Summary
This study examines the impact of bystander cardiopulmonary resuscitation (CPR) on out-of-hospital cardiac arrest (OHCA) survival in Saudi Arabia, using data from the Saudi Red Crescent Authority. Findings show that bystander CPR was performed in only 12.0% of cases, with higher return of spontaneous circulation (ROSC) rates among recipients (17.6% vs. 12.0%). However, after adjusting for confounders, bystander CPR was not independently linked to increased survival. Significant regional disparities were observed, with Riyadh showing the highest bystander CPR rate (26.4%), while several regions had rates below 5%. The study underscores the need for national CPR training programs, improved emergency response times, and targeted regional interventions to enhance OHCA survival outcomes.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a critical public health issue contributing to significant morbidity and mortality worldwide. Despite advancements in emergency medical services (EMS) and hospital-based resuscitation strategies, survival rates remain alarmingly low [1]. One of the most crucial factors influencing OHCA survival is the early initiation of bystander cardiopulmonary resuscitation (CPR), which can significantly enhance the likelihood of return of spontaneous circulation (ROSC) and overall survival rates [2]. However, despite its well-documented benefits, bystander CPR rates remain suboptimal in many regions, particularly in the Middle East, including Saudi Arabia, where cultural and logistical barriers often limit intervention.
Global studies have highlighted significant disparities in OHCA incidence, bystander CPR rates, and survival outcomes. In high-income countries, public awareness campaigns and mandatory CPR training have led to increased intervention rates. For example, Scandinavian countries report bystander CPR rates exceeding 70% due to mandatory CPR training in schools and workplaces [2]. Conversely, in many Middle Eastern and Asian countries, these rates remain below 20%, reflecting gaps in public education and access to AEDs [3].
In Saudi Arabia, studies indicate that bystander CPR rates are particularly low. Bin Salleeh et al. found that in a university hospital in central Saudi Arabia, delays in EMS response and a lack of bystander intervention significantly impacted OHCA survival rates [4]. Similarly, Almiro et al. examined OHCA cases in Riyadh and identified substantial demographic and clinical variations, highlighting the need for region-specific interventions [5]. Furthermore, Alabdali et al. presented findings from the Saudi Out-of-Hospital Cardiac Arrest Registry, emphasizing the necessity for improved public awareness and emergency response strategies [6].
While research from Oman and the broader Gulf region aligns with these findings, underscoring the importance of rapid EMS response and early CPR intervention, there is still a lack of comprehensive, nationwide data assessing the impact of bystander CPR on OHCA survival across different regions of Saudi Arabia [7]. Given the variations in healthcare infrastructure and emergency response capabilities across the Kingdom’s 13 regions, it is crucial to examine the regional differences in bystander CPR implementation and its effect on OHCA outcomes.
Aim
This study aims to bridge the knowledge gap by evaluating the impact of bystander CPR on OHCA survival rates across the 13 regions of Saudi Arabia. Specifically, it seeks to determine the proportion of OHCA cases that received bystander CPR in each region. Understanding these rates is essential to assessing the current state of public awareness and preparedness in responding to cardiac arrest emergencies.
Additionally, this study aims to assess ROSC rates for OHCA cases with and without bystander CPR intervention. Identifying differences in survival rates between these groups can provide critical insights into the effectiveness of early intervention. Another objective is to analyze the association between bystander CPR and OHCA survival rates while accounting for relevant factors such as patient demographics, arrest characteristics, and EMS response times. A comprehensive analysis of these variables will help determine whether bystander CPR independently contributes to improved survival outcomes.
Finally, this study seeks to identify regional variations in the impact of bystander CPR on OHCA survival rates. Investigating these disparities can inform targeted public health strategies and policy recommendations to enhance emergency response systems across Saudi Arabia.
This study provides evidence-based insights to inform future public health interventions and emergency response policies in Saudi Arabia, ultimately improving OHCA survival outcomes in the Kingdom.
Material and methods
Study design
This study employs a retrospective observational design to analyze the impact of bystander CPR on OHCA survival rates. The study covers a 6-month period, from January 1, 2024, to June 30, 2024. A retrospective approach allows for the assessment of real-world OHCA outcomes based on existing EMS records, minimizing bias while ensuring comprehensive data analysis.
Data source
The data for this study were obtained from the Saudi Red Crescent Authority (SRCA), the national emergency medical services (EMS) provider in Saudi Arabia. The dataset includes all OHCA cases transported by SRCA during the study period. The SRCA database is a reliable and comprehensive source of prehospital emergency data, allowing for an in-depth analysis of cardiac arrest cases and resuscitation efforts.
The SRCA operates as the sole national provider of emergency medical services in Saudi Arabia. The system is structured with a mix of Basic Life Support (BLS) and Advanced Life Support (ALS) ambulance teams, with ALS coverage being more prominent in urban regions. EMS personnel are trained to initiate defibrillation and provide advanced airway management and circulatory support when indicated. Most ambulances are equipped with manual defibrillators, and all EMS teams follow standardized prehospital resuscitation protocols based on international guidelines. However, the availability and use of public-access AEDs by bystanders remains limited, particularly in rural and underserved areas. This operational structure explains the high rate of recorded defibrillation in prehospital cases managed by EMS.
Study population
The study population consists of all OHCA cases transported by the SRCA across the 13 regions of Saudi Arabia during the study period. To ensure the accuracy and consistency of the analysis, cases that did not receive CPR, such as those pronounced dead upon EMS arrival, were excluded from the study. Cases were included irrespective of patient age, sex, nationality, or initial cardiac rhythm.
This broad inclusion criterion ensures a comprehensive understanding of OHCA outcomes in the Saudi Arabian context and facilitates a more detailed investigation of regional variations in bystander CPR effectiveness.
Data collection and variables
Data for this study were extracted from the SRCA database, which records extensive information on OHCA cases. The dataset included demographic details such as age, sex, and nationality. Cardiac arrest characteristics were also documented, including the location of the event (public, private, or residential), whether the arrest was witnessed, and the initial cardiac rhythm. Intervention variables focused on whether bystander CPR was administered, the EMS response time, the use of an AED, the number of shocks delivered, airway management procedures, and the use of mechanical CPR devices.
Outcome variables included the ROSC, survival to hospital admission, and regional differences in OHCA survival rates. To ensure data reliability, rigorous data validation techniques were employed, including error-checking for inconsistencies, removal of duplicate cases, and cross-verification with EMS records.
It is important to note that the dataset does not include region-specific population denominators, and therefore the reported figures reflect absolute case counts rather than incidence rates. As such, comparisons across regions are based on raw OHCA volumes and not adjusted for population size. Additionally, regions with high levels of domestic and international tourism, such as Makkah and Madinah, may have received a higher proportion of non-resident individuals, including pilgrims and visitors from countries with greater CPR awareness. While this may influence observed bystander CPR rates in certain regions, the data remain representative of the real-world operational burden faced by EMS teams and offer valuable insights for planning public health interventions and resource allocation.
Intervention variables included whether defibrillation was provided during the prehospital phase of care. The variable “Defibrillation provided (by EMS or AED, any source)” encompasses any instance of shock delivery using either manual defibrillators by EMS or AEDs regardless of whether the provider was a healthcare professional or a bystander. However, the dataset does not contain information that distinguishes who initiated the defibrillation. Therefore, it was not possible to separate AED use by bystanders from EMS-administered defibrillation. This is an important limitation, and future datasets should aim to capture this distinction for a more granular analysis of community-level resuscitation efforts.
Statistical analysis
Descriptive statistics were used to summarize patient demographics, clinical variables, and intervention details. Due to the observational nature of the dataset and the absence of distribution testing in the original EMS database export, continuous variables were reported as means and standard deviations (mean ± SD) for consistency with prior studies. However, given the expected skewness of time-based variables such as EMS response time, CPR initiation time, and on-scene resuscitation duration, we acknowledge that medians and interquartile ranges (Q1, Q3) would provide a more accurate representation. This limitation is discussed in the manuscript.
Additionally, geographical comparisons were made to evaluate regional variations in bystander CPR rates and their impact on survival outcomes. Statistical significance was set at a p-value of less than 0.05 to ensure robust conclusions. All analyses were performed using IBM SPSS Statistics for Windows, version 29.0 (IBM Corp., Armonk, NY, USA).
Results
Demographic and general information in the study
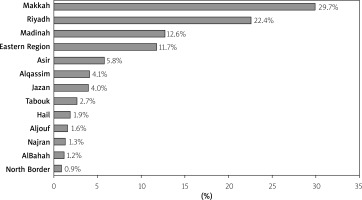
Table I shows the demographic and basic information of the patients in the study. The highest frequency of OHCA was recorded in Makkah (29.7%), followed by Riyadh (22.4%) and Madinah (12.6%), highlighting these areas as critical zones for targeted CPR training programs. Gender distribution showed a higher prevalence of males (65.2%) compared to females (34.7%), indicating potential gender-based disparities in OHCA incidents. Nationality analysis revealed that 53.6% of patients were Saudi nationals, 40.5% were non-Saudi, and 4.2% were not identified. The mean age of patients was 59.31 ± 22.0 years, underscoring the necessity for age-appropriate CPR interventions.
Table I
Demographic characteristics of OHCA patients across the 13 regions of Saudi Arabia
Moreover, Figure 1 illustrates the distribution of the OHCA across the different regions in the study.
Medical and clinical findings of the patients in the study
Table II shows the clinical findings of the patients in the study. It indicates that the majority of patients (87.4%) did not achieve a ROSC, with only 12.6% surviving. A significant portion of patients (77.8%) did not receive shocks, which might indicate non-shockable rhythms. Bystander CPR was provided to 12.0% of patients, highlighting the crucial role of public training initiatives. Witnessed arrests were noted in 29.6% of cases, emphasizing the importance of prompt intervention.
Table II
Clinical interventions and outcomes in OHCA
Advanced airway management techniques were utilized variably, with the majority (89.4%) receiving a combination of oropharyngeal airway (OPA) and bag-valve-mask (BVM). Intravenous (IV) access was established in 81.9% of cases, demonstrating adherence to resuscitation protocols. BLS alone was administered to 48.2% of patients, with a significant portion receiving a combination of ALS and BLS. The predominant cause of arrest was medical (87.8%), and mechanical CPR devices were used in 22% of cases. The mean response time was 12.13 min, and the average duration of on-scene CPR was 10.68 min, indicating efficient emergency response efforts. These findings underscore the need for continuous improvement in prehospital care and public awareness to enhance survival rates.
Factors influencing ROSC outcomes in the patients of the study
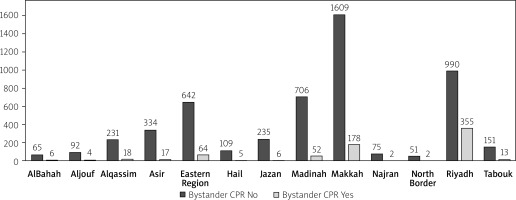
The distribution of bystander CPR across various regions in Saudi Arabia demonstrates significant variability (Table III and Figure 2). The results show significant disparities across all regions, p < 0.01. Riyadh stands out with the highest rate of bystander CPR, where 26.4% of cases received assistance before professional medical help arrived. This is notably higher compared to other regions, such as Makkah (10.0%) and the Eastern Region (9.1%), which also show relatively better rates of bystander CPR but still fall short of Riyadh.
Table III
Regional distribution of bystander CPR rates among OHCA patients
| Variables | Bystander CPR | P-value | |
|---|---|---|---|
| No | Yes | ||
| Al Bahah | 65 (91.5%) | 6 (8.5%) | < 0.001** |
| Aljouf | 92 (95.8%) | 4 (4.2%) | < 0.001** |
| Al Qassim | 231 (92.8%) | 18 (7.2%) | < 0.001** |
| Asir | 334 (95.2%) | 17 (4.8%) | < 0.001** |
| Eastern Region | 642 (90.9%) | 64 (9.1%) | < 0.001** |
| Hail | 109 (96.5%) | 5 (4.4%) | < 0.001** |
| Jazan | 235 (97.5%) | 6 (2.5%) | < 0.001** |
| Madinah | 706 (93.1%) | 52 (6.9%) | < 0.001** |
| Makkah | 1609 (90.0%) | 178 (10.0%) | < 0.001** |
| Najran | 75 (97.4%) | 2 (2.6%) | < 0.001** |
| North Border | 51 (96.2%) | 2 (3.8%) | < 0.001** |
| Riyadh | 990 (73.6%) | 355 (26.4%) | < 0.001** |
| Tabouk | 151 (92.1%) | 13 (7.9%) | 0.003** |
On the other end of the spectrum, regions like Jazan, Najran, Aljouf, and Hail demonstrate particularly low rates, with only 2.5%, 2.6%, 4.2%, and 4.4% of cases, respectively, receiving Bystander CPR. The regions of Al Qassim, Al Bahah, Asir, Madinah, North Border, and Tabouk also exhibit low rates, ranging from 4.8% to 8.5%.
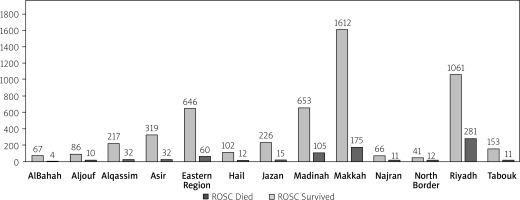
In addition, the analysis of ROSC outcomes across different regions in Saudi Arabia reveals significant geographic disparities (Table IV and Figure 3). The results revealed significant disparities across different regions in Saudi Arabia (p < 0.01). Notably, the North Border and Riyadh regions demonstrated higher survival rates, with 22.6% and 20.9% of patients achieving ROSC, respectively. These regions are followed by Najran (14.3%), Madinah (13.9%), and Al Qassim (12.9%), where survival rates are also relatively higher.
Table IV
Regional variations in ROSC outcomes among OHCA patients
| Regions | ROSC | P-value | |
|---|---|---|---|
| Died | Survived | ||
| Al Bahah | 67 (94.4%) | 4 (5.6%) | < 0.001** |
| Aljouf | 86 (89.6%) | 10 (10.4%) | < 0.001** |
| Al Qassim | 217 (87.1%) | 32 (12.9%) | < 0.001** |
| Asir | 319 (90.9%) | 32 (9.1%) | < 0.001** |
| Eastern Region | 646 (91.5%) | 60 (8.5%) | < 0.001** |
| Hail | 102 (89.5%) | 12 (10.5%) | < 0.001** |
| Jazan | 226 (93.8%) | 15 (6.2%) | < 0.001** |
| Madinah | 653 (86.1%) | 105 (13.9%) | < 0.001** |
| Makkah | 1612 (90.2%) | 175 (9.8%) | < 0.001** |
| Najran | 66 (85.7%) | 11 (14.3%) | < 0.001** |
| North Border | 41 (77.4%) | 12 (22.6%) | < 0.001** |
| Riyadh | 1064 (79.1%) | 281 (20.9%) | < 0.001** |
| Tabouk | 153 (93.3%) | 11 (6.7%) | < 0.001** |
In contrast, the regions of Al Bahah, Jazan, and Tabouk exhibit the lowest survival rates, with only 5.6%, 6.2%, and 6.7% of patients, respectively, achieving ROSC. The Eastern Region, Asir, and Makkah also show lower survival rates, with 8.5%, 9.1%, and 9.8%, respectively, despite their substantial population sizes. Hail and Aljouf have intermediate outcomes, with survival rates of 10.5% and 10.4%, respectively.
Moreover, Table V highlights several significant factors associated with ROSC outcomes in OHCA patients. The use of AED/defibrillators showed no significant difference in survival (p = 0.544), with similar ROSC rates between those who received defibrillation and those who did not. However, bystander CPR markedly improved survival rates (p < 0.001), with 17.6% of those receiving bystander CPR surviving compared to 12.0% who did not. Similarly, witnessed arrests significantly increased the likelihood of survival (p < 0.001), with 19.6% of witnessed cases achieving ROSC versus 9.7% of unwitnessed cases.
Table V
Association between clinical variables and ROSC in OHCA patients
| Variables | ROSC | P-value | ||
|---|---|---|---|---|
| Died | Survived | |||
| AED/Defibrillatora | No | 75 (85.2%) | 13 (14.8%) | 0.544 |
| Yes | 5177 (87.4%) | 747 (12.6%) | ||
| Bystander CPRa | No | 4657 (88.0%) | 633 (12.0%) | < 0.001** |
| Yes | 595 (82.4%) | 127 (17.6%) | ||
| Witnesseda | No | 3822 (90.3%) | 411 (9.7%) | < 0.001** |
| Yes | 1430 (80.4%) | 349 (19.6%) | ||
| Underlying cause of arresta | Medical | 4607 (87.3%) | 669 (12.7%) | 0.829 |
| Trauma | 643 (87.6%) | 91 (12.4%) | ||
| Mechanical CPR device usea | No | 4165 (88.8%) | 523 (11.2%) | < 0.001** |
| Yes | 1087 (82.1%) | 237 (17.9%) | ||
| Time of starting CPRb | Min.–max. | 0.030–0.926 | 0.003–0.888 | 0.318 |
| Mean ± SD | 0.671 ±2.48 | 0.660 ±1.51 | ||
| Time of arrest if (post-arrival)b | Min.–max. | 0.014–25.0 | 0.003–0.888 | 0.003** |
| Mean ± SD | 2.70 ±8.10 | 1.03 ±2.44 | ||
| Response time [min] from Incident time to Reach timeb | Min.–max. | 5.0–78.0 | 3.0–76 | < 0.001** |
| Mean ± SD | 12.45 ±8.73 | 11.10 ±7.49 | ||
| Duration of on-scene CPR [min]b | Min.–max. | 0.0–30.0 | 0.0–40.0 | 0.834 |
| Mean ± SD | 10.99 ±7.43 | 10.78 ±7.36 | ||
The underlying cause of arrest (medical vs. trauma) did not show a significant impact on survival (p = 0.829). The use of mechanical CPR devices was associated with improved outcomes (p < 0.001), with a higher survival rate of 17.9% compared to 11.2% for manual CPR. The time of arrest post-arrival, response time, and duration of on-scene CPR were also significant, with faster response times and shorter post-arrival arrest times linked to better survival rates (p < 0.01). Overall, these findings underscore the critical importance of rapid response and the utilization of mechanical CPR devices in improving survival rates for OHCA patients.
Finally, the logistic regression analysis identifies several key predictors for the ROSC in OHCA cases. Bystander CPR initially appeared significant with a crude odds ratio (OR) of 1.570 (95% CI: 1.274–1.935, p < 0.001); however, it was not statistically significant in the adjusted model (adjusted OR = 1.005, 95% CI: 0.802–1.260, p = 0.965). Witnessed arrests remained a robust predictor for ROSC, with a crude OR of 2.270 (95% CI: 1.944–2.650, p < 0.001) and an adjusted OR of 2.145 (95% CI: 1.816–2.534, p < 0.001), indicating more than twice the likelihood of ROSC if the arrest was witnessed.
The use of mechanical CPR devices also showed a significant positive association with ROSC, having a crude OR of 1.736 (95% CI: 1.469–2.053, p < 0.001) and an adjusted OR of 1.433 (95% CI: 1.202–1.709, p < 0.001). Response time was another significant factor; a shorter response time increased the odds of ROSC, with a crude OR of 0.981 (95% CI: 0.971–0.991, p < 0.001) and an adjusted OR of 0.981 (95% CI: 0.970–0.991, p < 0.001). The time of arrest post-arrival was not significant (p = 0.219) and was excluded from the adjusted model. These findings underscore the critical importance of witnessed arrests, mechanical CPR devices, and rapid response times in improving survival outcomes in OHCA cases (Table VI).
Table VI
Logistic regression analysis of predictors for ROSC in OHCA cases
| Predictors | Crude odds ratio | 95% CI for OR | P-value | Adjusted odds ratio | 95% CI for OR | P-value | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | |||||
| Bystander CPR | 1.570 | 1.274 | 1.935 | < 0.001** | 1.005 | 0.802 | 1.260 | 0.965 |
| Witnessed | 2.270 | 1.944 | 2.650 | < 0.001** | 2.145 | 1.816 | 2.534 | 0.000** |
| Mechanical CPR device use | 1.736 | 1.469 | 2.053 | < 0.001** | 1.433 | 1.202 | 1.709 | < 0.001** |
| Time of arrest if (post-arrival) | 0.956 | 0.890 | 1.027 | 0.219 | NA | |||
| Response time [min] | 0.981 | 0.971 | 0.991 | < 0.001** | 0.981 | 0.970 | 0.991 | < 0.001** |
Crude odds ratios measure the association between the two variables without controlling for other variables, detected by simple logistic regression. Adjusted odds ratios measure the association between the two variables while controlling for other variables in the model, detected by multiple logistic regression.
Lastly, Table VII shows the association between bystander CPR and ROSC across various regions in Saudi Arabia. The results indicate that most regions do not exhibit statistically significant associations between bystander CPR and ROSC outcomes (p > 0.05); however, some trends are worth mentioning. For instance, in Riyadh, a higher proportion of survivors was observed among those who received bystander CPR (24.2%) compared to those who did not (19.7%), with a p of 0.072, suggesting a potential, albeit non-significant, positive effect of bystander CPR in this region.
Table VII
Regional associations between bystander CPR and ROSC outcomes in OHCA patients
| Regions | Bystander CPR | ROSC | P-value | |
|---|---|---|---|---|
| Died | Survived | |||
| Al Bahaha | No | 62 (95.4%) | 3 (4.6%) | 0.303 |
| Yes | 5 (83.3%) | 1 (16.7%) | ||
| Aljoufa | No | 82 (89.1%) | 10 (10.9%) | 0.639 |
| Yes | 4 (100.0%) | 0 (0.0%) | ||
| Al Qassima | No | 200 (86.6%) | 31 (13.4%) | 0.297 |
| Yes | 17 (94.4%) | 1 (5.6%) | ||
| Asira | No | 302 (90.4%) | 32 (9.6%) | 0.189 |
| Yes | 17 (100.0%) | 0 (0.0%) | ||
| Eastern Regionb | No | 590 (91.9%) | 52 (8.1%) | 0.229 |
| Yes | 56 (87.5%) | 8 (12.5%) | ||
| Haila | No | 97 (89.0%) | 12 (11.0%) | 0.567 |
| Yes | 5 (100.0%) | 0 (0.0%) | ||
| Jazana | No | 220 (93.6%) | 15 (6.4%) | 0.677 |
| Yes | 6 (100.0%) | 0 (0.0%) | ||
| Madinahb | No | 606 (85.8%) | 100 (14.2%) | 0.359 |
| Yes | 47 (90.4%) | 5 (9.6%) | ||
| Makkahb | No | 1457 (90.6%) | 152 (9.4%) | 0.139 |
| Yes | 155 (87.1%) | 23 (12.9%) | ||
| Najrana | No | 65 (86.7%) | 10 (13.3%) | 0.267 |
| Yes | 1 (50.0%) | 1 (50.0%) | ||
| North Bordera | No | 39 (76.5%) | 12 (23.5%) | 0.595 |
| Yes | 2 (100.0%) | 0 (0.0%) | ||
| Riyadhb | No | 795 (80.3%) | 195 (19.7%) | 0.072 |
| Yes | 269 (75.8%) | 86 (24.2%) | ||
| Tabouka | No | 142 (94.0%) | 9 (6.0%) | 0.212 |
| Yes | 11 (84.6%) | 2 (15.4%) | ||
Conversely, in regions such as Aljouf, Asir, Hail, and Jazan, no survivors were recorded among patients who received bystander CPR, though the number of cases was relatively small. This lack of significant association is also observed in regions like Al Bahah, Al Qassim, and Madinah, where the difference in ROSC outcomes between those who did and did not receive bystander CPR was minimal. In Makkah and the Eastern Region, a slightly higher percentage of survivors was noted among those who received bystander CPR (12.9% and 12.5%, respectively); however, these differences were not statistically significant.
Discussion
The relatively low rate of bystander CPR in Saudi Arabia remains a significant public health concern. In contrast, countries with established CPR training policies, such as Sweden and Denmark, have reported bystander CPR rates exceeding 70%, which have contributed to markedly higher survival rates. Evidence from these settings highlights the importance of mandatory CPR education in schools, community-wide awareness campaigns, and increased accessibility to AEDs in public spaces. A study by Hansen et al. demonstrated that bystander intervention combined with early defibrillation substantially improves OHCA survival, a finding that aligns with international resuscitation guidelines recommending immediate CPR initiation [8]. The discrepancy between Saudi Arabia and high-performing countries suggests an urgent need for national CPR education initiatives to increase public confidence and willingness to perform CPR.
Interestingly, our study revealed significant regional variations in bystander CPR provision and OHCA survival rates across Saudi Arabia. Riyadh exhibited the highest rate of bystander CPR at 26.4%, while regions such as Jazan, Najran, and Aljouf recorded significantly lower rates, below 5%. These disparities could be attributed to differences in urbanization, public awareness, and EMS response times. Urban areas like Riyadh, where emergency medical services are more efficient and public CPR training programs are more accessible, may naturally demonstrate higher bystander intervention rates [9, 10]. In contrast, more rural or underserved regions may lack the infrastructure necessary for timely emergency response, which could explain lower rates of CPR administration and survival outcomes [11]. Studies from the United States have shown similar geographic disparities in OHCA survival, with urban areas consistently reporting higher bystander CPR rates than rural locations, largely due to differences in EMS accessibility and community engagement in CPR training [12, 13].
The findings of this study also highlight the potential impact of response times on OHCA survival. The mean EMS response time in our study was 12.13 min, which is notably longer than response times reported in countries with well-integrated prehospital care systems, such as Japan, where response times average around 8 min [13, 14]. Shorter response times are consistently associated with better survival outcomes, as the likelihood of ROSC decreases significantly with each passing minute without CPR. Our results reinforce the importance of enhancing prehospital emergency response systems in Saudi Arabia, including optimizing ambulance dispatch efficiency, expanding the presence of first responders, and increasing the availability of AEDs in public locations [15].
While bystander CPR was associated with improved ROSC rates, its impact on overall OHCA survival was not statistically significant after adjustment for confounders such as witnessed status, mechanical CPR device use, and response time. This finding warrants further investigation as international studies have consistently shown that bystander CPR can more than double the chances of survival. One possible explanation is that the quality of bystander CPR in Saudi Arabia may be suboptimal as previous research suggests that effective chest compressions and minimal interruptions are critical determinants of survival [16, 17]. Future studies should focus on assessing the quality and effectiveness of CPR delivered by bystanders, including compression depth, rate, and proper ventilation techniques.
Another critical factor influencing survival in our study was whether the OHCA event was witnessed. Witnessed arrests were significantly associated with higher ROSC rates (p < 0.001), with 19.6% of witnessed cases achieving ROSC compared to 9.7% of unwitnessed cases. This finding aligns with prior research demonstrating that OHCA cases witnessed by bystanders or EMS personnel have substantially better survival outcomes due to earlier intervention [18, 19]. This emphasizes the importance of increasing public awareness of cardiac arrest recognition and promoting immediate action in emergency situations. Additionally, mechanical CPR devices were associated with improved survival outcomes in our study, reinforcing their role in sustaining high-quality chest compressions, particularly in prolonged resuscitation efforts.
The results of this study have significant implications for public health policy and emergency response planning in Saudi Arabia. Increasing bystander CPR rates requires a multi-faceted approach that includes national-level CPR training programs, targeted education campaigns, and community engagement initiatives [20]. Implementing mandatory CPR training in high schools and workplaces, as successfully executed in countries like Denmark, Norway and the United Kingdom, could lead to substantial improvements in bystander intervention rates [21–23]. Additionally, improving EMS response times through optimized ambulance deployment strategies and increasing the availability of AEDs in public spaces could further enhance survival outcomes. The findings also highlight the need for region-specific strategies to address disparities in bystander CPR rates and OHCA survival, ensuring that underserved areas receive targeted interventions to improve emergency response effectiveness.
A comprehensive public health approach is essential to improving OHCA survival rates, as the effectiveness of bystander CPR extends beyond individual action to systemic preparedness and accessibility [24]. Strengthening emergency response systems requires not only widespread CPR training but also strategic placement of AEDs in high-risk locations, enhanced coordination between community responders and EMS, and targeted public awareness campaigns to foster a culture of immediate action during cardiac emergencies. Countries with high bystander CPR rates have successfully integrated CPR education into school curricula, workplace training, and national policies, demonstrating that early intervention can significantly reduce mortality [25, 26]. In Saudi Arabia, implementing a nationwide resuscitation initiative, supported by governmental and healthcare institutions, could bridge existing gaps and improve equitable access to life-saving measures [27, 28]. Investing in these long-term strategies will not only enhance OHCA survival but also contribute to a more resilient and health-conscious society.
Further research is needed to explore the reasons behind the observed regional disparities in OHCA outcomes, as well as to evaluate the long-term survival and neurological recovery of OHCA patients who receive bystander CPR. A prospective study design incorporating real-time data collection on CPR quality, response times, and AED use could provide a more comprehensive understanding of the factors influencing OHCA survival in Saudi Arabia. Future investigations should also assess the psychological and behavioral barriers that prevent bystanders from performing CPR, identifying strategies to increase public willingness to intervene in cardiac arrest situations.
This study provides valuable insights into the impact of bystander CPR on OHCA survival rates in Saudi Arabia. While bystander CPR improves ROSC rates, its overall impact on survival after adjusting for confounders was not significant, underscoring the need for further research into CPR quality and other determinants of OHCA outcomes. Regional variations in bystander CPR rates highlight the importance of targeted public health interventions to improve community response to cardiac arrest across all regions of the country. Enhancing CPR training programs, reducing EMS response times, and increasing AED accessibility are critical steps toward improving OHCA survival rates and reducing the burden of cardiac arrests in Saudi Arabia.
From a public health perspective, this study offers critical insights that go beyond individual patient outcomes. The regional disparities in bystander CPR provision and ROSC outcomes highlight systemic inequalities in health education, emergency preparedness, and access to prehospital care across Saudi Arabia. These findings underscore the urgent need for targeted health policies and region-specific interventions to improve OHCA survival.
Importantly, the data presented here can inform local and national public health strategies aimed at increasing bystander CPR rates, optimizing EMS response systems, and promoting equitable access to emergency resources. While this study may not offer granular clinical outcome data, its strength lies in capturing patterns of care and community response that are highly relevant to public health planning.
Given these dimensions, the study contributes meaningfully to the field of public health in Saudi Arabia and can support evidence-based decision-making for regional training programs, awareness campaigns, and system-level improvements in OHCA response.
While this study provides valuable insights into the impact of bystander CPR on OHCA survival rates in Saudi Arabia, several limitations should be acknowledged. The retrospective nature of this study means it relies on pre-existing EMS data, which may be subject to reporting inconsistencies and incomplete records. Some critical variables, such as the quality of bystander CPR, the exact timing of CPR initiation, and the presence of AEDs, are not fully documented, limiting the ability to assess their influence on survival outcomes.
Additionally, the study uses ROSC as the primary outcome, which, while important, represents only an initial resuscitation success and does not fully reflect longer-term clinical outcomes. Critical endpoints such as survival to hospital discharge, neurologic status, and post-discharge quality of life were not available in the dataset. These factors are essential to determine whether early bystander intervention translates into meaningful, sustained survival with good functional recovery.
The lack of these outcome measures limits the clinical interpretation of our findings. Although ROSC is a standard and necessary marker in prehospital studies, future research should incorporate hospital discharge data and validated neurological outcome scales such as the Cerebral Performance Category (CPC). This would allow for a more comprehensive evaluation of the true impact of bystander CPR on patient-centered outcomes.
Another important limitation is the absence of data regarding the quality of CPR administered by bystanders. While the dataset includes whether CPR was performed, it does not capture critical parameters such as compression depth, rate, or the presence of interruptions, which are essential for determining the true effectiveness of bystander resuscitation. Performing CPR does not necessarily imply effective resuscitation, and this limitation restricts the ability to draw strong conclusions about its clinical benefit.
Similarly, precise information on the timing of CPR initiation was not available. Although the dataset records EMS response times and arrest timing relative to EMS arrival, it lacks accurate time stamps for when bystander CPR began. Given that early initiation is a fundamental determinant of cardiac arrest survival, this data gap limits the study’s ability to assess the timeliness and potential impact of bystander actions.
Future research should incorporate real-time data capture technologies and include quality assessments of CPR performance. Integrating wearable or automated feedback devices and EMS-integrated digital logs could significantly enhance the granularity of data and allow for more accurate evaluation of intervention effectiveness.
The study also identifies regional variations in bystander CPR effectiveness, but the underlying reasons for these differences, such as public CPR training programs, emergency response efficiency, and cultural attitudes towards resuscitation, require further exploration. Another limitation is the potential for observer bias as EMS personnel rely on bystander reports to classify whether CPR was performed, which may lead to misclassification or inaccuracies in the dataset. Additionally, findings from Saudi Arabia may not be generalizable to other countries due to differences in emergency medical services infrastructure, healthcare policies, and public awareness regarding CPR.
Given these limitations, future research should adopt a prospective approach with real-time data collection, incorporate quality assessments of bystander CPR, and evaluate long-term patient outcomes to provide a more comprehensive understanding of the effectiveness of early resuscitation efforts.
Lastly, although the study is limited in its ability to assess long-term clinical outcomes or CPR quality, its strengths lie in population-level observations. From a public health standpoint, the identification of regional gaps in CPR provision offers actionable insights for system-wide improvements. The current dataset, while lacking clinical granularity, is sufficient to inform large-scale health interventions and prioritize regions for investment in training and infrastructure.
Furthermore, we acknowledge that the analysis was based on raw case counts without adjusting for regional population sizes. As such, the presented figures represent case volume rather than incidence rates. This was due to the unavailability of consistent and region-specific population data for the study period. Additionally, some high-tourism regions, such as Makkah or Madinah, may have included a larger proportion of non-residents, including pilgrims or visitors from countries with higher CPR awareness. While this may have influenced the likelihood of bystander CPR in certain areas, it does not compromise the internal validity of the dataset. These observed differences still hold public health relevance as they reflect the realities of EMS system strain and the potential benefits of targeted CPR training initiatives based on regional needs and demographics.
Conclusions
This study underscores the critical role of bystander CPR in improving OHCA survival outcomes in Saudi Arabia while revealing significant regional disparities in intervention rates. Although bystander CPR was associated with improved ROSC rates, its effect on overall survival after adjustment for confounders was not significant, highlighting the need for further research into CPR quality and other determinants of OHCA survival. The findings emphasize the urgency of strengthening CPR education, optimizing EMS response times, and expanding the availability of AEDs to enhance survival rates.
Targeted public health initiatives that address regional disparities and promote widespread CPR training are essential to improving emergency response effectiveness. This study’s national scope and focus on regional variation make it particularly valuable for guiding public health strategies in the Kingdom. While bystander CPR may not have shown a statistically significant adjusted impact on ROSC, its association with improved unadjusted outcomes and its uneven distribution across regions emphasize the importance of addressing social determinants of emergency response readiness.
These findings advocate for a health system approach, integrating community education, EMS logistics, and policy reform, to create a more equitable and effective response to out-of-hospital cardiac arrest nationwide.