After successful crossing with a Fielder XT-R wire (Asahi Intecc USA, Inc.), recanalization and stenting a chronic total occlusion (CTO) of the left circumflex (LCX) coronary artery (Figure 1 A), distal coronary artery perforation (CAP) was detected (Figure 1 B), but it was not definitive whether this CAP emptied into the pericardium or into a cardiac chamber [1].
Figure 1
A – Initial angiography with chronic total occlusion of the proximal left circumflex artery (white arrow). B – After successful intervention, a coronary artery perforation (CAP) is seen in the distal vessel (red arrow), but it is not definitive whether this perforation emptied into the pericardium (Ellis classification III) or into the left ventricle (Ellis classification III cavity spilling). C – Transthoracic echocardiography showed no evidence of pericardial effusion. D – Contrast-enhanced echocardiography after intravenous injection of the ultrasound contrast agent (UCA), the UCA is absent from the pericardium
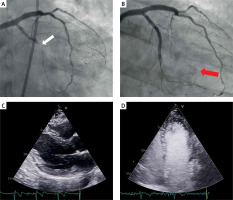
The patient remained hemodynamically stable, and transthoracic echocardiography (TTE) showed no evidence of pericardial effusion (Figure 1 C). Despite prolonged balloon inflation, spontaneous sealing was not achieved. To clearly define the direction of the CAP, contrast-enhanced TTE was performed after intravenous injection of 3 ml of sodium hexafluoride-based ultrasound contrast agent (UCA), SonoVue (Bracco International B.V., Amsterdam, NL), followed by 5 ml of a slow normal saline flush [2]. The echocardiographic contrast is used intravascularly and is visualized as hyperechoic spots using dedicated imaging protocols. The identification of contrast in the pericardial space implies active extravasation. No evidence of contrast in the pericardial space was detected in our patient, ruling out active intrapericardial bleeding (Figure 1 D). Following this, anticoagulant reversal with protamine was not performed and the procedure was then completed as it was felt there was no risk of late cardiac tamponade. The patient was discharged 24 h later, with a normal bed-side echocardiography and remains asymptomatic at 6 months’ follow-up. This case illustrates the utility of UCA along with TTE for the definitive diagnosis of CAP leaking into a cardiac chamber and excluding a communication with the pericardium.
Coronary artery perforations occur in approximately 0.3% to 0.5% of all percutaneous coronary interventions (PCIs) with higher rates in CTO PCI (4%). Appropriate management of perforations is essential as they can result in tamponade, hemodynamic collapse, and mortality. Depending on the severity and location, management of perforations varies from supportive care to emergent percutaneous treatment or cardiac surgery [1, 3].
Contrast-enhanced echocardiography (CEE) is an echocardiographic technique that uses UCAs, which are injectable echo-reflective microbubbles to improve imaging of the cardiac chambers and blood-filled spaces [2, 4]. In the setting of coronary perforations, these microbubbles better define the clinical impact of the perforation. UCAs can differentiate if there is blood extravasation into the pericardium or into a cardiac chamber as in our case. The technique is performed in the cath lab with UCA injected via a guide catheter directly into the coronary artery, or via peripheral intravenous access with the same dilution protocol, and similar diagnostic accuracy as in our case.
If ongoing bleeding is seen on angiography and UCA is present in the pericardium, it is consistent with a coronary perforation into the pericardium. If ongoing bleeding is seen on angiography, but UCA does not fill the pericardium, this excludes active intrapericardial bleeding and it is usually consistent with bleeding into a cardiac chamber or coronary vein as in our case.








