Introduction
Coarctation of the aorta (CoA) is a congenital heart defect characterized by a narrowing of the aorta, typically near the insertion of the ductus arteriosus.
While significant strides have been made in improving the outcomes of CoA repair, the occurrence of recoarctation poses a formidable challenge, warranting a meticulous exploration of its prevalence, associated risk factors, and subsequent management.
Recoarctation, while commonly used in both clinical practice and academic literature, can be a somewhat imprecise term. It does not signify a recurrence of the original congenital condition, but rather it refers to a new narrowing or obstruction at the site of a previous surgical repair for aortic coarctation. This phenomenon results from restenosis, a process where the vessel re-narrows after the initial correction. In this context, recoarctation is more accurately understood as a postoperative complication rather than a return of the initial defect.
Understanding the prevalence of recoarctation is essential for gauging the success of surgical interventions and developing targeted postoperative care strategies. Current literature suggests a variable incidence of recoarctation, ranging from 5% to 30% across different cohorts [1, 2]. This broad range underscores the complexity of factors influencing recoarctation dynamics, prompting the need for a nuanced examination of contributing variables.
In this study, we conducted on a comprehensive exploration of recoarctation after CoA repair, investigating the relationships among factors contributing to its occurrence.
Aim
We aimed to determine the prevalence of recoarctation, identify significant risk factors influencing its development, and assess the impact of different surgical techniques on its incidence.
Material and methods
A retrospective cohort investigation was conducted wherein medical records and computed tomography (CT) scans were retrospectively analyzed. Pertinent data, including intraoperative procedures, intraoperative and postoperative complications, and CT scan measurements, were gathered and recorded in an Excel spreadsheet for subsequent statistical analysis. Patient information and CT scan measurements were documented in separate Excel sheets to minimize performance and detection bias. Given that clinical audits entail no deviation from standard clinical management, patient consent or formal ethical review/approval was not required; thus, the present study was registered as a clinical audit, and all data were de-identified.
The study included 120 patients diagnosed with isolated CoA who underwent elective surgical repair over the past decade. Patient data encompassed preoperative medical examination results, including echocardiography (echoCG) and multi-slice computed tomography findings, postoperative hospital status with echoCG results, and follow-up examination findings at 1 month and 1 year post-operatively with echoCG. All echoCG examinations were conducted in accordance with established guidelines [3]. In our investigation, recoarctation was evaluated using the pressure gradient on the coarctation site measured by echoCG. A threshold of more than 20 mm Hg was employed to define recoarctation, in line with the recommendations of various authors and guidelines [1, 4]. Early recoarctation was characterized by a pressure gradient exceeding 20 mm Hg during the initial examination after the operation, typically conducted during the hospital stay. Late recoarctation, on the other hand, was identified when a pressure gradient greater than 20 mm Hg was observed in follow-up examinations conducted 1 year post-operatively.
Preoperative CT scans were scrutinized, and measurements were conducted utilizing Syngo.via ProtoNeo software (Siemens Healthcare GmbH/Siemens Medical Solutions USA, 2018), adhering to the Society for Vascular Surgery guidelines and reporting standards [5].
Hypoplasia of the aortic arch was evaluated based on the diameter of the aorta, which was measured using CT scans. These measurements were then converted into z-scores to standardize for body size and age. A z-score of less than –2.0 was considered indicative of a hypoplastic aortic arch. This threshold allowed us to identify patients with significant narrowing of the aortic arch relative to normal population values.
Patients were divided into four distinct age groups for analysis: Group 1 consisted of patients under 1 year of age, Group 2 included those aged 1–3 years, Group 3 comprised patients between 3 and 10 years, and Group 4 encompassed patients over 10 years of age. This stratification allowed for a more precise comparison of outcomes across different developmental stages and facilitated the evaluation of age-related factors in recoarctation risk.
The patients in this study underwent four different types of surgical procedures for aortic coarctation repair:
– Resection and end-to-end anastomosis (EEA): This procedure involves the removal of the narrowed section of the aorta, followed by the direct connection of the two healthy ends.
– Patch aortoplasty: In this technique, a synthetic patch is used to enlarge the narrowed section of the aorta without removing any part of the vessel.
– Interposition graft: This method involves the insertion of a graft (usually synthetic) to replace the resected portion of the aorta.
– Resection and extended EEA (EEEA): This is an extended version of the EEA, where a larger segment of the aorta is resected to ensure a wider and more durable anastomosis.
All operations were performed by three experienced cardiac surgeons, each with over 15 years of experience in pediatric cardiac surgery.
Statistical analysis
Statistical analyses were conducted using SPSS Statistics 22.0 software, checking for homogeneity (Levene’s test) and normal distribution (Q-Q plot). Mean and standard deviation (SD) summarized symmetrically distributed numerical variables, while median and inter-quantile range (IQR) described non-symmetric numerical variables. The χ2 test was used for categorical (nominal and ordinal) variables. Comparison of means was performed using the paired t-test or Wilcoxon signed-rank test for paired variables and the independent t-test or Mann-Whitney U test for independent variables according to normality and homogeneity. Pearson’s correlation coefficient was utilized for correlation tests. A significance level of p < 0.05 was employed in this study.
Results
The study revealed that 30 (25%) patients experienced early recoarctation, while 52 (43.7%) patients encountered late recoarctation.
A correlation test conducted between early and late recoarctation demonstrated a robust positive correlation (r = 0.644, p < 0.001), indicating that individuals experiencing early recoarctation were more likely to exhibit late recoarctation as well.
The investigation into patient-related factors for these cohorts yielded the following results (Table I).
Table I
The investigation into patient-related factors
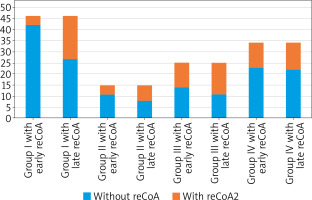
Upon examining the occurrence of early and late recoarctation status within different age groups, the following results were observed (Table II).
Table II
Occurrence of early and late recoarctation status in different age groups
From the Table II and Figure 1, it is evident that the early recoarctation rate was higher in older age groups compared to younger groups, and the χ2 test showed a significantly different distribution (p = 0.006). However, the number of patients with recoarctation differed significantly in younger age groups, especially in patients less than 1 year of age, and the percentage of patients with late recoarctation did not differ significantly between age groups (p = 0.358). Overall, in older patients, the risk of recoarctation is higher than in younger patients, but this proportion remained stable with time. Meanwhile, the proportion of patients with early recoarctation can be lower in younger patients, but this tends to increase over time. This finding requires further investigation to assess the factors that affect younger patients in developing recoarctation later.
Analyzing the influence of pre-operative echocardiographic findings on the development of early and late recoarctation yielded the following results (Table III).
Table III
Analyzing the influence of pre-operative echocardiographic findings on the development of early and late recoarctation
Our initial hypothesis suggesting that the severity of aortic coarctation influences the development of early and late recoarctation was not confirmed by statistical tests. The analyses revealed that only patients with left ventricular (LV) dysfunction, characterized by LV dilation, higher end-diastolic volume of the left ventricle (EDVLV), and lower ejection fraction of the left ventricle (EFLV), are at risk of early recoarctation. Additional comparison tests of CT scan findings could provide further insights into this topic (Table IV).
Table IV
Analyzing the influence of pre-operative CT scan findings on the development of early and late recoarctation
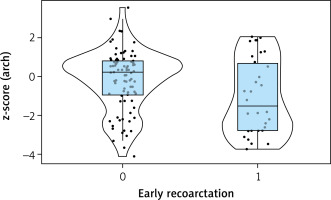
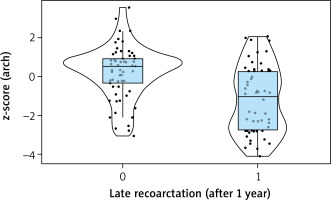
Several factors, such as the sizes of the ascending and descending aorta, and the size and z-score of the aorta at the diaphragm level, were initially considered to be influenced by age. However, upon closer examination, early recoarctation was found to occur more frequently in older age groups, and these factors became non-significantly different in the late recoarctation check. Only two variables remained significantly different, namely the z-score of the aortic arch and the z-score of the isthmus. Consequently, the z-score of the aortic arch and the z-score of the isthmus were significantly lower in patients with early and late recoarctation.
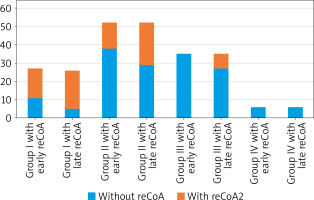
Many authors have reports [1, 2, 4] that one of the main risk factors for recoarctation is the surgical technique employed. To assess the impact of different operation types on recoarctation, we compared the incidence of recoarctation among the four surgical groups (Figure 2).
The analysis revealed notable variations in the rates of recoarctation among different surgical techniques. Patients who received a prosthetic interposition graft (PIG) did not exhibit any instances of early or late recoarctation. In contrast, resection and EEA displayed the highest proportions of early (59%) and late (77%) recoarctation. Prosthetic patch aortoplasty (PPA) showed a higher rate of recoarctation, with 27% of patients experiencing early recoarctation and 44% exhibiting late recoarctation. Resection and extended end-to-end anastomosis displayed a lower rate, with 0% experiencing early recoarctation and 23% exhibiting late recoarctation.
Discussion
The data in the table reveal that the mean age of patients with early recoarctation was higher compared to patients without early recoarctation. Intriguingly, the mean age at the time of the operation was lower in patients who later developed late recoarctation. However, a comparison test (t-test) indicated no statistical significance (p = 0.177). This implies that patient-related variables such as age, height, weight, gender, and body mass index (BMI) may not be causative factors in the development of early or late recoarctation.
The clinical significance of age at the time of repair in relation to recoarctation has been underscored in several studies [6, 7]. Additionally, investigations encompassing various factors, such as weight before surgery, have yielded mixed findings [6–9]. Some studies have suggested a noteworthy association between lower weight at the time of repair and arch restenosis [9].
However, the complexity of these associations becomes apparent when considering multivariable models. Notably, Gorbatykh et al. [8] observed that weight did not emerge as a significant risk factor when included in a multivariable model alongside different surgical strategies. Furthermore, contrasting perspectives have been presented regarding birthweight and body length at surgery as potential risk factors. While some studies posit lower birthweight [10] and smaller body length at surgery [11] as risk factors, our series challenges these assertions, suggesting that these factors may not be conclusive indicators of susceptibility to early or late recoarctation.
Among the 28 (23.3%) patients who had arch hypoplasia, 12 of them experienced early recoarctation, and 22 of them exhibited late recoarctation. Interestingly, only 6 patients (21.4% of patients with arch hypoplasia) did not experience recoarctation. Correlation tests demonstrated a strong negative correlation of the z-score of the arch size with both early recoarctation (r = –0.229, p = 0.013) and late recoarctation (r = –0.421, p < 0.001). Therefore, it can be concluded that arch hypoplasia is one of the main risk factors for the development of both early and late recoarctation (Figures 3, 4).
Numerous studies [6–8, 10–12] have explored the relationship between recoarctation and aortic arch morphometry. Conflicting results have been reported, with some studies identifying a hypoplastic aortic arch as a significant risk factor. Hager et al. [11] reported that the presence of a hypoplastic arch increased the odds of developing recoarctation or experiencing mortality by 2.9 to 1. However, Gorbatykh et al. [8] found that a hypoplastic arch did not remain a determinant factor when incorporated into a multivariable regression model alongside different types of surgical strategies. Intriguingly, McElhinney et al. [7] found that a smaller transverse arch diameter was associated with an elevated risk of recoarctation, and this effect was more pronounced when indexed to weight. Additionally, Burch et al. [12] concluded that for every 1-mm increase in the transverse arch diameter, the risk for recoarctation decreased by 43%. This collective evidence underscores the importance of considering hypoplastic aortic arch as a crucial risk factor for recoarctation when deciding on the optimal repair strategy.
While assessing the impact of different surgical methods on developing recoarctation, it is important to note that prosthetic interposition graft (PIG) was considered a less risky group. However, this observation should be interpreted cautiously, as PIG was primarily performed in older patients whose growth had nearly concluded. Consequently, the lack of recoarctation in the PIG group may be attributed to limited patient growth, preventing the graft size from becoming insufficient. Therefore, while PIG demonstrated a lower risk in this specific context, it cannot be conclusively deemed a universally safe method for all patients. In summary, all methods of coarctation repair carry some risk of recoarctation, but resection and EEA and PPA appear to have a higher risk than EEEA (Table V).
Table V
Impact of different operation types on recoarctation
Concerning the choice of surgical technique, the literature has emphasized that extended end-to-end anastomosis is considered a superior alternative for preventing recoarctation. This preference is attributed to the method’s advantages, including a more extensive resection, preservation of the subclavian artery, and the use of an oblique anastomosis [13–15].
To assess the impact of operation type within distinct age groups, the obtained results are as follows (Table VI). The Table illustrates that early recoarctation predominantly occurred in older age groups, particularly in cases involving EEA and PPA. EEA demonstrated a higher rate of early recoarctation across all age groups, with a more pronounced increase in older groups from an early stage, while in younger groups, it exhibited a tendency to rise over time. PPA exhibited more favorable short-term results in younger groups; however, the proportion of recoarctation in these groups significantly escalated, reaching up to 75%. In contrast, in older groups, although short-term results might be less favorable, they did not worsen significantly over time. EEEA exhibited the best short-term results, with 0% early recoarctation across all age groups. Nevertheless, in patients under 1 year of age, the proportion of late recoarctation reached up to 27.6%. It is important to note that the EEEA method was only applied to small children, and its performance in older populations remains unassessed.
Table VI
Impact of operation type within distinct age groups
In the literature, the EEA method has been considered the most prone to recoarctation, with reported rates reaching as high as 86% [1, 4], while PPA showed similar results in infant patients. However, in older patients, the recoarctation rate after PPA was lower [1, 16]. Across all methods, younger groups exhibited an increasing proportion of recoarctation over time. The primary surgical reasons for recoarctation are believed to include the following factors:
– Inadequate resection of all ductal tissues. Incomplete resection of the stenosis leads to the formation of thickened and nonelastic ends, hindering the growth of the anastomosis. Scarred walls with these characteristics are unable to undergo normal growth in subsequent years. Elzenga and Gittenberger’s [17] research revealed that the coarctation tissue and the adjacent portions of the aortic wall may contain ductal material, which, if not completely removed, poses a risk of restenosis. These histologic findings provide robust support for the hypothesis that every possible effort should be exerted to excise the constricting tissue and revert to the normal aortic wall, enabling growth at both ends. Therefore, methods of EEA and PPA showed higher risk of recoarctation, while in these methods there is high risk of leaving ductal tissue.
– Lack of growth of a suture line. The limited growth of a suture line has been identified as a potential factor contributing to increased pressure gradients across a coarctation site, particularly in procedures such as EEA and EEEA. While silk sutures were initially employed for anastomosis, contemporary practices in major centers have shifted towards using prolene 6.0. Nevertheless, various authors have reported that the lack of suture line growth remains a concern. Consequently, some experts recommend considering the use of prolene 7.0 or even prolene 8.0 for infants in these procedures to mitigate the risk of recoarctation [18].
– Lack of growth of a hypoplastic transverse arch. The inadequate growth of a hypoplastic transverse arch has been substantiated by our preceding statistical analyses. Notably, Kotani et al. [19] reported a remarkable 90% freedom from reoperation at 3 years with EEEA, even in cases of severe hypoplastic aortic arch (z-value < –6). Several other studies have consistently concluded that EEEA yields superior results in patients with a hypoplastic aortic arch [1, 6]. However, when we examined the impact of hypoplastic arch status across different operation methods, it became evident that patients with arch hypoplasia exhibited a high risk of late recoarctation in all methods: 100% in EEA, 75% in PPA, and 80% in EEEA among patients with a hypoplastic arch. In summary, aortic arch hypoplasia emerges as a principal risk factor for recoarctation, and none of the employed surgical techniques provide complete mitigation for these patients.
Despite numerous studies comparing various surgical strategies [1, 4, 16], the evidence suggests that there is no universally superior technique, and the selection among them should be customized based on individual patient characteristics.
In managing patients with coarctation of the aorta and coexisting conditions (multimorbidity), various alternative approaches have been explored to optimize outcomes. One such strategy is the use of mini-invasive interventions as a bridge to definitive surgical repair, particularly in critically ill newborns. Haponiuk et al. [20] demonstrated the efficacy of this approach in a case where a newborn with severe multiorgan failure underwent stenting prior to a major surgical repair, allowing for stabilization before definitive correction. Additionally, in emergency situations involving premature newborns, timely surgical intervention is crucial. Another study [21] highlighted the successful emergency repair of the aortic arch in a premature infant, emphasizing the challenges of addressing both prematurity and critical aortic defects. Hybrid and percutaneous interventions have also gained attention during the COVID-19 pandemic as viable options for managing complex coarctation cases in high-risk patients, as illustrated by Haponiuk et al. [22] in a more recent study. These alternative methods provide valuable insights into the evolving strategies for treating complex cases of aortic coarctation in patients with significant comorbidities.
Conclusions
The analysis of patient-related variables, including age, height, weight, gender, and BMI, suggests that these factors may not directly contribute to the development of early or late recoarctation. However, our findings indicate that aortic arch hypoplasia emerges as a significant risk factor for both early and late recoarctation, highlighting the importance of this anatomical characteristic in patient risk assessment and surgical planning.
Furthermore, while all methods of coarctation repair carry inherent risks of recoarctation, our study suggests that certain surgical techniques may pose a higher risk than others. Specifically, resection and EEA and PPA appear to be associated with a greater likelihood of recoarctation compared to EEEA.
In summary, our findings underscore the complexity of recoarctation development and its multifactorial nature. Recognizing the significance of aortic arch hypoplasia and considering the differential risks associated with various surgical techniques are essential for optimizing patient outcomes and reducing the incidence of recoarctation in individuals with coarctation of the aorta. Further research and ongoing surveillance are warranted to refine risk stratification strategies and improve the long-term management of patients undergoing surgical repair for coarctation of the aorta.