Introduction
The mediastinum is located between the lungs, the posterior sternum, the anterior of the vertebral column, the thoracic inlet and the diaphragm [1]. It is examined in three parts as anterior, middle and posterior mediastinum [2]. The mediastinum contains vital and vascular organs and very different histopathological tumors can be seen in this region of the thorax [3].
When the general patient population is considered, they are rare. It has been reported that it is asymptomatic at rates ranging from 9% to 17% at the stage of diagnosis in Chest Surgery and Chest Disease practice [4, 5]. In symptomatic patients dyspnea, cough and chest pain were the most common symptoms. Hormonally active tumors may present with secondary findings such as tachycardia or hypertension [6, 7].
Aim
In this study, we aimed to retrospectively evaluate the results of our patients with a primary mediastinal mass and the surgical techniques applied in our clinic.
Material and methods
Between March 2015 and March 2019, the results and treatment protocols of 32 patients with a primary mediastinal mass or cysts who were followed up and treated in our clinic were evaluated retrospectively. Patients were evaluated according to age, gender, symptoms at the time of presentation, physical examination findings, diagnostic examination methods, laboratory test results and pathology findings. Twenty-six patients who underwent surgery for biopsy or resection were included in the study. Patients who were referred for treatment with fine-needle aspiration biopsy or tru-cut biopsy and who had not undergone any surgical procedure for diagnosis or resection were excluded from the study.
Results
Sixteen of our patients (61.5%) were male and 10 (38.5%) were female. The mean age was 39 years (16–71). The mean age was 33.8 (16–62) in females and 42.3 (23–71) in males.
80.2% of our patients were symptomatic and 19.2% were asymptomatic and a mediastinal mass was incidentally detected in these patients. The most common symptoms were dyspnea with a rate of 38.4%, chest pain (30.7%), cough (26.9%) and voice hoarseness (26.9%). Fever was present in 6 (23%) and fatigue in 6 (23%) patients. The main symptom was palpitation (7.6%) in one patient with a posterior mediastinal mass diagnosed with pheochromocytoma. On physical examination, 1 patient had marked vena cava superior syndrome (VCSS). Tachycardia was observed in 1 patient, and wheezing and low eyelid were observed in one patient. The distribution of symptoms is given in Table I.
Table I
Distribution of symptoms at diagnosis (VCSS: vena cava superior syndrome)
| Symptoms | Number of patients (n = 26) | % |
|---|---|---|
| Dyspnea | 10 | 38.4 |
| Chest pain | 8 | 30.7 |
| Cough | 7 | 26.9 |
| Hoarseness | 7 | 26.9 |
| Fever | 6 | 23 |
| Weakness | 6 | 23 |
| VCSS findings | 1 | 3.8 |
| Palpitation | 1 | 3.8 |
| Low eyelid | 1 | 3.8 |
In all of our patients, radiological examination was performed by postero-anterior and lateral chest radiography after physical examination. When chest X-rays were evaluated retrospectively, 4 (15.4%) patients had no positive findings and 22 (84.6%) had a mediastinal mass. Contrast-enhanced thorax computed tomography (CT) was performed in all patients. Thorax magnetic resonance imaging (MRI) was performed in 1 (3.8%) patient, who was considered to have a neurogenic tumor. Positron emission tomography-CT (PET-CT) was used for diagnosis and staging purposes in 13 patients who were thought to have a malignant mass. In 11 patients, PET-CT diagnosed malignancy and 2 patients were reported to have benign lesions. The mean SUVmax value was 11.6 (5.3–20.1) in PET-CT imaging.
In terms of localization, 7 (26.9%) masses were on the right side and 5 (19.2%) were on the left side. In 13 (50%) patients, the mass originated from the anterior mediastinum, 7 (26.9%) from the posterior and 6 (23%) from the middle mediastinum.
Eight (30.7%) patients underwent anterior mediastinotomy and 1 (3.8%) patient underwent video-assisted thoracoscopic surgery (VATS) for biopsy. Eleven (42.3%) cases were diagnosed as malignant and 15 (57.7%) were diagnosed as benign. One patient diagnosed with thymic carcinoma underwent surgical resection after neoadjuvant chemotherapy treatment. Four lymphoma patients were treated with chemotherapy alone.
In a patient with primary anterior mediastinal seminoma, no residual mass remained after chemotherapy and therefore no surgical resection was considered. Pathology results of the patients are given in Table II. The most common pathological origin was the thymus (9 patients, 34.6%). The most common benign lesion was bronchogenic cyst (5 patients, 19.2%) and the most common malignant lesion was lymphoma (4 patients, 15.3%).
Table II
Pathology results of patients and mediastinal localization of masses
When surgical techniques were evaluated, the rate of excision with VATS was 57.7% (15 patients), thoracotomy 11.5% (3 patients), sternotomy 7.6% (2 patients) and VATS supported anterior minithoracotomy 3.8% (1 patient). There was no postoperative mortality in our series. In the postoperative morbidity, we observed diaphragmatic eventration in 1 patient and we performed plication surgery on this patient. Surgical techniques for excision of tumors and cysts are shown in Table III.
Discussion
Although primary tumors and cysts of the mediastinum are seen in almost every age group, they are most common in the third decade [8]. In our case series, contrary to the literature, the average age was 39 and the most common group was the fourth decade. Six of our patients (23%) came from abroad for treatment, especially from northern Iraq, and their mean age was 59.6 years. We think the reason for the high average age in our study was the high average age in the patients coming from abroad. We see that the patients in this group are diagnosed at an advanced age because of the poor development of the countries they come from and the insufficient diagnostic methods. In the literature, male sex was reported to be more frequent, and in our study, male gender was found to be 61.5% in 16 patients.
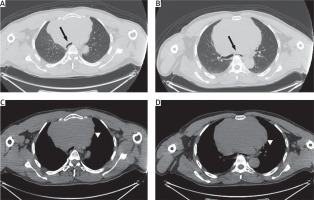
The majority of patients with mediastinal cysts or tumors are symptomatic [8, 9]. In the Çakan et al. [9] study, 83% of the patients were found to be symptomatic. They may come with different symptoms depending on the location of the tumor. The most common findings are compression of the surrounding organs. Findings such as shortness of breath, hoarseness, dysphagia, or chest pain can be detected. As a result of tracheal compression, we can see a flattening in the spirometry curve revealing a plateau sign [10]. In our patient with a diagnosis of primary anterior mediastinal seminoma, severe tracheal and bronchial compression was present (Figure 1) and there was a plateau sign in spirometry. In our study, 80.2% of our patients were symptomatic and were admitted to hospital due to dyspnea (38.4%).
Figure 1
A, B – Parenchymal window of the thorax CT showing compression of the mass to the trachea and the main bronchi (arrows). C, D – The mediastinal window of the thorax CT showing a mass of about 15 cm in the anterior mediastinum (arrowhead)
Postero-anterior and lateral chest radiography is the first step for diagnosis of mediastinal tumors. Afterwards, contrast-enhanced thorax CT, magnetic resonance imaging, positron emission tomography or scintigraphy can be used depending on the origin or location of the mass. Yasaka et al. [11] proposed the use of contrast-enhanced thorax CT in masses involving the anterior mediastinum in their study of 76 patients. They demonstrated that contrast-enhanced thorax CT has high specificity and sensitivity in the separation of solid and cystic masses. Contrast-enhanced CT is recommended for imaging of mature teratoma, mediastinal seminomas and mediastinal cysts [12].
Magnetic resonance imaging (MRI) is useful in demonstration of thymus hyperplasia and in the differentiation of thymic tumors. In contrast to noninvasive thymomas, invasive thymoma and thymic carcinomas have a more aggressive growth pattern. Local invasion and pleural invasion are a sign of invasive thymoma and can be clearly demonstrated by MRI [13, 14].
In our series, lymphomas were the most common malignant tumor with 4 patients (15.4%). Takahashi et al. evaluated MRI and MRI in their studies evaluating contrast-enhanced CT, especially to evaluate the response of lymphomas after treatment and to show the presence of a residual mass [15]. MRI imaging is also useful in the diagnosis of neurogenic tumors such as schwannoma and paraganglioma. MRI findings of neurogenic tumors such as Schwannomas show hypointense or isointense on T1 images and high non-homogeneous signal intensity on T2 images [16, 17].
PET CT is recommended when malignant and benign discrimination is required in mediastinal tumors. In the Tatci et al. study, the sensitivity of PET CT was 90% and the specificity was 55.17%. To distinguish malignant and benign lesions, the cut-off value of SUVmax was reported to be 4.67 [18]. The highest SUVmax value of our patients’ PET-CT results was 20.1, and the mean SUVmax value was 11.6. We present PET-CT images before and after chemotherapy in our patient with primary mediastinal seminoma in Figure 2. He received 6 cycles of bleomycin, etoposide and cisplatin chemotherapy and then we found that there was a complete response in the mass with control PET CT (Figure 2).
Figure 2
A, B – Axial and coronal sections of the PET CT showing high FDG uptake in the thyroid tissue and mediastinal mass (arrow). C, D – After chemotherapy PET-CT scan showing the full response in the mediastinal mass

Surgery is the mainstay of treatment for mediastinal cysts and tumors. There are different surgical approaches according to the location of the tumor. Thoracotomy, median sternotomy, VATS or robotic surgery techniques can be used in anterior and middle mediastinal masses [ 19–23]. VATS, thoracotomy or robotic surgery can be performed in the posterior mediastinal mass or cyst surgery [21–23].
Wang et al. [22] reported that they successfully performed mediastinal bronchogenic cyst excision with VATS in 108 patients. This case series, in which they shared their experience, required thoracotomy in only one patient. Li et al. [23] reported that robotic surgery could be used in all mediastinal areas in a series of 167 patients [23]. In our case series, VATS excision was performed in 15 (57.7%) patients and surgery was performed with VATS-assisted minithoracotomy in 1 patient. Gossot et al. [24] have shown that VATS can be used reliably even in bulky mediastinal masses.
Conclusions
The role of robotic surgery and VATS-assisted surgery is increasing due to technological advances in surgery techniques. In addition, the rate of demanding minimally invasive surgical techniques increases with the increasing level of consciousness of the patients. With the publication of series with high numbers of cases, robotic and VATS surgery will be more frequently used as reliable techniques. In the surgical evaluation of mediastinal tumors, prospective studies with higher numbers of cases are needed.






