Introduction
Oral squamous cell carcinoma (OSCC) is the most prevalent type of oral cancer. Diagnosing OSCC at an early stage (I or II) is crucial for treatments to be effective, and it results in better outcomes. Nevertheless, OSCC is frequently diagnosed at an advanced stage; hence, multimodal treatment with a personalized approach including surgical resection, radiation therapy, and systemic treatment (chemotherapy and immunotherapy) is indicated to improve outcomes [1–3]. Identification of new prognostic markers for better risk stratification in OSCC may help to adjust treatment in individual cases.
Galectins are a group of β-galactoside-binding proteins responsible for cell adhesion and regulation of proliferation [4]. Their role in carcinogenesis, cancer progression, and potential use in cancer therapy is being investigated. Moreover, they exhibit various functions on immune cells either promoting an inflammatory response or silencing T-cell mediated actions [4]. One of them, galectin-9, is a tandem-repeat type galectin with 2 carbohydrate recognition domains identified in a plethora of epithelial and immune cells. Like other galectins, it regulates various intra- and extracellular processes because it is located inside cells (in the cytoplasm and the nucleus) and along the plasma membrane. During oral cancer development, the intracellular distribution of galectin-3 and galectin-9 changes as it shifts from the nucleus to the cytoplasm [5, 6]. Additionally, galectin-9 induces apoptosis, inhibits cell proliferation in some tumours, and its expression is generally decreased in cancer when compared to healthy tissues [7]. Extracellularly galectin-9 may crosslink PD-1 and T-cell immunoglobulin and mucin domain 3 (TIM-3) to form galectin-glycoprotein lattices regulating T-cell death [8]. In consequence, it leads to exhausted T-cell persistence and modulates the tumour micro-environment (TME) [8]. On the other hand, tumour-derived galectin-9 may attract eosinophils and result in enhanced anti-tumour activity [7]. Importantly, galectin-9 is believed to be a promising target for immune therapy [8].
To date, galectin-9 has been investigated in various types of head and neck malignancies. Fík et al. demonstrated its loss in squamous cell carcinoma of the palatine tonsils, the base of the tongue, larynx, pharynx, soft palate, and oral floor [9]. Similarly, another study postulated that down-regulation of galectin-9 in oral cancer facilitates metastatic spread because of altered cancer cell-matrix interactions [10]. However, the level of galectin-9 in cancer cells does not seem to have direct prognostic significance [5]. Thus, due to the low-level or absent expression of galectin-9 on tumour cells, we aimed to investigate its expression on tumour- associated immune cells (TAICs) and to assess its potential prognostic value in OSCC.
Material and methods
Study group
A retrospective analysis was conducted in a group of 62 patients with OSCC treated in the Maxillofacial Surgery Department at the University Clinical Centre in Gdansk, Poland. The tissue naïve to chemotherapy and radiation therapy was collected during surgical resection or diagnostic biopsy. Basic clinicopathological data were retrieved from patients’ medical records (age, sex, grade, tumor-node-metastasis (TNM) stage, location, alcohol and tobacco abuse, treatment modalities). If necessary, TNM stages were reclassified according to the 8th edition of the American Joint Committee of Cancer Staging Manual. Overall survival (OS), defined as the time from the diagnosis to death from any cause, was established for all patients. The summary of basic clinicopathological characteristics of the study cohort is shown in Table 1.
Table 1
Summary of clinicopathological features of the study cohort
Immunohistochemistry
All hematoxylin and eosin stain microscopic slides were revised by 2 pathologists (RP and MK), and representative tumour areas were selected for further analyses. Subsequently, formalin-fixed, paraffin-embedded tissue blocks were used to construct tissue microarrays using a Manual Tissue Arrayer MTA 1 device (Beecher Instruments Inc., Sun Prairie, WI, USA). Then, all blocks were cut into sections of 4 µm thickness on a microtome (Leica SM 2000, Nussloch, Germany). Before staining, the slides were incubated for 24 hours at 37°C, deparaffinized, and rehydrated. For antigen retrieval, the heat-induced epitope retrieval method was used (PTLink, Dako, Glostrup, Denmark). For blocking, endogenous peroxidase slides were incubated in 3% H2O2 for 5 min. A manual staining procedure was conducted using the Dako EnVision Flex/HRP system (Glostrup, Denmark). Immunohistochemical staining was performed using rabbit monoclonal anti-galectin-9 antibody (D9R4A XP®, Cell Signalling Technology). Histologically normal tonsil was used for the positive control. Omission of the primary antibody was used as a negative control. Any lymphocytes or macrophages detected at the tumour-stroma interface were considered TAICs [11]. The assessment of the portion of positive TAICs was done manually by 2 pathologists (RP and MK). In discrepant cases, the final scores were reconciled following discussion. Cytoplasmatic reactions in the TAICs was counted as positive. For each core, the percentage of galactin-9-positive cells was established in relation to all TAICs in the core. The average score from both cores was used in the further analyses.
Statistics
Statistical analyses were performed with the use of Statistica 13 (RRID:SCR_014213, Tibco, Palo Alto, CA, USA) licensed to the Medical University of Gdansk, and R statistical environment [12]. Categorical variables were compared with χ2 or Fisher’s exact test if applicable. The distribution of continuous variables was analysed with the Mann-Whitney U test or the Kruskal-Wallis test. In the case of multiple comparisons, obtained p-values were controlled for a false discovery rate established at 0.05 with the Benjamini-Hochberg approach. The optimal cut-off value for galectin-9 expression in terms of survival analysis was identified with the use of the surv_cutpoint() function from the “survminer” package [13]. Kaplan- Meier curves were plotted using the “survminer” and “ggsci” packages [13, 14]. Hazard ratios were estimated using Cox regression analysis. A p-value < 0.05 was considered as significant. Boxplots were plotted using the “ggplot2” package [15].
Results
Expression of galectin-9 on tumour-associated immune cells and its association with clinicopathological characteristics
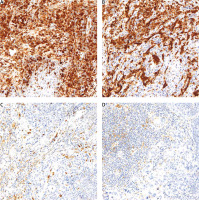
Expression of galectin-9 in at least 1% of TAICs was observed in all cases. The median percentage of galectin-9-expressing cells was 30% (range 5–90%, interquartile range 10–70%). The representative examples of immunohistochemical reactions are given in Figure 1.
Fig. 1
The representative examples of intense, diffuse staining (A, B) and weak reaction only in scattered tumour-associated immune cells of oral squamous cell carcinoma (C, D)
Note the negative reaction in cancer cells in all cases.
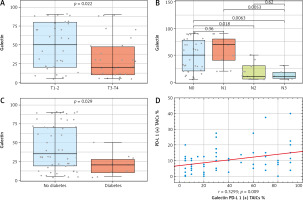
Expression of galectin-9 was not associated with sex (p = 0.192, Mann-Whitney U test), grade (p = 0.706, Mann-Whitney U test), smoking (p = 0.720, Mann-Whitney U test), or alcohol status (p = 0.829, Mann-Whitney U test). We observed higher expression of galectin-9 in less locally advanced tumours (lower T descriptor; p = 0.023, Mann-Whitney U test) (Fig. 2 A) without nodal metastases (p = 0.014, Mann-Whitney U test). Interestingly, there was no difference between N0 and N1 cancer, but N2 and N3 cases were associated with a significantly lower percentage of galectin-9-positive cells (Fig. 2 B). Conversely, significantly lower expression of the investigated marker was seen in patients with diabetes mellitus type 2 (p = 0.029, Mann-Whitney U test) (Fig. 2 C). There was a trend towards a higher expression of galectin-9 in cancers of the tongue and floor of the oral cavity when compared to other locations (p = 0.054, Mann-Whitney U test).
Due to the crucial role of galectin-9 as the immune regulator in TME, we also aimed to investigate its potential relationships with the expression of PD-L1 on TAICs and cancer cells. The PD-L1 expression was performed as described previously [16]. Interestingly, there was a positive correlation between high PD-L1 and galectin-9 expression on TAICs (r = 0.329, p = 0.009, Pearson) (Fig. 2 D). No association was noted with PD-L1 expression on tumour cells (r = 0.185, p = 0.15, Pearson).
Fig. 2
Boxplots presenting significant associations between clinicopathological parameters and the percentage of galectin-9-positive tumour-associated immune cells (TAICs) in oral squamous cell carcinoma. Patients with more locally advanced tumours (A), with N2 and N3 disease (B), and diabetes (C). PD-L1 expression on TAICs positively correlated with galectin-9 expression on immune cells as shown on scatterplot (D)
Presented p-values were calculated with Mann-Whitney U test, Kruskall-Wallis or Spearman test if applicable (in the case of multiple comparisons, the associations remained significant with Benjamini-Hochberg correction). Horizontal lines inside boxes show median values. The lower and upper hinges correspond to the first and third quartiles (the 25th and 75th percentiles). Upper and lower whiskers indicate 1.5 interquartile range of the lower and upper quartile, respectively. Circles represent individual measures.
Survival analysis
Follow-up of patients was censored at 5 years, and the cumulative 5-year OS was 40%. During the observation time 37 patients died (59.7%). All other patients (n = 25, 40.3%) were alive at the time of censoring.
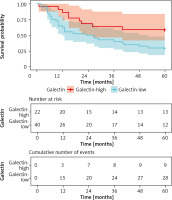
To explore the potential of galectin-9 as a prognostic factor in OSCC we divided our cohort into 2 groups depending on the percentage of galectin-9-positive cells. The cut-off of 50% of stained cells was established utilizing the “surv_cutpoint” function from the “survminer” package. Patients characterized by > 50% of galectin-9-positive cells were characterized by the favourable 5-year OS when compared to the galectin-9-low group (59% vs. 30%, p = 0.029, log-rank) (Fig. 3). This finding was confirmed in univariate Cox regression analysis (HR = 0.446, 95% CI: 0.201–0.946). Nevertheless, it was insignificant in the multivariable Cox regression model controlled by crucial clinicopathological factors (T descriptor, status of lymph nodes).
Fig. 3
Kaplan-Meier curves with confidence intervals plotted for cases with low and high expression of galectin-9 expression in tumourassociated immune cells in oral squamous cell carcinoma
Patients with high percentage (> 50%) of positive cells had better 5-year overall survival. P-value was calculated with log-rank test.
Discussion
Galectins are frequently described as the “double edged sword” in cancer due to their enhancing or inhibiting tumour activity depending on which ligand they interact with on various cells in TME [4]. Moreover, they may be expressed in tumour cells, but also in immune cells residing in TME. Importantly, galectin-9 is the only known soluble immune checkpoint molecule [16]. Galectins may serve as targets for immunotherapy, and current data suggest that its efficacy depends on expression profiles in each individual [8].
In the current study, we aimed to investigate the expression of galectin-9 in TAICs of OSCC. Our results demonstrate that high expression of galectin-9 in immune cells is associated with less locally advanced cancer, lack of nodal metastases, and higher 5-year OS. The majority of studies to-date have focused on the assessment of galectin-9 in tumour cells; however, various leukocytes may be its source, including activated T-lymphocytes, macrophages, dendritic cells, mast cells, and NK cells [17]. The soluble form of galectin-9 may work as an anti-tumour and anti- metastatic agent [18]. It may boost antitumor reactions, increasing the number of CD8/TIM-3-positive T lymphocytes and CD86/TIM-3-positive dendritic cells [19]. It can also interact with PD-L1 in immune cells. Hereby, we demonstrated that galectin-9 expression was positively correlated with PD-L1 expression on TAICs. In our previous study, we showed that high PD-L1 expression on immune cells in OSCC is associated with superior OS [19]. Similar relationships were previously reported in glioblastoma and small cell lung carcinoma [20, 21]. In the latter, co-expression of galectin-9 and PD-L1 was associated with longer relapse-free survival. Accordingly, in hepatocellular carcinoma, high circulating levels of PD-L1 and galectin-9 are associated with better survival [22]. Conversely, in non-small cell lung carcinoma, He et al. observed a negative impact of galectin-9 express on tumour-infiltrating lymphocytes on OS [23]. A recent study on a small cohort of head and neck squamous cell carcinomas showed that galectin-9 expression tends to be expressed in immune-inflamed tumours more than in immune-excluded or immune desert cases [24]. It is highly possible that the prognostic significance of this molecule depends on the tumour site, tissue context, other TME constituents, and immune characteristics of the host.
Surprisingly, we observed lower expression of galectin-9 in patients with diabetes. Generally, its serum levels tend to be elevated in diabetes [25, 26]. However, some studies showed contradictory results [27]. It is unclear if this association may have any impact on TME of OSCC or induce a mechanism of impact that affects survival in OSCC patients with diabetes. Nevertheless, future studies on galectin-9 levels in cancer should include diabetes as the potential confounder.
Our study has two important limitations. The cohort size was relatively small and the analysis was retrospective. Nevertheless, we performed long and full follow-up of the patients enrolled in the study.
Conclusions
Galectin-9 is commonly expressed on TAICs in OSCCs, but the portion of positive cells varies significantly. A high level of galectin-9 expression is related to the presence of favourable clinicopathological characteristics, i.e. lack of nodal metastases and less locally advanced tumours, and thus superior 5-year OS. Moreover, there was a positive correlation between the percentage of galectin-9-positive and PD-L1-positive TAICs. The latter may suggest the relationship between galectin-9 and the condition of the TME in OSCC. Future translational studies should focus on the molecular mechanisms of these associations and potential usefulness of galectin-targeted treatment in OSCC.







