Patients with impaired left ventricle ejection fraction (LVEF) have a significant risk of sudden cardiac death after high-risk percutaneous coronary intervention (PCI) requiring short-term mechanical circulatory support (MCS) [1]. Therefore, prevention of complications that may be critical for patients’ prognosis is crucial [2].
A 72-year-old man with multimorbidity (hypertension, type II diabetes, dyslipidemia, peripheral artery disease, chronic kidney failure) and reduced LVEF to 30%, presenting with chronic coronary syndrome with class III symptoms according to the Canadian Cardiovascular Society scale, was admitted to undergo elective invasive diagnostics of coronary artery disease. Coronary angiography revealed multivessel coronary disease with significant calcified lesions in the right coronary artery (RCA) (Figure 1 B) and chronic total occlusions of both the left anterior descending (LAD) and circumflex artery with poor collateral flow. Due to low LVEF and lack of venous material for grafting as well as non-surgical mid and distal portion of the LAD, the patient was planned for high-risk PCI with MCS on the last remaining vessel. Computed tomography angiography was performed to assess the access site and iliac arteries and showed bilateral iliac tortuosity with moderate calcifications more present on the left, so the right common femoral artery (RCFA) was used as a large-bore access site. Under ultrasound guidance, the RCFA was punctured and mechanical sutures were deployed. 19F Impella peel-away short and long sheaths could not be delivered, so predilation with a peripheral 7.0 × 30 mm Armada balloon (Abbott, USA) was performed. However, still the sheath was unable to cross. We decided on the off-label use of the 14F iSleeve sheath (Boston Scientific, USA), which is our routine approach as bailout for access, and the sheath easily crossed the lesion and ported in the abdominal aorta, with subsequent Impella insertion (Figure 1 A) and delivery to the left ventricle, but with former balloon inflation within the sheath.
Figure 1
A – angiography of right external iliac artery, inserted Impella (arrow: folding of the sheath during insertion), B – coronarography of right coronary artery (RCA), before percutaneous coronary intervention (PCI), C – final result of PCI RCA, D – removing Impella (trouble with inserting cannula to iSleeve sheath) (arrow: peripheral balloon), E – longitudinal distortion visible on the sheath, after removal
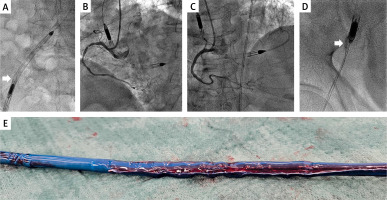
Imaging-guided PCI on the severely calcified RCA included lesion preparation with coronary lithotripsy using a 3.0 × 12 mm balloon, resulting in huge myocardial ischemia. Finally, two drug-eluting stents were implanted under intravascular ultrasound control. After completed revascularization (Figure 1 C), the Impella was removed from the left ventricle and typically pulled back down to the entry site. However, it was stuck within the iSleeve sheath and could not be retrieved. After increasing the tension on the whole system, the MCS device was able to reach the femoral artery but together with the folded sheath; thus, it could not be removed again. Using the right radial approach, from which PCI was performed, we crossed towards right iliac arteries with an 0.018′′ wire (Figure 1 D) and delivered a long shaft peripheral 4.0 × 40 balloon, which was inflated at the site of resistance. Then, after partial removal of the sheath, the Impella was successfully removed. A longitudinal distortion of the sheath was visible on fluoroscopy. The 0.035′′ wire could not cross the folded sheath, so we used a dilator with the wire; this successfully unfolded the sheath, which was then removed (Figure 1 E), and the artery was successfully closed with mechanical sutures and a collagen-based device. Follow-up angiography showed a minor dissection of the right external iliac artery, without impairment of the flow. The patient was discharged home after 3 days in a good overall condition.
Large-bore access-related complications are quite frequent [3, 4]. Here we presented one such case, with subsequent solution.








