Unroofed coronary sinus (CS) syndrome, also referred to as CS septal defect, represents a rare congenital cardiac abnormality characterized by the absence of the roof of the coronary sinus, leading to a partial or complete communication between the coronary sinus and the left atrium. The prevalence of the syndrome was found to be 0.36% [1]. The unroofed coronary sinus syndrome was initially reported by Raghib et al. in 1965 [2]. The early and accurate diagnosis of unroofed coronary sinus syndrome is of diagnostic significance due to the potential for right-to-left shunting, which can result in cerebral emboli [3]. The diagnosis is frequently challenging and may be delayed due to the non-specific nature of clinical signs and symptoms [4].
We illustrate the case of a 1.5-year-old girl presenting with failure to thrive and a heart murmur. The diagnosis of sinus venosus atrial septal defect with unroofed coronary sinus was suggested by echocardiography. Due to unclear delineation of a complete CS, the patient underwent cardiac computed tomography angiography (CCTA). CCTA confirmed a completely unroofed CS (Figure 1 A, white dashed line) without persistent left-superior vena cava (L-SVC). The only developed part of the CS, visible on CT, was the bottom of the CS (Figure 1 A, red dashed line) and a “beak” (Figure 1 A, *) located between the left atrial appendage (LAA) and the left lower pulmonary vein. The diameter of the interatrial communication was approximately 2 cm (Figure 1 B). Both the right atrium and right ventricle were qualitatively enlarged.
Figure 1
A – Completely unroofed coronary sinus (CS) (white dashed line) without persistent left-superior vena cava – coronal view. Red dashed line represents the bottom of the coronary sinus. Asterisk represents the beak of the coronary sinus. B – The diameter of the interatrial communication was approximately 2 cm. C, D – Perioperative findings. The surgical probe tip points to the ostium of the CS in the left atrium
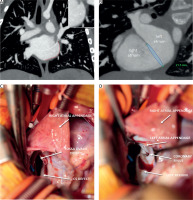
The patient was discussed within a multidisciplinary heart team, and was subsequently referred for surgery. The completely unroofed CS was confirmed perioperatively. Moreover, a confluent atrial septal defect (fossa ovalis plus CS type) was found (Figure 1 C). After administering an antegrade cardioplegia solution, the ostium of the CS in the left atrium (LA) was identified. The surgical probe tip points to the ostium of the CS in the LA (“beak” on CT, Figure 1 D). The defect was surgically repaired using autologous pericardial patch closure, and the CS was left to drain into the LA. The observed mild desaturation, a typical outcome of this procedure, was deemed acceptable. The post-operative transesophageal echocardiography demonstrated no residual shunt and normal systolic function. The postoperative course was uneventful, and the patient was discharged on the fourth day after surgery. At follow-up, the patient exhibited a favorable clinical course, characterized by preserved ventricular function and the absence of residual shunting.
Our case demonstrates a very rare type of completely unroofed CS without persistent L-SVC. CCTA plays a crucial role in CS imaging.






