Ibrutinib is an irreversible inhibitor of Bruton’s tyrosine kinase (BTK), a cytoplasmic tyrosine kinase of the Tec family, which plays an important role in the B-cell receptor signaling pathway [1]. Ibrutinib is used for the treatment of chronic lymphocytic leukemia, mantle cell lymphoma, Waldenström macroglobulinemia, and graft versus host disease [2]. Ibrutinib predisposes to bleeding by inhibiting BTK and Tec, which play a role in the inhibitory signaling pathway of platelet collagen receptors such as glycoprotein VI (GP VI) and C-type lectin-like receptor 2 (CLEC-2). In addition, ibrutinib has an inhibitory effect on the interaction of von Willebrand factor and glycoprotein-1b (GP 1b), and microvascular hemorrhages can be explained by this mechanism [3]. Cases of ibrutinib-related minor bleeding besides fatal hemorrhages such as subdural hematoma, gastrointestinal bleeding, and very rarely hemothorax, have been reported in the literature [2, 4]. Here, we aimed to present a case of ibrutinib-related alveolar hemorrhage and spontaneous hemothorax in a patient with pulmonary graft versus host disease due to allogeneic stem cell transplantation performed for acute lymphoblastic leukemia.
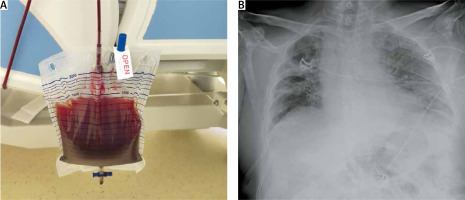
Written informed consent was obtained from the patient for the case report and each image used. A 56-year-old male patient presented with the complaint of hemoptysis that continued for 3 days. His medical history included allogeneic stem cell transplantation for precursor B-cell acute lymphocytic leukemia (ALL) 2 years ago and using ibrutinib treatment for treatment of pulmonary graft versus host disease for 8 days. He had neither antiaggregant nor anticoagulant use. His vital parameters were as follows: oxygen saturation was 93% with 2 l/minute nasal oxygen, heart rate was 92/minute, and arterial blood pressure was 137/76 mm Hg. There were decreased breath sounds at the right lung basal and bilateral fine crackles in respiratory system examination. Bluntness was detected at the right costophrenic sinus on chest X-ray (Figure 1 A). Bilateral alveolar hemorrhage and pleural effusion with high-density at the right side were detected on thorax computed tomography (Figure 1 B). The appearance of the fluid taken by thoracentesis from right hemithorax was hemorrhagic. Light criteria were as follows: lactate dehydrogenase (LDH): 621 U/l (serum LDH: 457 U/l), protein 4.39 g/dl (serum protein: 5 g/dl), albumin: 2.53 g/dl (serum albumin: 2.9 g/dl). Hematocrit of pleural fluid to serum hematocrit ratio was 0.93. A catheter thoracostomy with a 12-French chest catheter was performed for diagnosis of spontaneous hemothorax and 1100 ml of hemorrhagic drainage was observed for 24 hours (Figure 2 A). The patient was followed with the chest catheter for 7 days, drainage from the thoracic catheter decreased and it became serous in appearance, and the expansion of both lungs was observed on the chest X-ray (Figure 2 B). We decided to remove the chest catheter but the patient developed cardiac arrest of unknown cause. The patient died due to not responding to cardiopulmonary resuscitation.
Figure 1
A – Sinus bluntness is seen on the right chest X-ray. B – Thorax computed tomography shows alveolar hemorrhage and pleural effusion
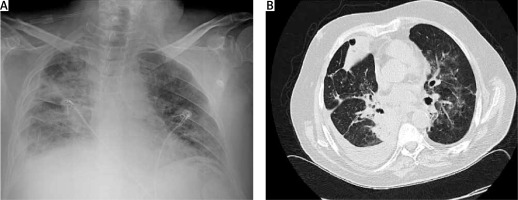
Figure 2
A – Appearance of pleural fluid drained by catheter thoracostomy. B – Chest X-ray shows lung expansion after the catheter thoracostomy treatment
Here, we present a case of alveolar hemorrhage and hemothorax that occurred as a rare complication of ibrutinib treatment. Publications including ibrutinib-related hemorrhage have emphasized platelet dysfunction for pathophysiology of bleeding in the literature [1, 5]. Lipsky et al. reported in their study including ibrutinib-associated mucocutaneous bleeding complications that patients not only had thrombocytopenia and platelet dysfunction, but also had a decrease in von Willebrand factor and factor VII activity. Furthermore it has been reported in another study that the risk of bleeding increases with the use of ibrutinib in combination with nonsteroidal anti-inflammatory drugs, aspirin or fish oil [2]. That combination was not present in our case. The majority of case reports including ibrutinib-related hemorrhage have reported minor bleeding such as subcutaneous hemorrhage or epistaxis, etc., whereas the risk of fatal hemorrhage has been reported as less than 1% [1]. Chanan-Khan et al. reported in their study that there was a significant increase of bleeding complications in the ibrutinib group compared to the placebo group; the rate of major bleeding was 4% and the rate of fatal bleeding was 0.7% [6]. An article published by Locke including ibrutinib-related alveolar hemorrhage reported that the patient used aspirin due to coronary artery disease and he died due to massive alveolar hemorrhage and asphyxia [7]. Similar aspects of our case were the initial presentation being hemoptysis and the detection of alveolar hemorrhage on tomography. But there was no use of aspirin and hemoptysis stopped at his follow-up. In addition, there were no signs of hemoptysis or asphyxia during the cardiac arrest period. Only 1 case report of ibrutinib-associated spontaneous hemothorax was found in the English literature. In this case report, spontaneous hemothorax occurred in a 71-year-old patient who received ibrutinib treatment for chronic lymphocytic leukemia and his hemothorax was treated by tube thoracostomy that continued 9 days. In our case, hemothorax treatment was completed in 7 days with catheter thoracostomy and we planned removal of the catheter, but the patient died due to cardiac arrest with an unknown cause.
As a result, it should be kept in mind that spontaneous hemothorax and diffuse alveolar hemorrhage may occur in patients with hemoptysis and pleural effusion who underwent ibrutinib therapy for whichever indications. Especially when aspirin and anticoagulants are used additionally, fatal bleeding may develop.






