Introduction
Growth hormone deficiency (GHD) is a medical disorder caused by insufficient secretion of the growth hormone. Approximately 1 : 4000 to 1 : 10,000 children worldwide are affected by this condition [1, 2]. The most prominent effect of GHD is a short stature, defined as a height of less than –2.0 standard deviation score (SDS) or below they third percentile [3, 4]. Currently, most children with GHD achieve normal height as a result of recombinant human growth hormone (rhGH) therapy, which has been shown to be safe and effective. However, the success of the treatment may be influenced by a variety of factors [5].
Simultaneously, prevalence of overweight and obesity, measured by body mass index (BMI) between the 1 SD and 2 SD and over 2 SD in children, respectively, is constantly increasing [6, 7]. According to a World Health Organisation (WHO) study, over 390 million (20%) children and adolescents aged 5–19 years were overweight in 2022, including 160 million (8%) who were living with obesity in 2022 [8]. Excessive body weight is proven to influence GH secretion and GH provocative testing [9].
The anterior pituitary gland secretes growth hormone (GH) in a pulsatile manner under the control of either growth hormone-releasing hormone (GHRH) or, in the opposite way, somatostatin; however, the amount of GH released is affected by a variety of other factors [10]. Chronological age (CA) and pubertal status have the greatest impact on GH level, while it is unclear how other factors such as gender, nutrition, sleep, or body composition influence GH secretion [11–13]. In the context of our study, special attention should be given to ghrelin, an essential factor that stimulates the secretion of growth hormone, the levels of which are reduced in individuals with obesity [14].
The purpose of the study is to assess one of the parameters contributing to the GH level, excessive body mass, described by the BMI status, and in accordance with it, further investigate the therapeutic response to rhGH in GHD children, including long-term follow-up.
Material and methods
Study design
Utilising the medical records of short-statured children receiving rhGH at the Clinical Paediatric Department of the Provincial Specialist Children’s Hospital in Olsztyn, a single-centre, retrospective cohort study was carried out. Patients having an isolated GHD diagnosis (multihormonal hypopituitarism were not included) and at least one year of follow-up were included. GHD diagnosis was made according to a standard scheme, using 2 different GH stimulation tests [15, 16]. The cut-off value for GH stimulation tests was 10 ng/ml. Patients were enrolled in the study regardless of their pubertal status at the start of rhGH treatment. The exclusion criteria were the lack of data (e.g. due to continuation of treatment in other medical facilities) and the presence of diseases that could affect growth, which makes these findings incomparable.
Outcomes measurement
The patient’s bone age (BA), height, weight, insulin-like growth factor 1 (IGF-1) level, and rhGH dosage for up to 10 years at yearly intervals were all extracted from the hospital database. We opted to incorporate the IGF-1 level into our analysis because it is frequently utilised in various studies as a substitute for GH due to its resistance to daily fluctuations.
Height, BMI, and IGF-1 were standardised for chronological age and gender using World Health Organisation (WHO) percentile and z-score calculations and somatic development indicators for Polish children, to assess the efficacy of rhGH therapy [17–19]. The average change in growth SDS over 5 consecutive years, starting with the baseline year, provided the basis for the height velocity (HV). The “baseline” refers to the start of rhGH treatment.
At each stage of observation, children were separated into 3 groups based on their BMI SDS. Patients in the first group were underweight and had BMI SDS below –1.65 SD. Patients in the second group varied in body weight from –1.65 SD to 1 SD of the BMI SDS (normal weight). Overweight patients and patients with obesity, with a BMI SDS over the 1 SD made up the third group, later called “excessive body weight”. The authors decided to omit the underweight group from the analysis because the main subject of the study is the difference between the normal and excessive weight children. However, the presence of an underweight group is essential because it cannot be combined with normal weight group. Current consensus recommendations for calculating the ideal weight for children under the age of 19 years were used to develop BMI SDS control points [20]. Based on the characteristics of the groups from the previous year, the treatment’s results are determined, for instance, baseline BMI SDS impacts change (Δ) height SDS in the first year.
Statistical analysis
Applying descriptive statistics, data were analysed. The values of the same parameter of the excessive- and normal-weight groups were compared using Student’s t-test for independent groups or the Mann-Whitney U test (parametric data) and the χ2 test (non-parametric data). P-values below 0.05 were regarded as significant, and those ranging from 0.05 to 0.1 were regarded as nearly significant. All calculations were preceded by Shapiro-Wilk and Levene tests. The analysis was performed using Statistica (data analysis software system), version 13, http://statistica.io (accessed March 4, 2024) TIBCO Software Inc., Krakow, Poland (2017).
Bioethical standards
The Provincial Specialist Children’s Hospital in Olsztyn’s Research Ethics Committee granted ethical permission (REC 29/ZE/2022/WSSD). Our institution gave the appropriate consent to conduct the study. Due to the retrospective nature of the study, consent to participate in the study was not obtained from patients or legal guardians. However, they signed a consent form for treatment with rhGH.
Results
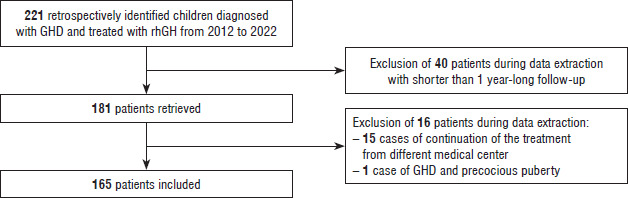
Between 2012 and 2022, the Department of Clinical Paediatrics at the Provincial Specialist Children’s Hospital in Olsztyn, Poland diagnosed 221 children with GHD and administered rhGH to treat them. The Polish guidelines for rhGH therapy were followed in the short-stature treatment [21]. Following the screening of 221 children, 40 were disqualified based on the follow-up requirements. The follow-up was on average 4.32 ±1.80 years during the observation period, which was between 1 and 10 years. Finally, 16 patients were excluded from the group of 181: 15 patients who continued treatment from various hospitals, and one child who had both GHD and premature puberty. The research comprised 165 children in total. The follow-up rate was 91% (Fig. 1).
Figure 1
Flow chart of the study.
GHD – growth hormone deficiency; rhGH – recombinant human growth hormone
According to the mean BMI SDS (based on the baseline to the fourth year after rhGH therapy onset), the normal-weight group consisted of 133 children (81%): 52 girls (39%) and 81 boys (61%). The 18 patients (11%) in the excessive body weight group comprised 6 girls (33%) and 12 boys (67%). The mean baseline CA was equal to 10.72 ±3.33 years and ranged from 3 to 17 years of age. For the normal-weight group the mean baseline CA was 10.56 ±3.23 years, and for the excessive-weight group it was 11.58 ±2.99 years (p = 0.18). Mean baseline high SDS was –2.58 ±0.65 SD. There were some statistically significant differences between the normal-weight and excessive-weight patients’ characteristics (p < 0.05 or p < 0.1). At almost every point during the observation period, children with overweight or obesity were older (mean baseline to fourth year BA; 12.09 ±2.93 vs. 10.58 ±3.21), had greater IGF-1 SDS (mean baseline to fourth year IGF-1; 1.74 ±1.85 SD vs. 0.16 ±1.25 SD), and had lower rhGH doses (mean baseline to fourth year rhGH dose; 0.1770 ±0.0323 mg/kg/week vs. 0.1923 ±0.0309 mg/kg/week) than normal-weight peers (Table I).
Table I
Characteristics of the groups
[i] The data are presented as mean ±SD. “Baseline” refers to the start of rhGH treatment. P-value refers to differences between excessive- and normal-weight patients. P < 0.05 was regarded as significant, marked in bold, and p < 0.1 was regarded as nearly significant – underlined. CA – chronological age; BA – bone age; SDS – standard deviation score; BMI – body mass index; IGF-1 – insulin-like growth factor 1; rhGH – recombinant human growth hormone.
The authors decided not to include children with longer than a 5-year follow-up in the results due to the small number of children. In the normal-weight group, the mean Δheight SDS (baseline to years 1, 2, 3, 4, and 5) were 0.52 ±0.41 SD, 0.43 ±0.35 SD, 0.32 ±0.34 SD, 0.32 ±0.35 SD, and 0.20 ±0.27 SD, respectively. In the excessive body weight group, the mean Δheight SDS were 0.60 ±0.32 SD, 0.31 ±0.31 SD, 0.15 ±0.30 SD, 0.01 ±0.22 SD, and 0.13 ±0.26 SD. Except for the first year, the increase in height SDS was greater in children with normal body weight compared to children with overweight and obesity. The mean HV (based on height SDS in consecutive years between baseline and fifth year) was 0.44 ±0.25 SD/year for the normal-weight group and 0.32 ±0.24 SD/year for the excessive body weight group when comparing the effectiveness of rhGH. All differences between normal- and excessive-weight groups were statistically significant (p < 0.05) or nearly significant (p < 0.1), except for the first, second, and fifth year of observation. The mean (baseline to fourth year) IGF-1 SDS value was significantly lower in the group with normal body weight (0.16 ±1.25 SD) than in the excessive body weight group (1.74 ±1.85 SD; p < 0.05) (Table II).
Table II
Treatment outcomes
[i] The data are presented as mean ±SD. “Baseline” refers to the start of rhGH treatment. P-value refers to differences between excessive- and normal-weight patients. P < 0.05 was regarded as significant, marked in bold, and p < 0.1 was regarded as nearly significant – underlined. SDS – standard deviation score; HV – height, velocity. HV SDS was based on the mean change of height SDS in consecutive years from the baseline to the fifth year.
This is a 5-year retrospective cohort study that analyses the efficacy of rhGH therapy in short-statured children with GHD. The patients were divided into 3 groups based on their BMI SDS at each yearly control observation: underweight (BMI SDS less than –1.65 SD), normal (BMI SDS between –1.65 SD and 1 SD), and excessive weight (BMI SDS above 1 SD) [16–18]. The mean HV (based on height SDS in consecutive years between baseline and fifth year) for the normal-weight group was 0.44 ±0.25 SD/year and for the excessive body weight group it was 0.32 ±0.24 SD/year (p < 0.1). Mean IGF-1 SDS (based on IGF-1 SDS in consecutive years between baseline and fourth year) for the normal-weight group was 0.16 ±1.25 SD and for the excessive body weight group, it was 1.74 ±1.85 SD (p < 0.05).
Discussion
Genetic, endocrine, and dietary variables all influence postnatal linear growth [22]. Together with thyroid hormones, GH plays a significant role in postnatal development via IGF-1 or direct action on the epiphyseal growth plate [23]. The growth trajectory and height of children are significantly impacted by obesity. As stated by Stovitz et al. adults who were overweight or obese were taller as children and experienced relatively slower height growth during their teenage years. Height difference between the obese and normal-weight group was greatest in females at the age of 11 years, reaching on average 5.7 cm, and 4.5 cm for males of the same age. The presented height difference vanished as participants entered early adulthood [24]. According to Chung et al., obese children may experience a head start in growth in early years, but they are not likely to grow taller as adults and should not exceed their genetic potential [25].
Existing research describes a multifactorial connection between obesity and GH secretion [26]. The hypothalamus regulates GH release from the anterior pituitary gland, which is controlled by numerous factors such as gender, age, sleep, physical activity, diet, and obesity [27]. Abdominal visceral fat and fasting serum insulin level play a key role in GH secretion [11]. According to studies, individuals with obesity have lower levels of spontaneous and induced GH release [28, 29]. Peak GH has a substantial inverse relationship with both intramyocellular lipids and intrahepatic lipids [30]. Additionally, patients with obesity have a higher metabolic clearance rate of GH, which further reduces the quantity of bioavailable GH [31].
A limited number of studies have been conducted on the relationship between BMI and rhGH therapy efficacy in children with GHD. Yang et al. studied the impact of BMI on therapeutic response in 460 patients with GHD. In comparison to our study, an additional group of patients with obesity (BMI ≥≥2 SD for age and gender) was created in Yang’s study. The patients with obesity in Yang’s study noted significantly greater height gain after 2 years of the therapy. This finding is consistent with our results showing that the excessive body weight group experienced greater height increase after the first year of therapy compared to the other groups. In Yang’s study, there was a negative association between BMI and peak-stimulated GH, implying that children with obesity had less peak-stimulated GH, raising the likelihood of an increased false-positive diagnosis of GHD [32]. Our research did not analyse the peak-stimulated GH, but it showed statistically higher IGF-1 levels in excessive body weight groups throughout the yearly assessments. This may imply that some patients in our excessive body weight group could have been falsely diagnosed with GHD.
Hawcutt et al., in a study on 213 children with GHD, found that an increase in height-SDS and IGF-1 SDS during the first year of rhGH therapy is related to a BMI SDS at the onset of treatment in children with GHD. This impact was most apparent when the patients did not exceed the 1.75 SD BMI threshold. Our research did not provide the same findings considering the increase in height-SDS. The disparity between our and Hawcutt’s research is most likely due to Hawcutt including additional subgroup for patients with BMI SDS ≥ 2.0 SD, whereas in our study this group of patients was classified as an excessive body weight group along with all patients with overweight (BMI SDS 1 ≥ SD). After the first year of Hawcutt’s study, IGF-1 SDS ≥ 2.0 SD was observed in 19/213 patients (8.9%), including 8/27 patients with obesity (29.6%), resulting in a mean IGF-1 SDS 90.5% greater in those within the cohort of BMI SDS ≥ 2.0 SD compared to the cohort of BMI SDS in the range –1.0 to 1.0 SD [33]. The BMI SDS ≥ 2.0 SD group had a threefold greater proportion of remarkably high SDS IGF-1, which, as previously stated, was due to a possible false-positive GHD test finding in some of the patients. Our results indicate a corresponding relationship regarding IGF-1 measurements.
What distinguishes our research from the previously mentioned studies is the 5-year-long follow-up period. A long study period may improve the quality of findings by reducing the significance of various dynamics of response to rhGH in the first years of therapy, as shown by Cole et al. [34]. The novel finding in our research is that, although BMI SDS correlates positively with height increase during the initial 2 years, as reported by Yang et al. and Hawcutt et al., this relationship reverses during the 5-year follow-up period [32, 33]. Our method of monitoring results is centred on the group rather than the individual. Our solution allows us to evaluate the overall shift in growth dynamics of complete BMI groups without considering the impact of individuals that moved in between groups throughout the study.
The growth hormone stimulation test is required to diagnose GHD in children; however, false-positive or false-negative findings can result in unnecessary or delayed treatment. The number of positive tests is determined by the prevalence of said condition in the test group and the test’s false-positive rate [35]. Regarding GHD, both the low frequency of the disease and the high rate of false positives imply a high possibility of a wrong diagnosis. The prevalence of GHD is rare – it is estimated to affect 1 in 4000 individuals worldwide [36–38]. Otherwise, the incidence rate of false-positive GHD diagnosis is common. Ghigo et al. estimated the false-positive rates to a single provocation test to be 0.33 in 472 normally growing children [39]. The studies mentioned above show the importance of precise diagnosis and may partly explain higher IGF-1 SDS in groups of the highest weight in previously mentioned studies, including our study. Furthermore, the possibility of unnecessary treatment is impliedHigher IGF-1 SDS in GHD patients may also be caused by using weight rhGH dosing instead of the body surface area approach [40]. The optimal rhGH dosing format is still being debated, but it is widely believed that variations between the 2 are only important in overweight or very young patients [41]. It is noteworthy that greater rhGH doses rarely result in increased patient’s height in comparison to normal doses. Randomised research conducted by Coelho et al. found no substantial difference in the end height of children with GHD between the 2 groups. The first group in the research received a normal rhGH dose (5 mg/m2/week), while the second group received a high rhGH dosage (10 mg/m2/week) [42].
According to Paediatric Endocrine Society agreement guidelines, the dosage should be between 0.16 and 0.24 mg/kg/week with IGF-1 levels taken into consideration and individualisation of subsequent dosing [43]. Because our study was conducted in Poland, our patients received doses of rhGH in the range of 0.1 to 0.33 mg/kg/week in accordance with the Polish Society of Paediatric Endocrinology guidelines, which falls within the presented global consensus range [16]. Patients from the excessive body weight group in our study received on average a dose of 0.1770 ±0.0323 mg/kg/week, which was significantly lower than the patients in the “normal-weight” group with a dose of 0.1923 ±0.0309 mg/kg/week. The dose difference did not prevent high SDS IGF-1 levels in the excessive body weight group. Thus, a shift in rhGH dosage strategy to one based on body surface area should be further explored, particularly when the patients are diagnosed with obesity.
The topic of excessive body mass has a multifactorial impact on rhGH treatment in GHD children [23]. Low physiological GH in adolescents with obesity, as well as reduced peak GH in stimulation tests, can contribute to a false-positive diagnosis of GHD [36–38]. The first years of treatment can then produce deceptively positive outcomes, with children growing faster than their peers of normal weight. Finally, incorrect rhGH dosing can result in elevated IGF-1 serum levels, potentially causing damage to the patient and straining the health care units’ rhGH therapy funding [39].
This study has several limitations. The most important one concerns the differences between the characteristics of the normal and excessive body weight groups. Children with overweight or obesity were usually older and had higher BA, had higher IGF-1 SDS, and had slightly lower rhGH doses compared to their peers with normal body weight. This creates a significant risk of bias and calls into question all our results. Children with overweight and obesity had the highest BA in the third and fourth years of treatment and may have already reached adult height and therefore stopped growing. The number of participants is also suboptimal. Although the overall quantity is satisfactory (n = 165), the number decreased with follow-up, reaching 33 after 5 years of follow-up. Our study may seem less reliable compared to studies involving larger numbers of patients. The single-centre, retrospective study design is also a limitation because the sample of participants may not be representative. The optimal method to assess the impact of body weight on growth velocity would be multiple regression. However, this test was impossible in our analysis because we failed to meet the assumptions.
Conclusions
This 5-year retrospective cohort study showed a significant effect of excess body weight on the outcomes of rhGH therapy in children with GHD. Overweight or obesity resulted in an increase in HV in the first year. However, long-term follow-up showed that excess body mass distinctly worsened the results of rhGH treatment. Further research is needed, especially to evaluate the possibility of a false-positive diagnosis of GHD and an appropriate rhGH dosing strategy in children diagnosed with overweight or obesity.

 POLSKI
POLSKI





