Summary
This is the first study to compare the efficacy of antazoline with propafenone versus electrical cardioversion in restoring and maintaining sinus rhythm at discharge in patients who developed atrial fibrillation during pulmonary vein cryoablation. This research showed that in atrial fibrillation during the cryoablation procedure electrical cardioversion appears to be more effective in restoring sinus rhythm than antazoline with propafenone in the general atrial fibrillation patient population, especially in patients with persistent atrial fibrillation.
Introduction
Atrial fibrillation (AF) is the most common supraventricular arrhythmia – affecting over 33 million people, with an ever-increasing number of patients worldwide [1]. Its treatment should be characterized by an integrated and holistic approach to the patient. Anticoagulants are used to prevent ischemic stroke. Better symptom control can be achieved by controlling the ventricular rate. This could be achieved by different treatment modalities – electrical cardioversion, antiarrhythmic drugs, and percutaneous ablation. Catheter ablation is a minimally invasive procedure with the highest effectiveness in treating heart rhythm disorders [2]. During all AF catheter-ablation procedures pulmonary vein isolation (PVI) is recommended; it can be achieved with radiofrequency (RF) ablation or balloon cryoablation. AF catheter ablation for PVI is recommended for rhythm control after one failed or intolerant class I or III antiarrhythmic drug (AAD), to improve symptoms of AF recurrences in patients with: paroxysmal AF, or persistent AF without major risk factors for AF recurrence, or persistent AF with major risk factors for AF recurrence. Furthermore, AF catheter ablation is recommended to reverse left ventricle dysfunction in AF patients when tachycardia-induced cardiomyopathy is highly probable, independent of their symptom status as first-line therapy [3]. Cryoablation appears to be a more favorable alternative to the traditional RF approach. Compared with RF ablation, it has a lower risk of accidental catheter displacement during energy application, and it also provides a lower risk of endocardial surface damage and thrombus formation, therefore reducing the risk of cerebral embolism [4, 5]. The standard refrigerant used in this method is nitrous oxide – the gas is expanded through a porous baffle during the phase transition from a liquid state, resulting in significant cooling and very low temperatures, which are then applied to the heart tissues, causing their necrosis and the intended therapeutic effect [6]. Cryoablation is primarily used to treat paroxysmal AF when the sources of the arrhythmia are focally located in the pulmonary vein region of the left atrium (LA) [7]; however, it is also proven to be safe and effective treatment of persistent AF, which is accompanied by complex underlying mechanisms such as progressive electrical, structural remodeling and fibrosis of the atrial myocardium [8]. The pulmonary vein isolation (PVI) procedure may induce AF, and hence affect its assessment; therefore it generally requires subsequent electrical or pharmacological cardioversion [9]. Transthoracic synchronized CVE is well known as the treatment of choice in immediate termination of AF and restoring sinus rhythm among hemodynamically unstable patients and it is more effective than pharmacological cardioversion despite the requirement of sedation. However, in stable patients pharmacological or electrical cardioversion can be applied [10, 11]. The standard drugs used for pharmacological cardioversion are group IA, IC and III AAD: flecainide, ibutilide, dofetilide, propafenone and amiodarone. Beta adrenergic drugs are not used because of their low efficacy as sole agents. Vernakalant is also used to quickly restore sinus rhythm in rapid PVC [12, 13]. Propafenone is classified as a class Ic AAD, demonstrating active blockade of sodium channels. In addition, it has β-adrenergic receptor antagonist properties and shows weak activity as a calcium channel antagonist [14]. It is used for the adjuvant treatment and prophylaxis of supraventricular arrhythmias, especially in patients with symptomatic AF, and less commonly in ventricular arrhythmias. It is not used in patients with organic heart disease or in hypertensive patients without evidence of left ventricular hypertrophy. In recent years, there has been increased interest in antazoline as a drug used for pharmacological cardioversion. Antazoline is a first-generation antihistamine with additional anticholinergic and antiarrhythmic effects [15]. Its action results from prolonging the duration of the action potential, lowering its amplitude, and decreasing the excitability of cardiac tissue. It also decreases atrial conduction velocity, prolongs atrial refractory time, and may improve atrioventricular conduction [16]. Antazoline has a proven high efficacy of restoring sinus rhythm in emergency department patients comparable to other AAD [17]. Furthermore, it appears to be a suitable choice for safe termination of AF induced during a PVI procedure [16].
Aim
The aim of the research was to compare the efficacy of antazoline with propafenone and electrical cardioversion in restoring and maintaining sinus rhythm at discharge in patients with AF during cryoablation, with special regard to patients with paroxysmal AF.
Material and methods
Owing to the observational and retrospective nature of this study, neither patient’s consent nor ethics committee approval was required.
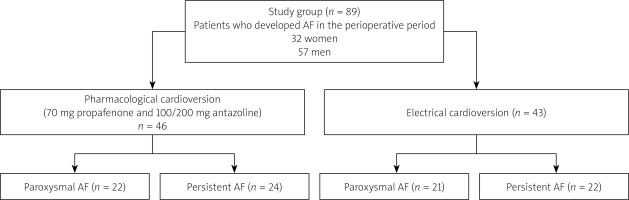
This study retrospectively analyzed 196 patients (mean age: 62.4 years old) who underwent elective cryoablation between September 2018 and May 2021 at American Heart of Poland in Tychy and Dąbrowa Górnicza. Eighty-nine (45.4%) patients who developed AF in the perioperative period (and it was not terminated by PVI) were selected as a study group. It consisted of 32 (40%) women and 57 (64.1%) men. Based on the method of sinus rhythm restoration the study group was divided into two groups – 46 (51.7%) patients were given pharmacological cardioversion with 70 mg of propafenone and 100 or 200 mg of antazoline, whereas the other 43 (48.3%) patients underwent ECV. This study has a retrospective registry design. The decision to perform electrical or pharmacological cardioversion was made at the operator’s discretion. In the group of patients who received pharmacological cardioversion, there were 22 (47.8%) patients with paroxysmal AF and 24 (52.2%) with persistent AF. On the other hand, in the group of patients who underwent electrical cardioversion, 21 (48.8%) patients had paroxysmal AF and 22 (51.2%) patients had persistent AF (Figure 1).
An evaluation and comparison of the effectiveness of methods of restoring sinus rhythm was made in the study group as well as among patients particularly with paroxysmal and persistent AF.
Inclusion criteria for the study were eligibility for cryoablation: paroxysmal AF with symptoms when at least one class I or III antiarrhythmic drug was ineffective and the patient preferred further rhythm control; significantly symptomatic AF after evaluation of the benefits and risks of the procedure and informed patient consent; symptomatic patients with persistent drug-resistant AF; AF and heart failure with decreased left ventricular ejection fraction (LVEF).
Patients were loaded orally with 600 mg of propafenone before the procedure was performed, while antazoline and 70 mg of propafenone were given in a bolus immediately after cryoablation.
The primary endpoint of the study was the maintenance of sinus rhythm at discharge.
Patients with acute coronary syndrome and active infection were excluded from the study.
Duration of more than 7 days was accepted as a criterion for persistent AF. The cryoablation procedure was performed by an experienced team.
Kidney failure was defined as an estimated glomerular filtration rate (eGFR) level below 60 ml/kg/min.
A database of study patients was created comparing the groups with pharmacological and electrical cardioversion. Data such as age, sex, weight, height, presence of chronic diseases such as hypertension, diabetes, dyslipidemia, renal failure, history of stroke and myocardial infarction, history of percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG) were analyzed. Medications taken on a regular basis by patients were also evaluated. Additionally, echocardiographic parameters such as left and right atrial area and size and left ventricular ejection fraction were compared. The groups were also compared in terms of parameters assessed during the cryoablation procedure such as the time to cryoablate individual pulmonary veins and the temperature used.
Statistical analysis
Categorical data were compared with the χ2 test and are presented as frequencies. Continuous data with normal distribution (compared with Student’s t-test) are presented as mean and standard deviation (SD). Continuous data with skewed distribution were compared with the Mann-Whitney U test and are presented as medians (first to third quartile). Statistical significance was considered for p-values < 0.05. The analysis was performed with Statistica 13 PL Software.
Results
Considering demographic criteria, the groups were homogeneous with respect to age, number of women, weight, height, presence of hypertension, diabetes mellitus, dyslipidemia, renal failure, history of stroke, myocardial infarction and PCI (Table I).
Table I
Comparison of baseline characteristics and comorbidities between patients with antazoline and propafenone chosen as a sinus restoration method vs. patients with ECV regarding perioperative amiodarone usage
There were no statistically significant differences between the groups with respect to transthoracic echocardiographic findings – LA area, LA diameter, right atrium (RA) area, RA diameter and LVEF (Table II).
Table II
Comparison of echocardiographic parameters between patients with antazoline and propafenone chosen as a sinus restoration method vs. patients with ECV regarding perioperative amiodarone usage
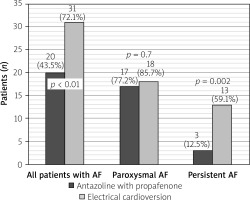
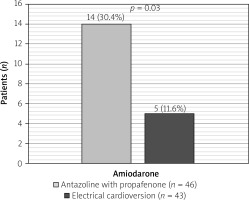
For medications received by patients in the perioperative period, only higher use of amiodarone was observed among patients in the antazoline with propafenone group (14 [30.4%] vs. 5 [11.6%]; p = 0.03) (Figure 2). There were no statistically significant differences in other medications taken between the group receiving antazoline with propafenone and ECV.
Figure 2
Comparison between patients with antazoline and propafenone chosen as a sinus restoration method vs. patients with ECV regarding perioperative amiodarone usage
Patients with paroxysmal and persistent AF were selected from the study group and subsequently assessed. The efficacy of antazoline and propafenone therapy was compared to ECV efficiency in each group.
There were no significant differences between these groups in selected risk factors (age, number of women, weight, height, presence of hypertension, dyslipidemia, renal failure, history of stroke and myocardial infarction), echocardiographic parameters (LA area, LA diameter, RA area, RA diameter, LVEF), and medications during hospitalization (β-blockers, ACE inhibitors, angiotensin receptor blockers, anticoagulants, amiodarone and aldosterone antagonists).
On the other hand, patients with persistent AF, in case of the therapy used , differed only in the presence of diabetes mellitus (2 [8.3%] vs. 5 [22.7%]; p = 0.05) and hypertension (18 [75%] vs. 21 [95.5%]; p = 0.001), which were more common among patients undergoing ECV. There were no other statistically significant differences in other compared risk factors (age, number of women, weight, height, dyslipidemia, renal failure, myocardial infarction and history of stroke) and echocardiographic parameters.
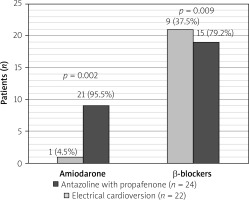
In the group of patients with persistent AF there were noted two statistically significant differences regarding use of medications – β-blockers were more commonly used in the ECV group (19 [79.2%] – ECV vs. 21 [95.5%] – pharmacological cardioversion; p = 0.009), whereas amiodarone was chosen more frequently in patients on antazoline and propafenone (9 [37.5%] vs. 1 [4.5%]; p = 0.0002) (Figure 3).
Figure 3
Comparison of drugs used during hospitalization between antazoline and propafenone vs. ECV approach in patients with persistent AF
Irrespective of the type of AF, in the study group of 89 patients, there was a higher rate of successful sinus rhythm maintenance at discharge using electrical cardioversion (31 (72.1%)) compared with the use of antazoline with propafenone (20 [43.5%]) (p < 0.01). However, among patients with paroxysmal atrial fibrillation, the difference in efficacy between electrical and pharmacological cardioversion using these drugs was not statistically significant (18 [85.6%] vs. 17 [77.3%] p = 0.7]. Another phenomenon observed was a significant difference in the efficacy of these two methods in patients with persistent AF – 13 (59.1%) cases of successful restoration of sinus rhythm among patients undergoing electrical cardioversion and only 3 (12.5%) in the antazoline and propafenone group (p = 0.002) (Figure 4).
Discussion
This is the first study to compare the efficacy of antazoline with propafenone versus electrical cardioversion in restoring and maintaining sinus rhythm in patients who developed atrial fibrillation during pulmonary vein cryoablation. In addition, we found no papers describing the efficacy of electrical cardioversion in terminating atrial fibrillation during this procedure.
As demonstrated by Wybraniec et al. in the CANT study, antazoline was more efficient than amiodarone and had comparable efficacy to propafenone in the emergency restoration of sinus rhythm [17]. Since many centers use a combination of antazoline and propafenone as a standard of pharmacological cardioversion during cryoablation, we decided to test their efficacy.
According to Balsam et al., antazoline seems to be a safe agent in termination of AF with satisfying efficacy among patients with paroxysmal AF – 83.6% [16]. On the other hand, the termination of persistent AF was worse, at only 31.1%. The efficacy of antazoline in restoring sinus rhythm in short-duration AF was also demonstrated in the Farkowski study, where its efficacy and safety were compared with propafenone. Unfortunately, its efficacy in persistent AF was not evaluated in this study [18]. In our research we detected a similar relationship in which antazoline with propafenone may have significant efficiency, comparable to ECV among patients diagnosed with paroxysmal atrial fibrillation (77.2% antazoline-propafenone vs. 85.7% ECV). In contrast, antazoline with propafenone showed significantly lower efficacy than ECV in the entire study group and especially in patients with persistent AF (12.5% antazoline-propafenone vs. 59.1% ECV). The above-mentioned results of our study indicate that persistent AF not only worsens the efficacy of antazoline and propafenone compared to paroxysmal AF, but also significantly worsens the efficacy of ECV, which may be explained by atrial morphological changes in the course of prolonged AF, worsening its efficacy. Atrial remodeling and the electrophysiological changes it entails are often the cause of AF, although it can also be its effect [19]. Therapy that can inhibit or even reverse atrial remodeling is electrical cardioversion [20], which can reduce recurrence rates and increase efficacy of this therapy in both paroxysmal and persistent AF. This may indicate a preference for this therapy over pharmacological cardioversion, although there are no studies on the reversibility of atrial remodeling with antazoline.
Farkowski et al. [9], in their study evaluating the efficacy of antazoline in preempting AF during PVI procedure, demonstrated its high efficacy in restoring sinus rhythm. They also emphasized careful patient evaluation during intravenous administration of antazoline because it may induce conversion of AF into sustained atrial tachycardia or atrial flutter and reveal additional conduction pathways; therefore despite its good efficacy this drug should be used with caution. In his study, antazoline alone was administered and its efficacy was not compared with other drugs or electrical cardioversion, and the division of atrial fibrillation into paroxysmal and persistent was not considered.
While the results of our study may provide valuable guidance, the efficacy and safety of antazoline with propafenone in patients with atrial fibrillation during pulmonary vein cryoablation should be proven in large, randomized trials. In addition, information on the persistence of sinus rhythm after its restoration would be a valuable addition worth considering in future studies.
As reported by Ceynowa-Sielawko et al. in the CANT II study antazoline seemed to be less effective in PCV of recent-onset AF among patients with eGFR < 45 ml/min/1.73 m2. This effect was not observed with amiodarone and propafenone [21]. It would be advisable to document the effect of eGFR < 45 ml/min/1.73 m2 and chronic kidney disease on the efficacy of antazoline with propafenone used during the pulmonary vein cryoablation procedure.
The limitations of this study are that the study presents only short-term results and did not evaluate persistence of sinus rhythm after the end of hospitalization. It also had moderate sample size and a single-center design; thus a multicenter study would be needed to obtain the most reliable results. This research did not take into account the placement of electrodes during the electrical cardioversion procedure, which could have an impact on the effectiveness of rhythm restoration. In addition, we did not analyze the energy required to perform an effective cardioversion or the number of attempts. In addition, due to the retrospective nature of the study, the energy required for successful cardioversion and the number of attempts were not analyzed.