Chylothorax is a rare but potentially life-threatening complication that can occur after disruption of the thoracic duct [1]. While iatrogenic and malignant causes are more common, penetrating trauma – particularly involving the neck – is an exceptionally rare etiology [2, 3].
Herein, we report a rare instance of chylothorax secondary to a contralateral thoracic duct injury following a right-sided cervical stab wound. Notably, an initial attempt at leftside cervical duct ligation failed to control the chyle leak, ultimately necessitating successful right-sided video-assisted thoracoscopic duct ligation.
A 43-year-old previously healthy male patient was admitted to the emergency department after sustaining a stab wound to the right side of the neck. On physical examination, there was a small stab wound approximately 1 cm in length on the right side of the neck, without any visible bleeding or active drainage. The patient was hemodynamically stable with a blood pressure of 110/60 mm Hg and heart rate of 85 beats per minute, but was mildly hypoxic with an oxygen saturation of 90% on room air.
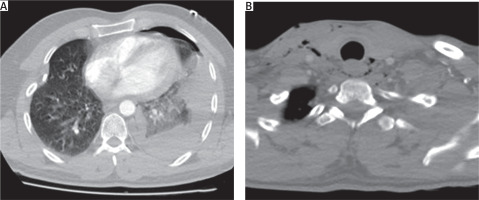
Contrast-enhanced computed tomography (CT) of the neck and thorax revealed a left-sided hydropneumothorax, an unexpected finding given the right-sided cervical entry point of the stab wound. Careful evaluation of the CT images demonstrated a linear tract of mediastinal emphysema extending posterior to the esophagus, suggesting that the penetrating object had followed a retroesophageal path (Figures 1 A, B). An urgent left-sided tube thoracostomy was performed, and the patient was admitted to the intensive care unit for close monitoring. Initial drainage was hemorrhagic in character, totaling approximately 700 ml within the first 24 hours. Given the left-sided vascular findings and the retroesophageal air tract noted on CT, there was a clinical concern for possible concomitant esophageal or tracheal injury. To minimize the risk of contamination in the event of an esophageal perforation, oral intake was withheld. On the first post-admission day, both bronchoscopy and upper gastrointestinal endoscopy were performed, and no evidence of tracheal or esophageal injury was identified.
Figure 1
Computed tomograpohy (CT) images demonstrating the unusual trajectory of a contralateral penetrating cervical injury. A – Axial thoracic CT showing a left-sided hydropneumothorax and lung contusion. B – Axial cervical CT revealing retroesophageal air tracking indicative of mediastinal penetration
On the second day of follow-up, the character of the pleural drainage changed from hemorrhagic to milky white in appearance. Biochemical analysis of the pleural fluid revealed a triglyceride level of 193 mg/dl and a cholesterol level of 41 mg/dl, yielding a triglyceride-to-cholesterol ratio of 4.7, consistent with the diagnosis of chylothorax. Oral intake remained restricted due to the initial concern for esophageal injury. Total parenteral nutrition was initiated via a central venous catheter, and intravenous octreotide therapy was started at a dose of 100 µg three times daily. This regimen was continued for 5 days with nil per os status except for water.
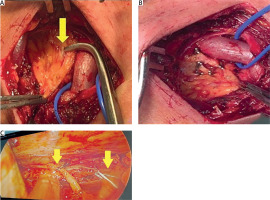
Despite conservative management, the daily chyle output remained high and did not show any significant decrease. Therefore, surgical intervention was planned. Through a left supraclavicular incision, the thoracic duct was carefully explored and clearly identified. The site of ductal injury, presumed to be caused by the stab wound, was visualized and marked (Figure 2 A). The thoracic duct was then doubly clipped both proximally and distally to the area of disruption to ensure complete control of the leak (Figure 2 B). During the 3-day follow-up period after cervical duct ligation, there was no significant reduction in chyle output. As a result, right uniportal video-assisted thoracoscopic surgery (VATS) was performed, and the thoracic duct was ligated (Figure 2 C). Oral intake was resumed on the first postoperative day. Since no further chylous drainage was observed, the chest tube was removed on postoperative day two, and the patient was subsequently discharged. At the 6-month outpatient follow-up, there was no evidence of chyle reaccumulation or recurrence of pleural effusion.
Figure 2
Intraoperative views demonstrating stepwise surgical management of thoracic duct injury. A – Left supraclavicular exploration showing the thoracic duct with the site of injury marked by the yellow arrow. B – Cervical thoracic duct ligation with double clips placed proximally and distally to the injured segment. C – Right uniportal VATS view demonstrating thoracic duct ligation after failure of cervical approach
Chylothorax is an uncommon but clinically significant condition characterized by the accumulation of chyle in the pleural cavity due to disruption of the thoracic duct [1]. It accounts for approximately 2–3% of all pleural effusions and may lead to severe complications including respiratory compromise, malnutrition, and immunosuppression if not managed effectively [1, 4]. Under normal physiological conditions, the thoracic duct transports approximately 2.4 l of chyle per day, and its disruption can lead to rapid and clinically significant accumulation within the pleural space [4]. Chylothorax was classically categorized by De-Meester into congenital, traumatic, malignant, and miscellaneous causes, but is now more commonly divided into traumatic and non-traumatic etiologies [5, 6]. Traumatic chylothorax constitutes a minority of cases, and is most often associated with blunt thoracic trauma; penetrating cervical injuries represent an exceptionally rare cause [2, 3].
Previously, Eren et al. reported the case of a left-sided cervical stab wound causing chylothorax, which was successfully managed with conservative treatment including tube thoracostomy and total parenteral nutrition [7]. Their report underscores the potential for nonoperative management in selected cases of isolated thoracic duct injury following penetrating neck trauma. In contrast, this experience demonstrates a more complex clinical scenario: the thoracic duct was injured contralaterally relative to the stab entry site, and conservative therapy failed to resolve the chyle leak. Two separate surgical interventions – first via left cervical exploration and subsequently through right-sided VATS – were ultimately required to achieve complete resolution. To our knowledge, this is one of the few reported instances in which both the atypical trajectory of injury and the stepwise surgical management are clearly documented with intraoperative imaging.
The initial surgical approach was guided by the anatomical course of the thoracic duct and the location of the cervical stab wound. Given that the duct typically drains into the left subclavian vein, and considering the cervical entry site of the injury, it was presumed that the disruption had occurred near its terminal segment. Therefore, a left supraclavicular exploration was performed, during which the thoracic duct was visualized and doubly clipped. Despite technically successful ligation, the chyle leak persisted. In the second step, right-sided video-assisted thoracoscopic surgery (VATS) was undertaken, which is the most commonly employed approach for thoracic duct ligation in high-output chylothorax. The duct was clearly identified and clipped, resulting in immediate cessation of chylous drainage.
In conclusion, although thoracic duct injury secondary to penetrating cervical trauma is rare, it should be considered in patients presenting with delayed chylothorax. Accurate radiological evaluation and early biochemical confirmation are critical for timely diagnosis. While conservative management remains the initial strategy, persistent high-output chyle leaks may necessitate surgical intervention. This experience highlights that, in anatomically complex or refractory situations, a stepwise surgical approach – including both cervical exploration and thoracoscopic duct ligation – can be safely and effectively employed.






