Introduction
The pathophysiology of aortic dilatation is unclear. It has been proposed that abnormal aortic stress as a consequence of pathological transvalvular flow as well as cellular and extracellular abnormalities of the aortic wall plays a key role in the formation of an aneurysm in the aortic root [1, 2]. Patients with aortic root diameter greater than 5 cm with or without aortic valve insufficiency undergo aortic root replacement. However, the surgical strategy for patients with moderate aortic root involvement remains controversial, especially in patients with high perioperative risk due to age and comorbidities [3].
In addition, it is a common scenario to come across a moderately dilated aorta in patients undergoing cardiac surgery for a different indication. Several institutions propose a prophylactic replacement of the aorta in such cases [4, 5]. The surgical strategy in these cases remains unclear. In our department a cutoff diameter of 5 cm is used for aortic replacement in cases like that.
Aim
We report aortic dimensions after cardiac surgery for a different cause in patients with coexisting aortic dilatation at the time of surgery and the progression of aortic root and aortic arch diameters after ascending aorta replacement with a Dacron prosthesis in an almost 5-year follow-up.
Material and methods
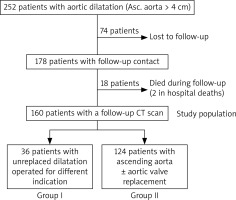
In the period from January 2010 to June 2019 a total of 252 patients with aortic dilatation (ascending aorta diameter > 4 cm) underwent cardiac surgery in our institution, excluding patients with Marfan syndrome or aortic dissection. A total of 61 patients – all of them with tricuspid valves – had an aorta of less than 5 cm and did not receive aortic replacement. In 191 patients (14 bicuspid valves) the dimension of the ascending aorta was greater than 5 cm and underwent ascending aorta replacement with a Dacron tube. Forty-seven of these patients also received aortic valve replacement for severe aortic stenosis or regurgitation.
Follow-up was performed with complete clinical examination and computed tomography (CT) angiography. Eighteen patients died during the follow-up period and were excluded from further analysis. One of these deaths occurred during reoperation for a false aneurysm of the distal tube to arch anastomosis. Another 74 (29.3%) patients were lost to follow-up and were also excluded from further analysis. The remaining population (160 patients) was divided into two groups according to the initial operation they received. Group I consisted of patients with a dilated aorta, unreplaced during cardiac surgery for a different indication. Group II included patients who received ascending aorta replacement with a tube graft with or without aortic valve replacement. In group I measurements of the aortic root, arch and ascending aorta from preoperative and postoperative CT scans were compared. In group II these comparisons concerned only the aortic root and arch. Figure 1 shows the flow chart of the study. Measurements of the aorta were made perpendicularly to its axis on reconstructed images of the CT scan at the levels of the sinuses of Valsalva, the ascending aorta at its maximal diameter and the aortic arch after the innominate artery. The mean follow-up was 47.8 ±29 months. Patients underwent a CT scan after informed consent was obtained. Timing of the CT scan after the operation varied amongst patients.
It is our policy to prescribe antihypertensive drugs as well as β-adrenergic blockers in all patients unless contraindicated in order to reduce the progression of aortic dilatation and prevent the onset of aortic complications.
Consent of the bioethics committee was obtained for this retrospective study.
Statistical analysis
Continuous data are presented as means ± SD standard deviation. Categorical variables are reported as numbers and percentages.
Preoperative and postoperative mean aortic diameters of the patients as measured on CT angiography were compared using the two-sided paired t-test for repeated measurements.
Results
Eighteen patients died during the follow-up period. Two (0.79%) patients died in hospital early after surgery and 16 (6.3%) patients died late during follow-up. Mean dimensions of the ascending aorta were: 4.2 ±0.03 cm for group I and 5.18 ±0.6 cm for group II.
Table I show causes of mortality during the follow-up period for both groups. One patient in this cohort needed a re-operation during the follow-up period for a false aneurysm on the distal anastomosis of a tube graft 4 years after ascending aorta replacement. This patient died during reoperation. No other death was due to a ruptured aneurysm, or in any way related to the aorta. Criteria for an elective re-operation were aortic root diameter and ascending aorta diameter greater than 5 cm or aortic valve insufficiency. These patients were excluded from the study.
Table I
Causes of death during follow-up for patients of group I and II. Percentages are expressed for all patients with a known follow-up status
Table II shows the basic preoperative characteristics and the evolution of aortic dimensions in patients with a dilated aorta having cardiac surgery for another reason. Mean ascending aorta and root diameters remained unchanged during the follow-up period whereas a small yet statistically significant increase in the mean arch diameter was noted. Table III shows basic preoperative characteristics and dimensions of the aortic root and arch in patients with replacement of the ascending aorta with or without valve replacement. The mean aortic root diameter showed a small but statistically significant decrease in its diameter during the follow-up period. The aortic arch dimensions however remained the same.
Table II
Basic characteristics and aortic dimensions of patients with a dilated aorta unreplaced during other cardiac surgery
| Group I | N = 36 | P-value |
|---|---|---|
| Age [years] | 67.3 ±10.9 | |
| Female sex | 1 (2.7%) | |
| Hypertension | 16 (44.4%) | |
| Diabetes mellitus | 7 (19.4%) | |
| Dyslipidemia | 8 (22.2%) | |
| COPD | 2 (5.5%) | |
| Stroke | 4 (11.1%) | |
| Ejection fraction | 55.9 ±10.2% | |
| Acute myocardial infarction | 7 (19.4%) | |
| CABG | 20 (55.5%) | |
| AVR | 16 (44.5%) | |
| Follow-up duration [months] | 40.8 ±29.3 | |
| Aortic root diameter [mm] preop* | 34.7 ±5.7 | 0.662 |
| Aortic root diameter [mm] postop* | 35.1 ±5.9 | |
| Ascending aorta diameter [mm] preop* | 43.2 ±2.6 | 0.615 |
| Ascending aorta diameter [mm] postop* | 43.5 ±2.9 | |
| Aortic arch diameter [mm] preop* | 30.3 ±4.1 | 0.005 |
| Aortic arch diameter [mm] postop* | 31.1 ±4.4 |
Table III
Basic characteristics and aortic dimensions of patients with ascending aorta aneurysm replaced by a tube graft
| Group II | N = 124 | P-value |
|---|---|---|
| Age [years] | 64.8 ±10.2 | |
| Female sex | 40 (32.2%) | |
| Hypertension | 101 (81.4%) | |
| Diabetes mellitus | 23 (18.5%) | |
| Dyslipidemia | 36 (29%) | |
| COPD | 19 (15.3%) | |
| Stroke | 24 (19.3%) | |
| Ejection fraction | 59.8 ±8.7 | |
| Acute myocardial infarction | 22 (17.7%) | |
| Aortic valve replacement | 47 (37.9%) | |
| Follow-up duration [months] | 50.94 ±31.1 | |
| Aortic root diameter [mm] preop* | 3.74 ±0.7 | 0.015 |
| Aortic root diameter [mm] postop* | 3.67 ±0.6 | |
| Aortic arch diameter [mm] preop* | 3.3 ±0.54 | 0.569 |
| Aortic arch diameter [mm] postop* | 3.32 ±0.47 |
Discussion
The 2010 American guidelines for thoracic disease of the thoracic aorta recommend concomitant aortic replacement at a diameter of 45 mm [6]. Replacement of the ascending aorta is a procedure with low operative risk under elective circumstances. Aortic root replacement with coronary ostia re-implantation includes an additional risk of complications such as bleeding, kinking of the coronaries, and false aneurysm formation, and has an operative mortality that ranges from 1.5% to 11.5% [6]. Decision making regarding the aortic root is complex and includes consideration of several factors such as the patient’s age and comorbidities, quality of aortic tissue, degree and rate of aortic dilatation, number of sinuses involved, patient’s preference of mechanical or tissue aortic valve, displacement of the coronary ostia, need for aortic arch reconstruction or for concomitant coronary artery bypass grafting, which may prolong the bypass time, and the likelihood of a redo operation or transcatheter aortic valve implantation in the future [7]. Most societies define an aortic aneurysm as an aortic diameter greater than 50–55 mm but also describe a grey zone of aortic diameters between 40 and 50 mm. Defining the normal aorta is quite complex and various factors such as age, somatometric characteristics and different genes determine what an abnormal increase in aortic diameter is and the actual risk of rupture for a specific patient. Although according to Laplace’s law the aortic wall tension depends on the diameter, wall thickness and pressure difference, various clinical studies have shown that aortic rupture and aortic dissection are not fully explained by aortic diameter alone. In 40% of patients with acute aortic A-type dissection the aortic diameter was < 40 mm and in 60% the diameter was < 55 mm. Moreover, 50% of patients with type A aortic dissection had a normal aortic diameter < 40 mm and none of the known risk factors [8].
After aortic replacement, careful follow-up and evaluation of patients is mandatory. It has been proposed that replacement of the ascending aorta with a non-compliant Dacron graft may increase the stress on the proximal non-treated aortic segment having as a result progressive dilatation and increased risk of wall dissection [9]. Simon-Kupilik et al. in an in-vitro model demonstrated that aortic replacement with a non-compliant Dacron graft could increase the systolic cross-sectional area of the aortic root and the calculated wall stress index thus resulting in late development of aortic root aneurysm [10]. Abi Akar et al. in a series of bicuspid aortic valve replacement patients reported that when the aortic root was not initially dilated the risk of secondary dilatation at 10 years was low, justifying its preservation in older patients [11].
In our study, we found a different pattern of evolution for the different segments of the aorta on CT angiography. The aortic root did not dilate over time when a moderately dilated ascending aorta was left in place, and its diameter was even slightly reduced when a tube graft replacement of the ascending aorta was indicated. This implies that a less aggressive approach towards the aortic root may be indicated in such cases.
Balci et al. in a study comparing pre- and postoperative echographic dimensions of the ascending aorta and the sinotubular junction in patients with CABG and a moderately dilated aorta found an increased expansion rate of these segments when a proximal anastomosis was constructed on the diseased aorta, proposing a disruption of the elastic structure and connective tissue of the aorta by the arteriotomy as a possible mechanism [12]. In contrast, we found that the moderately dilated aorta, unreplaced during cardiac surgery, did not dilate further during the follow-up period. Approximately half of the patients in our cohort had CABG and the rest of them were operated on for aortic valve replacement (AVR). In both types of surgery an arteriotomy is performed routinely. However, in these patients a small but statistically significant increase of the aortic arch diameter was found. When the ascending aorta had to be replaced by a tube graft the dimensions of the aortic arch remained unchanged. In our cohort, during follow-up, there were no late complications related to the aortic root, but 1 patient had to be re-operated on for a false aneurysm of the distal tube to arch anastomosis 4 years after ascending aorta replacement and died during reoperation. Our data suggest that the aortic arch may be more prone to future complications, requiring a closer follow-up.
The findings of our study are consistent with reports from other institutions focusing on aortic valve replacement surgery and comparing bicuspid and tricuspid aortic valves. Hui et al. reported that if the aortic root is not initially dilated the risk of future enlargement is minimal, and that therefore no prophylactic replacement is required in patients with bicuspid or tricuspid aortic valves [7]. De Paulis et al. suggested that aggressive treatment of the aortic root is justified only in acute aortic dissection because of progressive worsening of aortic valve insufficiency and an increase of aortic root diameter and not in chronic atherosclerotic non-dissecting aneurysms [9]. Idrees et al. in a recent propensity-matched study reported that prophylactic aorta replacement can be done without increasing patients’ mortality or the incidence of stroke. However, in their study patients receiving prophylactic replacement of the aorta had increased ventilation time, ICU and hospital length of stay as well as atrial fibrillation incidence [5]. Our results do not support aggressive treatment of the aortic root but do suggest a close follow-up especially of the aortic arch in these patients.
Most studies on the fate of the aorta postoperatively focus only on comparing patients with bicuspid versus tricuspid valves in need of replacement [11, 13–15]. Our study focused on patients who underwent ascending aorta replacement with or without AVR as well as on patients who underwent other cardiac surgery having moderate ascending aorta dilatation.
Several limitations to this study exist. The main limitation is the duration of follow-up. As aortic dilatation is time-dependent, it may be that a longer follow-up period will bring forth problems related with aortic disease in the future. Moreover, this study is limited by the completeness of follow-up. As 29.3% of patients were lost to follow-up, their health status could not be evaluated and it is possible that some of them experienced complications due to aortic disease. Finally the sample size was relatively small, and it may be that aortic measurements made it so that it was not possible to report a statistically significant increase in this time period. These results should be considered preliminary until they are confirmed by larger studies with a larger number of patients and more complete follow-up. We believe that a prospective study with complete imaging and monitoring for a longer period of time would yield some definitive results.
Conclusions
During a follow-up period of up to 10 years we found that in patients with moderate ascending aorta dilatation operated on for a different indication, the unreplaced ascending aorta and aortic root remained relatively stable but the aortic arch increased slightly during follow-up. Ascending aorta replacement with a tube graft remodeled the aortic root and did not allow progressive dilatation of the aortic arch. These data suggest a more conservative strategy regarding the aortic root but a vigilant approach to the aortic arch.