A 75-year-old male patient was admitted to the Cardiology Department in July of 2024 due to exacerbation of chronic heart failure with reduced left ventricle ejection fraction (HFrEF), a subtype of pulmonary edema, and elevated blood arterial pressure. The medical history of the patient was: coronary artery bypass graft (2006); implantation of cardioverter-defibrillator (2020); open surgery for infrarenal abdominal aorta aneurysm with implantation of straight aortic prosthesis (2006); a branched endovascular abdominal aortic aneurysm repair (BEVAR) with Jotec VO 1234 aortic stent-graft and four stents – Jotec E-Ventus BX implanted to the celiac trunk, superior mesenteric artery, and right renal artery (RRA, 2 stents BX 91BX3709L-00) (2014); resection of a left kidney due to clear cell carcinoma (2000), and thermoablation of right kidney tumors (2017).
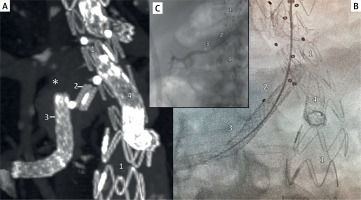
During the first 3 weeks of hospitalization, flash pulmonary edemas developed several times in the course of a sudden elevation of blood arterial pressure. Moreover, an increase in blood creatinine concentration (from 1.78 mg/dl at admission to 2.86 mg/dl) was observed. Because of progression of echocardiographic abnormalities, and severity of renal failure did not explain the paroxysmal (not continuous) rises in arterial blood pressure with flash pulmonary edema, the malfunction of right renal stent-grafts (e.g. partial thrombosis, stent-graft connection instability) was taken into account in the differential diagnosis. Doppler ultrasound showed turbulent flow at the renal stent-graft projection and flattened flow in the renal artery near the right kidney. Due to suspicion of renal branch disconnection as a cause of instability of the renal blood supply, computed tomography angiography was performed. It revealed total separation of the renal side-branch and bridging stent graft in the RRA, which had migrated about 15 mm from the main stent graft body, as well as an active inflow to the aneurysm sac (endoleak type IIIc), which provided the contrast-enhanced blood to the medial and distal part of the renal artery (Figure 1 A). Because the patient refused to be transferred to the vascular surgery center which performed BEVAR in the other hospital, the endoleak was repaired by angiologists in our hospital via brachial access. Using numerous catheters (Judkins R, Terumo 6F Guiding Catheter, Terumo NaviCross angled) and Terumo Guidewire Advantage 0.018′′, a migrated renal stent graft was cannulated and repositioned by traction of the balloon (Ultraverse 018 6 × 40 mm), keeping it inflated in the distal renal stent graft [1]. Next, separated renal stent grafts were connected by the BeGraft 7 mm × 57 mm stent graft (Bentley), and the correct route of blood flow to the right kidney was restored (Figures 1 B, C). After that, pulmonary edemas did not recur, and blood creatinine concentration decreased to the level at admission (1.73 mg/dl). The patient was discharged to the rehabilitation center. After 8 weeks of rehabilitation, the patient was discharged home with significant improvement in functional status. Until the end of 2024, the patient did not require hospitalization.
Figure 1
A – computed tomography angiography imaging before the procedure showing separated parts of renal side-branch; B – digital subtraction angiography after reposition of migrated renal stent graft; C – restoration of correct blood flow to the right kidney without endoleak type IIIc. Annotations: *contrast medium flow to aneurysm sac (endoleak) with dimensions: 51 × 25 × 78 mm; 1 – main body of aortic multi-branched stent graft, 2 – renal side-branch, 3 – migrated stent graft implanted in the right renal artery, 4 – superior mesenteric artery side-branch prolonged by stent graft
The presented case shows that acute renal artery pathology [2–4], including branch thrombosis or migration, should be considered as a reversible cause of recurrent pulmonary edemas and paroxysmal elevations of blood pressure, including in patients with more prevalent causes of hemodynamic instability, such as HFrEF.








