrosis [12]. In the present analysis microRNAs were tested in 6 studies; however, the most frequently assessed microRNA-21 appeared only in 2 studies and in 1 analysis a positive correlation with remodeling was reported; thus selecting a biomarker of remodeling from the microRNA family is limited.
Methods and time points of remodeling assessment
Remodeling is defined as molecular, cellular and interstitial changes resulting from myocardial ischemia [13]. Clinical assessment of LV remodeling is based on detection of increase of LV volumes. In the present analysis the most common cut-off value was a 20% increase in LVEDV. Cardiac magnetic resonance is considered to be a gold standard for remodeling assessment due to accurate and reproducible measurements of LV volumes [14]. CMR is a more precise method with reduced operator variability compared to echocardiography. In addition, CMR with late gadolinium enhancement has the ability to distinguish between reversible and irreversible myocardial injury. CMR may also provide more precise information about scar formation, transmural necrosis and microvascular obstruction [15–18]. In the present analysis the rate of studies utilizing CMR was 41% and increased in more recent publications. Despite this, echocardiography remains the fastest and most accessible method which is used not only in clinical practice but also in clinical trials. Transthoracic echocardiography is also recommended in all patients with acute MI to evaluate global and regional function of LV [7].
Remodeling is a time-dependent process, which can continue up to 6–12 months after MI with infarct extension occurring in weeks to months after reperfusion [19]. Earlier assessment might not reflect the full remodeling process. A frequently selected time point for remodeling evaluation is 6 months after MI. Time points of blood collection are also vital. In several analyzed studies, serial blood sampling during index hospitalization and follow-up was utilized, which is helpful in determining the strongest association with remodeling. However, we think that the most clinically useful is the relationship between remodeling and levels of biomarkers measured in the acute phase of MI. Nowadays, biomarker guided therapy in patients after MI is not a standard approach. On the other hand, identification of high risk individuals could allow implementation of follow-up with more frequent LV assessment after hospital discharge.
Future directions
Association of classic biomarkers including BNPs, cardiac troponin and CRP with post-MI remodeling is widely documented. These biomarkers are readily available, routinely assessed in MI patients and their measurement is relatively inexpensive. In the present analysis MMP-9 was frequently examined and positively correlated with remodeling. However, measurement of MMP-9 activity is challenging due to its complex in vivo regulation. MMPs are synthesized as inactive zymogens, and must be enzymatically activated by hydrolyzation of a propeptide domain. Their activity is further regulated by TIMPs. Typical methods such as western blot, ELISA or immunohistochemistry are reported to be not sufficient to accurately describe MMPs’ in vivo activity [20]. The ideal biomarker should not only allow improvement of clinical decisions but also be easily detectable from blood. The main idea of biomarker testing is their wide availability and no inter/intra-operator variability. The present analysis shows that a relatively large number of different biomarkers were assessed. Due to the complex pathophysiology of remodeling, selecting one marker is challenging. What is more, several biomarkers including MMPs, TIMPs and microRNAs occur in many types; thus despite being tested in a relatively large amount of studies, individual biomarkers appeared in a limited number of reports. Perhaps at a recent stage of studies, single biomarker testing might be not sufficient for remodeling prediction. A combination of biomarkers from different groups, reflecting different pathways of remodeling, might be appropriate. Reinstadler et al. showed that combined biomarker testing including NT-proBNP, troponin T, CRP, lactate dehydrogenase and liver transaminases improved the predictive value for remodeling compared to single biomarker assessment [21].







