A 63-year-old female patient who was suffering from hypertension visited a cardiologist because of fainting and palpitations. Auscultation revealed a continuous murmur over the entire precordium, the most intense in the second intercostal space, intensity IV/V. The electrocardiogram showed sinus rhythm, frequency 60/min, normogram, and incomplete right bundle branch block. On transthoracic echocardiography, a jet was registered on the parasternal long axis view of the aorta at the insertion site of the left aortic cusp, while on the subcostal view, a high flow velocity was registered at the site of the jet (Vmax 4 m/s). After that, transesophageal echocardiography (TEE) was suggested. On TEE in the projection of the left sinus of Valsalva, a fistula was observed, which was most likely in communication with the right atrium (RA). Coronary angiogram showed the fistula originating near the left coronary cusp and probably ending in the RA (Figure 1 A). A previous exercise stress test was negative. Computed tomography revealed that the fistula originated from the left main coronary artery (LMCA) and flowed into the RA (Figures 1 B, C). The heart team initially considered percutaneous closure of the fistula. However, due to the diameter of the fistula, which in its full extent came out of the LMCA, as well as the need for an additional stent in the same, it was decided to perform a surgical intervention.
Figure 1
A – Conventional angiography demonstrating filling of fistula with contrast agent. B – Computed tomography (CT): the fistula (blue arrow) originates from the left main coronary artery (green arrow). C – CT: the fistula flows into the right atrium (blue arrow). D – Surgical view of the fistula (Note: The image was taken during cardiopulmonary bypass, so the actual diameter of the fistula, which was 1.5–3 cm, is not visible.)
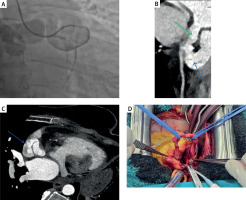
After transverse aortotomy, a dilated left coronary artery ostium was observed. An anomalous canal began from the LMCA, directed towards the RA, retro-aortic, with an opening into the RA in the region of the superior vena cava, with a tortuous course (Figure 1 D). The fistula was prepared along its entire length, tied, and cut. The total length of the fistula was 17 cm. The postoperative course was uneventful, and the patient was discharged from the hospital on the 6th postoperative day. At the check-up 2 months later, she stated that she did not have the problems she had before the surgery.
The existence of congenital anomalies of the heart and blood vessels, even when asymptomatic, can be extremely dangerous in situations of interventional procedures on the heart and blood vessels [1]. Coronary artery fistulas are rare and present in about 0.002% of the general population and represent 0.3% of congenital heart disease [2, 3].
Coronary-cameral fistulas (CCFs) are a rare form of coronary artery fistula in which an abnormal communication exists between the coronary artery and a cardiac chamber. CCFs commonly arise from the right coronary artery (50–60%) and the left anterior descending artery (25–42%) [2, 3]. The right ventricle is the most common site of inflow of these fistulas, in up to 40% [2, 3]. LMCA involvement accounts for just 0.7% of CCFs [2]. Of all types of coronary fistulas, those that connect the LMCA to the RA, as in our case, are uncommon, and very few surgically corrected cases have been reported previously [3].








