Corrective cardiac surgery in infants with congenital common atrioventricular septal defect (CAVSD) remains a challenge in patients with suboptimal anatomy [1]. We present the hybrid primary implantation of an inverted MELODY valve into the left atrioventricular valve (LAVV) position as a corrective procedure in an infant with CAVSD and our current 4-year, event-free follow-up – another successful application of the MELODY valve in a pediatric patient, used for the first time in the primary correction of CAVSD [2, 3].
A 6-month-old boy presented with prenatally diagnosed CAVSD, chronic respiratory failure, a history of septic shock, prolonged respiratory support, and deletion of the 12q chromosome without neurological disorders. The child was initially treated with pulmonary artery (PA) banding at the age of 4 weeks. The patient was continuously managed in the intensive care unit (ICU) until the time of corrective surgery.
The child was admitted to the pediatric cardiac surgery unit in critical general condition, nasally intubated, with borderline decompensation, hepatomegaly and peripheral edema (Figure 1 A). Preoperative echocardiography confirmed CAVSD with moderate central regurgitation of the common atrioventricular (AV) valve and a single papillary muscle present in the left ventricle with atrophy of the left posterior leaflet. The patient was referred for high-risk correction of the CAVSD with primary hybrid inverted MELODY valve implantation in the LAVV position with PA debanding and balloon dilatation of the pulmonary stenosis (Figure 1).
Figure 1
A – Preoperative chest X-ray revealed cardiomegaly with pulmonary interstitial changes. B – MELODY valve pre-prepared on a side table, with a Gore-Tex collar and double-folded valve stent. C – Intraoperative view: Inverted MELODY valve implanted in the left neo-orifice using a Prolene 5-0 semi-continuous suture technique. Single-patch correction of a common atrioventricular septal defect. D – Intraoperative final balloon dilatation of MELODY valve to adjust the stent diameter to the new left ‘neo-AV’ orifice. E – Postoperative control echocardiography after CAVSD correction with the MELODY valve in the left atrioventricular position – after 4 years. Apical four-chamber view with color Doppler demonstrated laminar flow through the MELODY valve
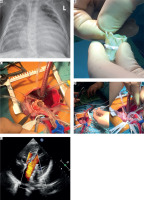
Intraoperatively an extensive CAVSD Rastelli type A [4] with a large inflow ventricular septal defect (VSD) and a primum atrial septum defect was identified. The common AV valve appeared fibrotic and dysmorphic – irreparable using the patient’s own tissues. The single patch technique was used. The VSD was closed with a Gore-Tex patch and a continuous suture technique. Afterward, a reversed MELODY valve was implanted into the created left ‘neo-orifice’ using Prolene 5-0 semi-continuous sutures (Figures 1 B, C). Prior to closure of the primum defect, hybrid balloon dilatation of the MELODY was performed using sequentially sized balloons of 8, 10, 12, 14, and 16 mm (Figure 1 D). Following balloon dilatation, no leaflet regurgitation or perivalvular leakage was found. Subsequently, the primum defect was closed with the same continuous Gore-Tex patch with an intentionally left interatrial communication (3.5 mm puncher facing the MELODY stent). The remaining tissues of the native AV valve were used to rebuild the right atrioventricular valve (RAVV). After PA debanding, a complementary hybrid intraoperative balloon dilatation of the PA trunk was performed.
The early postoperative period was supported with moderate catecholamines and prolonged mechanical ventilation due to interstitial lung lesions with planned extubation in the ICU. Two-drug antibiotic therapy was administered. Bronchial bloody effusions and signs of bleeding from the gastrointestinal tube and Foley catheter were temporarily observed. Postoperative echocardiography revealed an LAVV orifice with a competent MELODY valve (Figure 1 E), mild RAVV insufficiency, and preserved general heart contractility.
After gradual improvement, enteral nutrition was started, and antiplatelet therapy with oral acetylsalicylic acid was initiated. Follow-up echocardiograms consistently confirmed successful correction of CAVSD with no dysfunction of the MELODY valve in the LAVV position and preserved ventricular function. The child was discharged home and referred for outpatient follow-up, further multi-specialist care, and physiotherapy.
Currently, after 4 years, the child’s condition is fairly good, with predominant symptoms of the genetic disorder, without heart failure. The MELODY valve function in the LAVV, as well as left ventricle contractility, is excellent, further valve dilatation has not yet been needed, and the patient is currently on antiplatelet therapy only.
To our knowledge, this report presents the first application of the MELODY valve for primary anatomical correction of complex CAVSD. The main advantage of using the MELODY valve as an atrioventricular prosthesis is its ability to tailor the valve to the reconstructed atrioventricular annulus, maximizing the effective orifice area – an important consideration for potential future valve replacements. Despite its known limitations, in some anatomically unfavorable cases the MELODY valve may offer the most advantageous prosthetic solution among the available suboptimal options.






