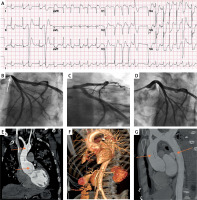
A 41-year-old man with a history of sarcoidosis was admitted with severe chest pain at rest with propagation in the arms and hypotension. Electrocardiogram on arrival showed diffuse ST depression and ST elevation in aVR and V1 leads (Figure 1 A). Emergency coronary angiography in a regional primary percutaneous coronary intervention (PCI) center showed an isolated, sub-occlusive lesion of the ostial left main (LM), which was treated with a zotarolimus-eluting stent (4.5 × 18 mm) (Figures 1 B–D). Intracoronary imaging was not performed at the time due to the patient’s instability, but was planned to take place during hospital treatment. Immediately after the intervention, the patient felt better, with relief of chest pain, resolution of ECG changes and a slight increase in blood pressure (maximum 115/70 mm Hg). Three hours after the procedure, the patient became hemodynamically unstable, with divergent arterial pressure (100/35 mm Hg), ultimately requiring inotropic stimulation. Echocardiography showed a small pericardial effusion (5 mm) and a dilatation of the ascending aorta (48 mm) with an intimal flap. Subsequent multislice computed tomography (MSCT) confirmed a type A dissection starting 1 cm from the aortic root with propagation through the thoracic and abdominal aorta ending in the left external iliac artery (Figures 1 E–G). Afterwards the patient was immediately transferred to a tertiary center where the emergency Bentall procedure was performed (the stent from the LM was not removed before reconnecting to the homograft). The postoperative course was complicated by acute kidney injury and right hemiplegia, both resolving during the hospitalization. Echocardiography at discharge showed a functional mechanical valve with a preserved left ventricular ejection fraction of 60% and the patient was discharged with warfarin and clopidogrel. The patient was asymptomatic and suffered no adverse events at the 1-year follow-up.
Figure 1
A – Electrocardiogram showed diffuse ST depression of more than 2 mm, premature ventricular complex, and ST elevation in aVR and V1 leads. B – “Critical ostial sub-occlusive lesion” in left main. C, D – Final angiogram after implantation of drug-eluting stent (4.5 × 18 mm) in ostial left-main. E–G – Multislice computed tomography (MSCT) indicated a type A aortic dissection, starting 1 cm from the aortic root with propagation through the thoracic and abdominal aorta ending in the left external iliac artery
Diagnosing acute Stanford type A aortic dissection with the uncommon involvement of the left main coronary artery remains challenging for physicians because it can resemble acute myocardial infarction with cardiogenic shock [1]. Some authors [2, 3] have suggested that in such cases the coronary angiogram not only led to the correct diagnosis, but also stabilized the patient prior to the definitive surgical management. Even in this case, stent implantation in the LM enabled ischemic stability of the patient and transport to the nearest cardiac surgery center, but in our opinion, non-invasive diagnostics such as echocardiography before urgent coronary angiography are crucial.
In an era of expanding regional primary PCI networks without on-site cardiac surgery availability, this case highlights the need for careful clinical evaluation and procedural planning in a young patient presenting with a baseline angiographic finding of an isolated ostial left main stenosis.








