Introduction
Myocardial bridging (MB) is an intramuscular course of a normal epicardial coronary artery first identified by Reyman in 1737 in autopsy series. In 1960, angiographic features were defined by Portman and Ivigin [1]. The ratio of MB in the general population varies in the range 0.5–4.5% in angiography series and 15–85% in autopsy series [2–4]. In addition, it constitutes 76.9% of left anterior descending (LAD), 10% of right coronary artery (RCA) and 6.7% of left circumflex (LCX). It usually appears in the mid-section of the LAD coronary artery (46.7%) [4–6].
MB is often considered a harmless anatomical variant of the coronary artery. But MB can cause myocardial ischemia, rhythm disorder and sudden death [7–10].
In the diagnosis of MB, catheter coronary angiography is the gold standard. Low detection of MB in coronary angiography may be because of superficial bridging. Coronary angiography and intravascular ultrasound (IVUS) are invasive methods and involve various risks. In addition, both methods are costly and are not routinely used in clinical practice. Multi-detector computed tomography (MDCT) coronary angiography is rapid and sufficient for diagnosis. MDCT can evaluate the course of coronary artery and its relationship with other anatomical structures [11, 12].
Aim
The goal of this study was to assess the incidence, localization, depth, length of MB with LAD, systolic compression ratio, atherosclerotic plaque localization and degree of stenosis by 256-slice MDCT.
Material and methods
Study population
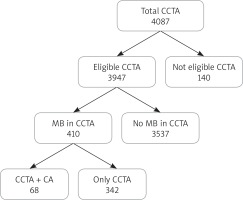
The retrospective study was done in our university’s Radiology Department. This study was confirmed by the ethics council of our university. The patient population comprised 410 consecutive patients (159 female; 251 male, mean age: 55.99 ±12.24 years; range: 16–90 years) who underwent coronary angiography with MDCT. Patients were sent for MDCT angiography because of clinically suspicious coronary artery disease. Patients with atypical chest pain, family history of coronary artery disease, smoking, high cholesterol and lipid levels, previous coronary artery disease and coronary CT angiography were included in the study. Exclusion situations for MDCT were decided as allergy to iodinated contrast agent, gravidity, renal failure and arrhythmia. Non-diagnostic images were excluded from this study. 140 patients were excluded because of inadequate imaging due to patient characteristics (obesity, respiratory incontinence and high pulse) and movement artifacts. The study flow chart is shown in Figure 1.
MDCT imaging protocol
MDCT images were obtained using a 256-slice dual energy CT scanner (Siemens Definition Flash, Berlin, Germany). The imaging parameters were 256 × 0.75 mm detector collimation, pitch 0.23, rotation time 400 ms, tube voltage 120 kV and current 320 mAs. ECG-induced tube current modulation was performed in rhythmic heart beats. During the middle inspiratory breath-hold, the single scan direction was craniocaudal. The scan range covered all the heart to the diaphragm of the tracheal bifurcation level. A bolus of 100 ml of iodinated contrast medium ioversol (Optiray 350 mg/ml; Guerbet, France) was administered intravenously to an antecubital vein at a flow rate of 5–6 ml/s using a double-headed power injector. Then 50–60 ml of salt solution (5 ml/s) was given. The imaging was started automatically by applying the “sure start” method (left atrium, threshold 130 HU). If the heart beat is greater than 65 beats per minute, oral β-blockers are given before MDCT screening.
Image analysis
Retrospective reconstructions were used in whole cardiac phases with 10% steps of the R-R interval. Images were reconstructed with a slice thickness of 0.75 mm, a reconstruction increase of 0.3 mm, image matrix 512 × 512, and an field of view (FOV) of 180–240 mm. Data were transferred to the Syngo Via workstation (Siemens, Berlin, Germany). A diastolic and systolic dataset with the best image quality was selected. Images were restructured using multiple post-processing methods. Transverse source images, multiplanar reformations (MPR), curved multiplanar reformations and maximum intensity projection images were used for evaluating the intramyocardial course. Myocardial bridge was defined as the coronary artery with intra-myocardial course. MDCT images were assessed by single radiologists experienced in cardiovascular radiology.
Myocardial bridging was divided into two types: ‘deep’ and ‘superficial’. Deep myocardial bridging was identified as full LAD (depth ≥ 2 mm) (Figure 2) surrounded by myocardium. Superficial bridging was defined as the surface not completely covered by myocardial fibers (depth < 2 mm) (Figure 3) [13, 14]. Location of the LAD (proximal, middle, and distal) MB segment was saved. The length and depth of the bridging segment were calculated with the digital caliper on the curved MPR. The diameter of each bridging segment was measured at the end of the diastolic and systole phase in curved MPR. The systolic compression difference and percentage were calculated from the average of the measurements in two different phases. For each bridged segment, the presence of atherosclerosis was saved in a 2-cm-long part proximal to the entrance of the bridging segment. The degree of stenosis made by atherosclerotic plaques was determined. It was defined as mild stenosis below 50%, moderate stenosis of 50–70% and severe stenosis over 70%.
Results
A total of 3947 patients who underwent coronary CT angiography in our hospital between 2017 and 2019 were retrospectively evaluated. LAD myocardial bridging was detected in 410 (10.4%) patients. The mean age of the patients was 55.99 ±12.24 years. Demographic and plaque characteristics of patients with LAD MB are shown in Table I. Table II shows location and depth type of myocardial bridging in LAD coronary arteries. Depth, length, systolic and diastolic coronary artery diameters of LAD myocardial bridging are given in Table III. The systolic and diastolic mean diameter difference was 0.193 mm and the average compression ratio was 9.44%.
Table I
Demographic and atherosclerotic plaque characteristics of patients with myocardial bridges in LAD coronary arteries
Table II
Location and depth type of myocardial bridging in LAD coronary arteries
| Myocardial bridging | n | % |
|---|---|---|
| Location: | ||
| Proximal | 6 | 1.5 |
| Middle | 366 | 89.3 |
| Distal | 38 | 9.3 |
| Type: | ||
| Deep | 97 | 23.7 |
| Superficial | 313 | 76.3 |
Table III
Measurements of myocardial bridging in LAD coronary arteries
| Parameter | Mean ± SD | % |
|---|---|---|
| Dept [mm] | 1.72 ±1.11 | |
| Length [mm] | 20.28 ±9.63 | |
| Systolic [mm] | 1.82 ±0.17 | 9.44 (0.193 mm) |
| Diastolic [mm] | 2.02 ±0.19 |
Atherosclerotic plaques were found in 167 (40.7%) of 410 LAD MB. Atherosclerotic plaques were found in 50.5% of deep MB and 37.7% of superficial MB. 76.2% of atherosclerotic plaques were calcific, 15.5% soft and 17.4% mixed. Atherosclerotic plaques caused mild stenosis in 75.5%, moderate stenosis in 14.4% and severe stenosis in 10.2% (Table I). Ninety-one percent of atherosclerotic plaques were present in the middle segment MB, 7.2% distal and 1.8% proximal MB.
Discussion
In many studies, LAD bridging rates and depth types differ according to race, geographic region, and gender. Jin et al. [13] detected LAD myocardial bridging in 557 (42%) patients in their study in 1275 patients. Superficial MB was found in 368 (66%) patients and deep MB in 189 (34%) patients. Superficial MB was complete in 128 (35%) and incomplete in 240 (65%). Jodocy et al. [14] found LAD MB in 51 (23%) of 221 patients. Aydın et al. [15] found LAD MB in 41 (21.5%) patients in their study in 191 patients. In this study, the deep MB ratio was 39% and the superficial MB ratio was 61%. Çay et al. [16] found 316 patients with myocardial bridging among 25 982 patients. Total prevalence was 1.22%. Although myocardial bridging had lesions in the left anterior descending coronary artery as expected in 96.52% of patients, the distribution of the bridging in the middle and distal regions was almost equal (52.9% and 47.21%, respectively). In the study of Ma et al. [17], MB was detected in the LAD in 325 (13.2%) of 2462 patients. The LAD MB rate was 60.4% among MB patients. Donkol and Saad [18] found MB in 89 of 350 patients. 76.4% of these MBs were in the middle LAD and 14.6% were in the distal LAD. In this study, 46 (61.3%) LAD MB were superficial and 29 (38.7%) were the deep type. Atar et al. [19] found MB in 25 of 165 patients. Among these, LAD MB was detected in 21 (60%) patients. In our study, a total of 4100 coronary CT angiographies were evaluated retrospectively. The mean age of the patients was 56 years. 61.2% of the patients were male. LAD MB was detected in 410 (10%) patients. Among these, LAD MD was detected in the proximal segment in 8 (1.5%) patients, in the middle segment in 366 patients (89.1%), and in the distal segment in 38 (9.3%) patients. Among these, 97 (23.7%) patients had deep and 313 (76.3%) patients had superficial course.
Depth, length and systolic-diastolic diameters and compression percentage of myocardial bridging are important for the development of symptoms. Ma et al. [17] found that the mean length of LAD MB was 18.1 ±6.1 mm and the depth was 2.9 ±0.8 mm. They found that arterial diameter in the ED phase was 2.6 ±0.5 mm and ES artery diameter was 1.5 ±0.3 mm. The change in mean systolic-diastolic diameter was 1.1 ±0.4 mm and compression percentage ranged from 34.9% to 50%. In the study of Ercakmak et al. [20], MB length was found to be between 8 and 50 mm and depth between 0.7 and 4.5 mm in CT angiography. Jodocy et al. [14] found that the LAD MB length was 14.9 ±6.5 mm and the depth was 2.6 ±1.6 mm. They found an average reduction in arterial diameter in the systolic phase of 27% and in the end diastolic phase of 15%. They detected luminal narrowing above 50% in 8% of patients. Zhang et al. [21] found that the narrowing of the arterial lumen was between 14% and 36% on average. In the study of Donkol and Saad [18], mean length of MB was 15 ±7 mm (min.–max. 6–24 mm) and mean diameter was 3 ±3 mm for the LAD. Dynamic compression was observed in 35 patients. However, no signs of hypoperfusion were observed. Chen et al. [22] found as 21.1 ±7.3 mm and 3.60 ±1.47 mm in the middle segment, and 22.1 ±10.8 mm and 3.12 ±2.39 mm in the distal segment the mean LAD MB length and depth. Hwang et al. [13] found a superficial length of 16.4 ±8.6 mm in the LAD MB. The length of the deep MB was 27.6 ±12.8 mm and the depth was 3.0 ±1.4 mm. In our study, the mean LAD MB length was 20.28 ±9.63 mm and the depth was 1.72 ±1.11 mm. The mean systolic diameter reduction was approximately 10%. The clinical course of patients with LAD bridging has changed in terms of symptoms. Drug therapy was administered to those patients. After the administration of these drugs, the complaints of patients have mitigated, and patients’ life quality has increased.
There is a relationship between myocardial bridged coronary segments and atherosclerotic plaque. In the study of Hwang et al. [13], atherosclerotic plaques were associated with MB in 175 (31%) of 557 tunneled segments. In their study, most atherosclerotic plaques were located at the segment proximal to the MB segment, with a rate of 91%. Atherosclerotic plaques were found in 17 of the complete superficial type, in 29 of the incomplete superficial type, and in 41 of the deep type. In the study of Aydın et al. [15], the proportion of atherosclerotic plaques in the proximal segment of the LAD MB was 49%. Mild and moderate CAD was found in 11 and 9 cases respectively. Mixed atheroma plaques were seen in 17 of 20 cases. Soft plaques were monitored in only 3 cases. Atherosclerotic plaque and stenosis were not detected in the LAD bridging segment. Atherosclerotic plaques were found in 167 (40.7%) of 410 LAD MB. Atherosclerotic plaques were more frequent in deep MB than in superficial MB. Atherosclerotic plaques mostly caused mild stenosis. The moderate to severe stenosis rate was 24.6%. In the LAD MB middle segment, the rate of atherosclerotic plaque was higher than the others.
This study has some limitations. The first is that it is single-centered and retrospective. Second, intra-interobserver variability was not evaluated in the study.