Treatment of in-stent restenosis (ISR) may reach up to 5–10% of all percutaneous coronary interventions (PCI) [1]. ISR may occur despite significant improvements in stent technology and pharmacological treatment [2]. Excimer laser coronary atherectomy (ELCA) is considered to be advantageous for ISR treatment by debulking and softening the neointima, allowing lesions to be treated more effectively [3, 4].
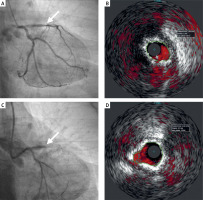
A 66-year-old female patient with a history of myocardial infarction, multiple PCI procedures, brachytherapy due to ISR, strokes, hypertension, and dyslipidemia was admitted to undergo invasive coronary diagnostics due to Canadian Cardiovascular Society grading of angina pectoris III. The coronarography revealed diffuse recurrent ISR in the left anterior descending artery (LAD) within previously implanted stents (Figure 1 A). Echocardiography showed hypokinesis of the lateral and anterior wall. The Heart Team determined that the patient was eligible for PCI. Revascularization was performed under intravascular ultrasonography (IVUS) guidance, showing diffusely narrowed and calcified neoatherosclerosis within the stent sandwich in LAD with moderate underexpansion (Figure 1 B). Repeated ballooning with non-compliant (NCB) and very high-pressure balloons (OPN) was ineffective. We decided to use ELCA with a 1.7 mm catheter. Several passages were performed using increased fluence and frequency up to maximal values (60 J/mm2 and 40 Hz, respectively) with a concomitant saline flush. Finally, the catheter could cross the lesion, causing a no-reflow event in the LAD, resulting in cardiac arrest: pulseless electrical activity (Figure 1 C). The patient was immediately intubated and resuscitated; pressors were also administered, and aspiration thrombectomy was performed. Moreover, intracoronary boluses of eptifibatide followed by intravenous infusions and adenosine via the thrombectomy device directly to the distal LAD were administered. After restoring blood flow and achieving the stable hemodynamic status of the patient, balloon angioplasty with NCB, cutting balloon, and OPN with subsequent implantation of a drug-eluting stent (3.0 × 15 mm) was performed at 20 atm, followed by OPN postdilatation up to 35 atm, with good results indicated by angiography and IVUS (Figure 1 D). Finally, the patient was discharged home with good left ventricle function. To conclude, ELCA is a valuable tool for treating calcified ISR; however, serious complications such as no-reflow may occur.
Figure 1
A – Coronarography showed diffuse restenosis up to 90% in and 50% below the stent. B – Intravascular ultrasonography performed before revascularization showed diffusely narrowed and calcified neoatherosclerosis within previously implanted stents in LAD with minimal stent area (MSA) of 3.69 mm2. C – No-reflow in LAD after the catheter crossed the lesion. D – Result in LAD in intravascular ultrasonography after revascularization with final MSA of 4.94 mm2