Summary
Coronary interventions substantiated by the physiological evaluation of coronary lesions are associated with better outcomes; therefore, they are supported by experts worldwide. Nevertheless, the use of physiological assessment methods remains insufficient, mainly due to procedure prolongation, increased dose of ionising radiation, and possible complications. This study was designed to identify the method associated with the lowest exposure to ionising radiation. A novel, minimally invasive fractional flow reserve value computation from an ordinary angiogram method – quantitative flow ratio (QFR) – has shown a significant reduction in expose to ionising radiation compared to pressure-wire-based methods. Hence, wider QFR application in clinical practice may safely increase the prevalence of physiology-guided revascularisation.
Introduction
The development of interventional cardiology increases the prevalence of invasive procedures which are inevitably associated with increased exposure to ionising radiation and associated risks for the physicians [1]. Despite adequate radiation protection, interventional cardiologists among all physicians working in radiology facilities receive the highest amount of ionising radiation [2, 3]. Seymour et al. estimated that during his or her career, an interventional cardiologist is exposed to a cumulative dose of ionising radiation equal to 10 000 chest X-rays [1, 4]. In contrast, for the most sensitive organ, the brain, the effect of the received dose of ionising radiation increases 5-fold [4], which could lead to increased risk of development of left side brain and neck tumours [5, 6].
A percutaneous coronary intervention (PCI) substantiated by the evaluation of coronary artery (CA) lesion’s functional significance is strongly recommended by both the European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EACTS) and the American College of Cardiology (ACC) [7–9]. According to the latest guidelines on myocardial revascularization, the method of choice for intermediate coronary artery lesions’ functional evaluation is fractional flow reserve (FFR) followed by an instantaneous wave-free ratio (iFR) [7–9]. They are pressure-wire-based methods extending the costs and the duration of the procedure [9]. Also, the necessity of a stiff wire insertion through a tight lesion might be complicated by a failure to pass through the lesion or in forceful manoeuvres by a plaque rupture, a CA dissection or perforation [9]. Moreover, an FFR measurement requires intravenous or intracoronary adenosine injection which occasionally may cause drug-related adverse reactions including dyspnoea, chest discomfort, bradycardia, atrioventricular blocks, ventricular arrhythmias, cardiac arrest, asystole and even death [10]. An iFR is advantageous due to redundancy of adenosine due to exploitation of the natural heart cycle hyperaemic phase [11]. Its performance and agreement with FFR has been proved in numerous clinical trials [12, 13]. Nevertheless, the application of pressure-wire-based methods remains extremely low and, in the best scenario, does not exceed 10% of all PCIs all over the world [9, 14–16]. Seeking a functional evaluation method that is as non-invasive as possible, a novel minimally invasive quantitative flow ratio (QFR) method based on three-dimensional (3D) coronary artery reconstruction from an ordinary diagnostic coronary artery angiography (CAG) images and FFR value computation by applying specific mathematical equations was developed a couple years ago [9, 15–17] and has demonstrated promising results. Previous studies have proved excellent agreement separately between FFR and both iFR and QFR [9, 12, 13, 15–26]. However, the data comparing all three methods at any aspect are scarce. Hence, we designed this study to compare the dose of ionising radiation received during diagnostic CAG accompanied by performance of FFR, QFR or iFR for CA lesions’ physiological evaluation.
Aim
To compare the dose of ionising radiation received during CAG accompanied by performance of FFR, QFR or iFR for CA lesions’ physiological evaluation.
Material and methods
Study population
After study approval by the Regional Ethical Committee, anonymized data of 421 patients who were admitted to our hospital due to stable angina pectoris between 1st January 2018 and 1st March 2020 were prospectively included in our single-centre observational study. For all included patients, an elective CAG followed by functional assessment of intermediate (lumen diameter stenosis of 35–90%) CA stenosis was performed. For the physiological evaluation, one of three methods (FFR, QFR, or iFR) was chosen according to the operator’s preference.
All included patients met all the inclusion criteria given in Table I. Patients who did not meet at least one inclusion criterion were excluded from the analysis.
Coronary angiography technique
CAG was performed in standard fashion, obtaining images after intracoronary nitrate administration. The right radial approach was chosen for all procedures. All CAGs were performed using GE Healthcare Innova Cardiovascular Imaging System machines. Standard coronary artery angiograms in our catheterization laboratory employ certain angulations including anteroposterior (AP) caudal (about 30°) and AP cranial (about 30°), left anterior oblique (LAO) cranial (both between 20° and 30°), right anterior oblique (RAO) cranial (both between 20° and 30°) and RAO caudal (both between 20° and 30°) for the left coronary artery and LAO cranial (both between 15–30°) and AP cranial (about 20°) or RAO cranial (both between 10–30°) for the right coronary artery. For QFR analyses, dedicated angulations [27] were acquired if necessary. The chosen frame rate of 7.5 frames per second is used for fluoroscopy and 15 frames per second for cinematography modes. A standard diagnostic CAG procedure was followed by a physiological evaluation procedure.
Physiology evaluation techniques
After engagement of the 6F guide catheter, the pressure wire was placed at the aortic ostium of either the right or left coronary artery under fluoroscopy mode guidance, and then the calibration and equalization to aortic pressure were performed. Later, the pressure wire was placed distally to the index lesion. The position of the wire was recorded in cinematography mode. In total, 0.28 mg of intracoronary adenosine were injected for maximal hyperaemia induction during every FFR measurement. After 5–10 s, the FFR was recorded. Then the guiding catheter was flushed with saline, and the FFR measurements repeated twice more. When performing iFR measurements, intravenous adenosine injection was omitted. A pullback record was performed in both FFR and iFR measurements. Online QFR analyses were performed using the certified software package QAngio-XA 3D, version 2.0 (Medis Medical Imaging Systems, Leiden, The Netherlands) from coronary artery angiograms, acquired following previously described recommendations [24]. All functional assessments were performed by an experienced interventional cardiologist and repeated at least three times to avoid any possible mismatches; averaged values were included in the analysis.
Measures of ionising radiation dose
The ionising radiation dose was evaluated by dose area product (DAP) and total fluoroscopy time (FT). Data were collected from index diagnostic procedure protocols obtained from the local database.
Only diagnostic-procedure-related data were analysed; hence the dose of ionising radiation exposed during PCIs was not included in the analysis.
Statistical analysis
Categorical data were presented as numbers and percentages. Continuous variables were normally distributed, presented as mean with standard deviation (±) and were compared using the unpaired Student’s two-sided t-test. One-way ANOVA was used to assess potential differences between groups. Statistical analysis was performed using the software package SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The chosen level of significance was p < 0.05.
Results
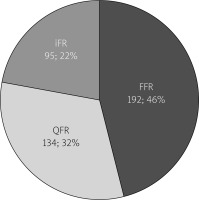
Of all 421 investigated procedures 192 (45.6%) were FFRs, 134 (31.8%) were QFRs and 95 (22.6%) were iFRs (Figure 1).
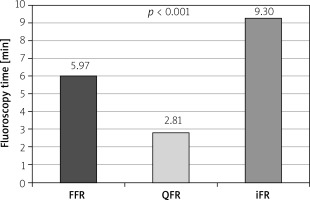
The mean FT was 5.97 ±0.32 min in the FFR group, 2.81 ±0.23 min in the QFR group, and 9.30 ±0.62 min in the iFR group (Figure 2). Compared to FFR as a reference, FT was almost half in QFR and almost double in iFR, p < 0.001. Moreover, it was found that the duration of QFR analyses is more than 3 times shorter compared to iFR measurements, p < 0.001.
Figure 2
Comparison of fluoroscopy time in FFR, quantitative flow ratio and instantaneous wavefree ratio groups
The mean DAP was 2040.57 ±151.64 cGy/cm2 in the FFR group, 1587.85 ±136.76 cGy/cm2 in the QFR group and 2251.72 ±211.77 cGy/cm2 in the iFR group (Figure 3). DAP was lower in QFR compared to iFR with the mean difference of 663.87 ±260.51 cGy/cm2, p = 0.03. No significant differences between other groups were found. The study design and results are summarized in Figure 4.
Figure 3
Comparison of dose area product in FFR, quantitative flow ratio and instantaneous wavefree ratio groups
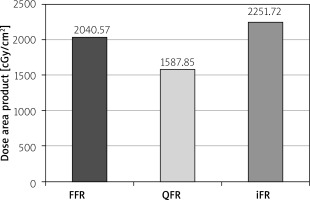
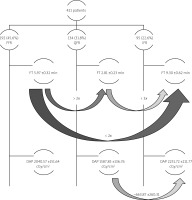
Figure 4
Schematic study methods and results. Curved arrows mark the direction of comparison between two physiological assessment methods, number above the arrows shows either fold difference or numerical expression of the difference between compared values
DAP – dose area product, FFR – fractional flow reserve, FT – fluoroscopy time, iFR – instantaneous wave-free ratio, QFR – quantitative flow ratio.
Discussion
Development of interventional cardiology with an increasing number of procedures over the past decade [27–30] is inevitably associated with increased requirement for physiology guidance of PCI [7, 8]. The use of any of pressure-wire-based physiology evaluation method (FFR or iFR) remains limited in clinical practice, likely due to the requirement of stiff pressure-wire intracoronary instrumentations and its association with complications in addition to prolongation of the procedure time and increase of the economic aspects [9, 31–34]. The newly developed wireless FFR value computation method QFR seems to be beneficial due to the lack of need of adenosine injections and intracoronary instrumentation of pressure-wire resulting in a shorter procedure and fluoroscopy time [9], which was double in the FFR group and three times longer in the iFR group compared to QFR analysis in this study. Moreover, FT compared to FFR was almost double in iFR, most likely due to intracoronary instrumentation with a stiffer, less torque and less flexible pressure-wire dedicated for iFR. It normally takes longer to pass through tight lesions with stiffer wire. This QFR benefit might be explained by the lack of need of any intracoronary manoeuvres under fluoroscopy guidance [15, 24, 35]. That certainly results in shorter FT and lower DAP. It is known that DAP is closely related to angiography technique and patients’ body constitution. Unfortunately, patients’ physical characteristics were not included in this analysis. Accordingly, associations between the body constitution and exposure to ionising radiation were not investigated. Therefore, DAP was considered as a less reliable parameter for evaluation of the ionising radiation dose associated with the used physiological evaluation method in this study. Nevertheless , DAP was lower in QFR compared to iFR. A higher dose of ionising radiation is necessary to obtain appropriate quality angiograms for patients with increased body mass index (BMI), especially when BMI is over 30 kg/m2 [3, 36, 37]. Cinematography mode requires the double frame rate compared to fluoroscopy mode; therefore cinematography replacement by fluoroscopy is supported by several scientists [38]. Even though significantly longer FT in FFR and iFR groups, possibly due to intracoronary instrumentations of pressure-wire, it can be assumed that proper angiograms may reduce FT and DAP in addition to a shorter overall procedure time when QFR is chosen for physiology evaluation [15, 18–26]. The use of QFR could reduce to the minimum the amount of additional ionising radiation during physiological assessment procedures without loss of diagnostic accuracy [15, 18–26]. Eventually, the application of QFR significantly reduces total FT compared to pressure-wire-based methods and substantially reduces the total procedure time [35]. Wider application in clinical practice of QFR as a preferred physiology-evaluation method, in addition to the increase of physiologically guided PCI, could eliminate any additional exposure to ionising radiation warranting the highest level of radiation protection for interventional cardiologists.
Despite its novelty comparing the exposure to ionising radiation during coronary artery physiological assessment procedures, the study has certain limitations. Data on patients’ body constitutions and the number of diagnosed vessels were not included. Hence, we were not able to validate the impact of BMI on ionizing radiation increase during interventional procedures. Furthermore, the desire to reduce the exposure to ionising radiation during physiology assessment procedures raised the hypothesis of a possibility to perform qualified QFR analysis using images acquired under fluoroscopy mode. This is the subject for further studies. The study is being continued, including omitted parameters.
Conclusions
Physiological assessment by QFR, in addition to its reproducibility, convenience, and accuracy, is associated with significantly reduced exposure to ionizing radiation compared to both FFR and iFR. Therefore, wider QFR application in clinical practice and consideration of it as the first-choice method for physiological evaluation, in addition to increase of physiology-guided coronary artery revascularization, could eliminate any additional exposure to ionizing radiation. Moreover, acceptance of standard QFR projections in routine clinical practice may enable wider use of the method and may significantly enhance QFR benefits.