Introduction
Wire localization (WL) is a needle method for locating lesions in the breast. It has been used as a standard of preoperative image-guided localization of non-palpable breast lesions since the early 1970s. The wire is placed on the same day as a surgical breast excision using ultrasound, mammography, magnetic resonance imaging (MRI) or computed tomography (CT). This technique limits radiological and surgical schedules in the early mornings [1–3]. It also requires following the dissection route as designed, which should not be changed. The wire can protrude from the patient’s skin, which will cause displacement. Besides its disadvantages, in many institutions it remains the primary technique because of low cost and accessibility worldwide. The rate of positive margins for wire localizations ranges from 20% to 70% [4]. Finally, some investigations have started to find better alternative localization techniques.
The first non-wire system was radio-guided localization (RGL) in the form of radio-guided occult lesion localization (ROLL) using radiolabeled albumin-based colloid with TC-99m injected into the tumor under ultrasound and stereotactic guidance. ROLL was first described as a possible alternative to WL in 1996 [5]. The second RGL method, known as radio-guided seed localization (RSL), was reported by Gray et al. in 2001 [6]. RSL uses a titanium seed radiolabeled with I-125 inserted into the tumor using the same guidance as ROLL. RGL overcomes many of the disadvantages of WL [7]. TC-99m, as well as I-125, can be placed before the day of surgery and detected by the handheld gamma probe to guide intra-operative identification and surgical resection [8]. Nevertheless, these techniques require a strict nuclear regimen, which is the main limitation for hospitals. It has been demonstrated that the method causes less pain and greater overall convenience for patients [9]. RSL has advantages over ROLL such as the possibility of mammographic or ultrasound confirmation of the site of implantation in relation to the tumor after placement of the I-125 seed and improvement in logistics of the operative planning because of I-125’s long half-life of 60 days compared to the TC-99m radioisotope, which requires injection into the tumor bed within 24 h of surgery [10]. The tumor-free margin rates range from 73% to 92.8% with RSL [7, 11]. In cases in which ROLL was performed, the tumor-free margin rate was 82.5–90%. Re-excision rates range from 7.2% to 21% with RSL, 12% to 25% with WL and 10.9% with ROLL [7, 12–14].
Recently, two new nonradioactive technologies have been developed for nonpalpable breast lesions. Both have received clearance from the Food and Drug Administration: SAVI SCOUT in August 2014 and Magseed in April 2016. The SAVI SCOUT (Cianna Medical, Aliso Viejo, California) uses a radar wave reflector which is activated with infrared light. The 12 mm radar wave-reflective device is percutaneously placed under imaging guidance (ultrasound or mammogram) up to 7 days before surgery. Mango et al. reported clear margins in a total of 8 bracketed cases [15]. The re-excision rates from initial publications with SAVI SCOUT range from 0% to 18.5%. Disadvantages of the technique include the possibility of nondetection after placement (2.0–2.5%) and that it cannot be placed at greater than 45 mm depth [16, 17].
Magseed (Endomag, Austin, TX) is a 1 mm × 5 mm magnetic metallic marker, which is preloaded within a sterile 18-G needle and inserted into the lesion up to 30 mm depth under mammographic or ultrasound guidance up to 30 days before surgery [18, 19]. The procedure is performed under local anesthesia. Immediately after, a mammogram confirms appropriate positioning. The seed is detectable using the Sentimag probe in the same way as the Sienna+ tracer in sentinel lymph node (SNL) biopsy. It can be detected from any direction, regardless of seed orientation. The Sentimag probe produces an alternating magnetic field which transiently magnetizes the iron oxide particles within the Magseed [20]. The probe shows a numerical count and produces an audio tone, which is related to the strength of the magnetic field and therefore to the distance of the seed in the tumor from the detector probe. Bracketing may be performed as long as the seeds are placed greater than 20 mm from one another. The seed is cylindrical with no barbs, has no moving parts and cannot be damaged when implanted [21]. The main advantage of the Magseed and SAVI SCOUT is that there is no associated radiation like that associated with radioactive seed localization. All the most important characteristics of these methods are presented in Table 1.
Table 1
Preoperative localization methods of nonpalpable breast lesions and surgical outcomes
| Method | Type of inserted material | Positive margin rates (%) | Advantages | Disadvantages |
|---|---|---|---|---|
| WL | Stainless steel wire | 20–70 [11] | Low cost | Placement on the same day as surgery Painful Possibility of protrusion and displacement Surgical positioning Worse oncoplastic effect |
| ROLL | Radiolabeled albumin-based colloid with TC-99m | 10–18.5 [7] | Placement within 24 h of surgery | Nuclear regimen |
| RSL | Titanium seed radiolabeled with I-125 | 7.2–27 [7, 11] | Placement before the day of surgery | Nuclear regimen |
| SAVI SCOUT | Wire-free radar | 10.3–15 [23, 24] | Placement up to 7 days before surgery Nonradioactive technology | Cannot be placed at greater than 45 mm depth |
| Magseed | Magnetic metallic marker | 7.5 [25] | Placement up to 30 days before surgery Nonradioactive technology | Sensing depth 30 mm [18] Bracketing seeds greater than 20 mm [21] |
Material and methods
The current lesion localization techniques in the Department of General and Minimally Invasive Surgery, Baptism of Poland Memorial Hospital in Gniezno, Poland, where the study was conducted, are WL and ROLL. On average, ROLL technique requires 60 min for placement one day before surgery and WL is placed in the early morning just before the surgery. Our surgeons have experience in all of these methods. Between November 2017 and May 2018, we scheduled 10 patients for the Magseed localization procedure. The mean patient age at the time of localization was 60.6 (range, 42–79 years) and the mean BMI was 27.74 (range 24– 39.3).
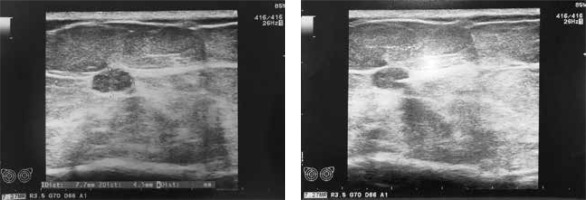
All Magseed markers (Endomagnetics Ltd, Cambridge, UK) were inserted with 18-gauge needle deployment under local anesthesia into the center of the target lesions under ultrasound guidance. The nonpalpable breast lesion on the left and the Magseed insertion process on the right are presented as an ultrasound image in Figure 1. Each procedure treated 1 lesion with 1 seed. The Magseed was placed in 100% of cases where intended and was simple to maneuver. On average, Magseed placement took 7.5 min. All seeds were placed successfully, and no seed migration was noted. The approximate depth of placement in post-insertion ultrasound was in 50% patients less than 30 mm and in the other 50% greater than 30 mm. In all cases of Magseed use, ultrasound was performed intraoperatively and confirmed Magseed findings in 100% of cases. The technique was evaluated by surgeons as easier than WL and ROLL. On average, from incision until specimen removal, it took 13.5 min. In 8/10 patients (80%) Sienna+ was used for SLN localization and in this group of patients in 5/8 cases (62.5%) the lesion was removed first before the nodes. The mean distance between the closest lesion and the Sienna+ injection site was 33.1 mm (range 20–45 mm). All Siena+ injections were subareolar, performed one day before the surgery, and were detectable with Sentimag through the skin. The mean number of removed sentinel nodes was 1.9 (range 1–3) and the mean Sienna+ count of the highest sentinel was 3738.75 (range 750–7600). No complication after the procedure was reported.
Fig. 1
Nonpalpable breast lesion on the left and the Magseed insertion process on the right ultrasound image
As presented in Table 2, wide local excision was performed in 100% of cases (10/10). The pathological examination found malignant lesions (9/10) in the majority of cases. In total, there was 50% invasive ductal carcinoma and 40% ductal carcinoma in situ. One patient had benign pseudoangiomatous stromal hyperplasia. Surgical specimen margins were evaluated in 90% as negative, with no additional re-excision. Only one patient with ductal carcinoma in situ had a positive tumor margin at the axillary side. No Magseed displacement was observed, and all seeds were removed intact, as shown on histology from 10 breasts.
Results and discussion
The findings of this single-center case study of Magseed demonstrate that it is an easy, sensitive and effective localization method. It improved scheduling efficiency and patient comfort. In comparison with needle techniques, there is no need to cut exactly where the needle was inserted, which influences the oncoplastic outcome. Although the primary goal of breast-conserving surgery is to achieve negative margins, the cosmetic outcome is essential for the patient’s quality of life. Co-usage of Magseed and Sienna+ was successful in 100% of cases and all surgeons asked in the survey would like to use them together again. Ease of placing a magnetic marker, its detection and margin rate results seem to be more beneficial than the isotopic technique used before. In our clinical practice, all seeds at all depths in the breast were detectable using the Sentimag probe intraoperatively. As well as Magseed, Sienna+ is nonradioactive, so they do not need to use special nuclear regimens, which allows more surgical centers to localize lesions and operate on them. Furthermore, the surgeons who inserted the seeds found it easy and similar to the insertion of a conventional biopsy marker. The disadvantage of this method is the price itself, but the total cost of nuclear requirement, operation delays and finally surgical outcome is thought-provoking. The limitation to the Magseed system may be placing a seed into the lesion at a depth greater than 4 cm. Also, the signals from multiple seeds placed in close proximity (< 2 cm) can be challenging to separate [22]. Our findings regarding the re-excision rate appear to be comparable to those reported in a prospective study on 200 patients with non-palpable invasive and in-situ breast carcinoma by Zacharioudakis et al. [23] where the same rate in the Magseed cohort was 16% and in the WL cohort was 14%. In another study evaluating Magseed localization of 73 nonpalpable breast lesions, there were positive margins in 12% of cases [22].








