Summary
We decided to submit the manuscript for your consideration since it concerns a very important clinical problem. This paper may be of significant importance since, to the best of our knowledge it is the first to present data concerning coronary artery disease (CAD) in patients treated with transcatheter aortic valve implantation (TAVI) based on the endpoints suggested by the VARC. The incidence of CAD was found not to affect the in-hospital and 1-year outcomes of treatment of patients suffering from AS using TAVI.
Introduction
Developed by Alan Cribier in 2002, transcatheter aortic valve implantation (TAVI) has been commonly used to treat severe aortic stenosis (AS) in selected groups of patients [1]. It has been shown that this method improves survival in inoperable patients [2]. The TAVI procedures in high-risk surgical patients were found to be equivalent – and, in some studies, even better – in terms of survival compared with surgical aortic valve replacement (SAVR) [3, 4]. There has been a trend to use TAVI in younger patients characterized by lower risk [5, 6]. The 2017 guidelines of the European Society of Cardiology (ESC) expanded the scope of TAVI indications to include intermediate-risk patients [7]. It appears that the long-term effects of treating patients with TAVI may be affected by both valve durability and, most importantly, the progression of coronary artery disease (CAD) if present. The incidence of CAD increases with age; therefore, higher prevalence of CAD in patients who underwent TAVI is understandable. It is estimated that 25–50% of patients who were treated with SAVR and 40–75% of patients who received TAVI suffer from CAD [8]. Patients who underwent TAVI include patients after myocardial infarction, coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI). The PCI had been performed before TAVI in 11–23% of the patients as a complex part of treatment of patients suffering from AS and CAD [9–12]. The occurrence of CAD in patients who underwent SAVR doubles the risk of mortality during the perioperative period (from 2.5–3.7% to 4.5–6.1%) [13]. It should be stressed that TAVI procedures are performed in patients with even higher surgical risk. The occurrence of CAD in patients treated with TAVI may increase in-hospital and long-term mortality; however, the data from the literature concerning 1-year observations are ambiguous [10–12, 14–17].
Aim
The objective of this study was to evaluate the effect of CAD in patients who underwent TAVI on the outcomes of treatment in the in-hospital period and during 1-year observation.
Material and methods
The TAVI Registry in our hospital is a prospective study, collecting data of patients suffering from severe AS who were referred for TAVI. The aim of the registry is to monitor the outcomes for patients treated with TAVI in terms of safety, efficacy and cost-effectiveness.
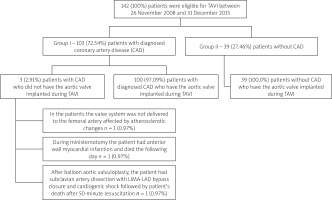
Between 26 November 2008 and 31 December 2015, 142 patients were treated with TAVI. This group included patients suffering from severe symptomatic AS with the aortic valve area of < 1 cm2 and/or < 0.6 cm2/m2, determined through echocardiography, and with a high surgical risk (> 20% according to the Logistic EuroSCORE and/or > 10% according to the Society of Thoracic Surgeons (STS)), or inoperable patients. Other patients with lower surgical risk were also treated with TAVI. They were suffering from comorbidities which were not included in the risk scores, e.g. liver insufficiency, porcelain aorta, conditions after radiation therapy, frailty (Figure 1).
Figure 1
General characteristics of patients eligible for transcatheter aortic valve implantation (TAVI)
All patients gave informed consent for participation in the study. The TAVI was performed in a Cardiac Catheterization Laboratory or a Hybrid Operating Room. The valve was implanted via transapical, direct aortic, subclavian or transfemoral access. Transapical, direct aortic, subclavian and certain transfemoral procedures were performed under general anesthesia with surgical exposure of the access site. Other transfemoral access procedures were carried out percutaneously under local anesthesia with sedation and using vascular closure devices. 109 (77.9%) CoreValve and Evolut R aortic valves (Medtronic, Minneapolis, MN, USA), sizes 26, 29, 31 and 34, were implanted, and 31 (22.1%) Edwards SAPIEN and Edwards SAPIEN XT (Edwards Lifesciences, Irvine, California, USA) aortic valves, sizes 23, 26 and 29, were implanted. The procedures were performed as a routine TAVI as described elsewhere [18–20]. According to the decision of the Heart Team, some patients had received balloon aortic valvuloplasty (BAV) as a bridge to TAVI, and some had their planned PCI performed as a complex treatment of patients with CAD and AS. Patients with stenosis of the main branches of coronary arteries at > 70% of the diameter were selected by the Heart Team as eligible for these procedures [7, 21].
The patients were divided into two groups. Group I comprised 103 (72.5%) patients with diagnosed CAD. This group included patients after PCI, CABG, with a history of myocardial infarction, and patients with stenosis of at least one coronary artery at ≥ 50% of its diameter. The remaining 39 (27.5%) patients constituted group II – non-CAD (Table I).
Table I
Clinical characteristics of patients and procedural data
VARC-2 criteria were applied to assess the outcomes [22].
The patients were evaluated during hospitalization as well as 30 days, 6 months and 12 months after the procedure at the outpatient clinic.
Statistical analysis
The numerical data obtained during the study were expressed as mean and standard deviation. The Kolmogorov-Smirnov test was used to evaluate the similarity of distributions to the normal distribution. If the distribution of two variables in a pair was similar to the normal distribution, Student’s t-test was used for independent and dependent variables. Differences between qualitative parameters were assessed based on the χ2 test with Yates’s correction, and Fisher’s test was applied in the case of small groups. Cumulative event rates were estimated by means of the Kaplan-Meier method. The log-rank test was applied to compare the survival curves. The level of statistical significance was p < 0.05. Statistica 10 software was used to perform the calculations.
Results
The study group was selected out of 253 patients qualified for TAVI/AVR by the Heart Team. One hundred and forty-two patients eligible for TAVI were selected for the analysis.
Patients were divided according to the presence of CAD. Group I comprised 103 (72.5%) patients with diagnosed CAD. The remaining 39 (27.5%) patients constituted group II – without CAD.
Twenty-five (24.3%) patients from group I underwent PCI before TAVI as a complex treatment of AS and CAD. The PCI was performed as a staged procedure in 22 (21.4%) patients – PCI first, followed by TAVI after several days/weeks. PCI and TAVI were performed in one stage in 3 (2.9%) patients. TAVI was performed in 20 (14.1%) patients via transapical access, in 8 (5.6%) patients via direct aortic access, in 25 (17.6%) patients via subclavian access, and in 89 (62.7%) patients via transfemoral access. 105 (75.5%) CoreValve aortic valves, 3 (2.2%) Evolut R aortic valves, 23 (16.5%) Edwards Sapien aortic valves, and 8 (5.8%) Edwards Sapien XT aortic valves were implanted.
Table I shows the characteristics of the study groups. The patients with CAD were characterized by a significantly higher surgical risk according to the Standard (11.3 ±2.6 vs. 9.0 ±2.3, p < 0.001) and the Logistic EuroSCORE (25.7 ±14.0% vs. 16.1 ±8.7%, p < 0.001), higher incidence of hypertension (77.7% vs. 56.4%, p = 0.0118) and a higher rate of pacemaker implantation prior to the procedure (23.3% vs. 7.7%, p = 0.0345).
The echocardiographic data before and after TAVI are presented in Table II.
Table II
Echocardiographic data before TAVI, echocardiographic data during 30-day observation after TAVI and 1-year observation after TAVI
Thirty-day mortality was 8 (7.8% ) in group I and 2 (5.1%) in group II (p = NS). One-year mortality was 22 (21.4%) and 6 (15.4%) in group I and II, respectively (p = NS).
The data were analyzed according to the VARC-2 criteria, which comprised device success, 30-day TAVI safety and clinical efficacy of TAVI within 1 year [22].
The composite endpoint evaluating the efficacy of the aortic valve implantation was achieved in 82 (79.6%) CAD patients and in 31 (79.5%) non-CAD patients (p = NS) (Table III).
Table III
Composite endpoint evaluating the efficacy of aortic valve implantation; composite endpoint – 30-day observation; composite endpoint – 1-year evaluation of the clinical efficacy of transcatheter aortic valve implantation
| Parameter | Group I(n = 103) | Group II(n = 39) | P-value |
|---|---|---|---|
| Device success: | |||
| Absence of procedural mortality | 102 (99%) | 38 (97.4%) | NS |
| Correct positioning of a single prosthetic aortic valve into the proper anatomical location | 99 (96.1%) | 38 (97.4%) | NS |
| Intended performance of the prosthetic aortic valve (no prosthesis – patient severe mismatch and mean aortic valve gradient < 20 mm Hg or peak velocity < 3 m/s, and no moderate or severe prosthetic valve regurgitation) | 87 (84.5%) | 31 (79.5%) | NS |
| Composite endpoints (expressed as number of patients) | 21 (20.4%) | 8 (20.5%) | NS |
| Early safety (at 30 days): | |||
| All-cause mortality | 8 (7.8%) | 2 (5.1%) | NS |
| Stroke (disabling and non-disabling) | 3 (2.9%) | 1 (2.6%) | NS |
| Life-threatening hemorrhaging | 26 (25.2%) | 10 (25.6%) | NS |
| Acute kidney injury – stage 2 or 3 (including renal replacement therapy) | 8 (7.8%) | 2 (5.1%) | NS |
| Coronary artery obstruction requiring intervention | 0 (0%) | 0 (0%) | NS |
| Major vascular complication | 12 (11.7%) | 2 (5.1%) | NS |
| Valve-related dysfunction requiring another procedure (BAV, TAVI or SAVR) | 0 (0%) | 0 (0%) | NS |
| Composite endpoints (expressed as number of patients) | 39 (37.86%) | 12 (30.77%) | NS |
| Clinical efficacy (1-year evaluation): | |||
| All-cause mortality | 22 (21.4%) | 6 (15.4%) | NS |
| Stroke (disabling and non-disabling) | 3 (2.9%) | 2 (5.1%) | NS |
| Requiring hospitalizations for valve-related symptoms or worsening congestive heart failure | 14 (16.86%)* | 4 (15.4%)** | NS |
| NYHA class III or IV | 14 (16.86%)* | 2 (7.7%)** | NS |
| Valve-related dysfunction (mean aortic valve gradient ≥ 20 mm Hg, EOA ≤ 0.9–1.1 cm2 and/or DVI 0.35 m/s, and/or moderate or severe prosthetic valve regurgitation) | 14 (17.28%)*** | 5 (19.2%)** | NS |
| Composite endpoints (expressed as number of patients) | 49 (47.6%) | 14 (35.9%) | NS |
The secondary composite endpoint, which comprised early safety during 30-day observation, occurred in 39 (37.86%) patients of the CAD group and in 12 (30.77%) patients of the non-CAD group (p = NS) (Table III).
The tertiary composite endpoint occurred in 48 (57.8%) patients from group I, and in 13 (48.1%) patients from group II (p = NS) (Table III).
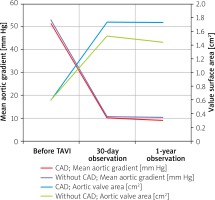
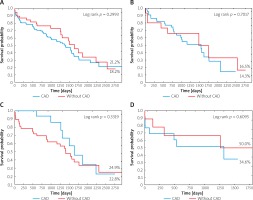
The survival curves are shown in Figure 2. There were no differences between the patients with and without CAD or between separate age groups in terms of survival.
Figure 2
A – Survival curves of patients with and without CAD; B – survival curves of patients with CAD and without it aged ≥ 80; C – survival curves of patients with CAD and without it aged ≥ 70 but < 80; D – survival curves of patients with CAD and without it aged < 70
Echocardiographic results are shown in Figure 3. Both groups experienced a significant reduction of the mean aortic valve gradient and an increase in the aortic valve area and indexed area. These changes were maintained in the case of 30-day and 1-year observations. There were no significant differences in this regard between group I and II, except for a significantly lower left ventricular ejection fraction during 1-year observation in group I (Table II).
Discussion
This paper presents data concerning CAD in patients treated with TAVI based on the endpoints suggested by the VARC. We found that the occurrence of CAD did not affect the in-hospital and 1-year outcomes of treatment of patients suffering from AS treated with TAVI. In the whole study group the prevalence of CAD was 72.5%, which is one of the highest to be found in the literature [4]. According to the literature, CAD was diagnosed in 25–50% of patients with severe AS and in 40–75% of patients undergoing TAVI depending on the criteria adopted for CAD diagnosis [8]. In this paper, we applied the criterion of stenosis of over 50% in major pericardial arteries in coronary angiograms performed before TAVI. Although it may seem quite liberal, this study involved a considerable number of patients who had a history of myocardial infarction – 51 (35.9%), CABG – 42 (29.6%) or PCI – 83 (58.5%). Similar criteria were adopted by Masson et al. and Abdel-Wahab et al. [10, 23]. Patients with CAD are characterized by a significantly higher surgical risk according to the Standard and Logistic EuroSCORE or the STS scores. This is caused by a higher incidence of factors associated with atherosclerosis that increase the risk calculated with these scores. The above-mentioned factors include extracardiac arteriopathy, previous cardiac surgery, myocardial infarction up to 90 days before the procedure, and reduced ejection fraction.
The outcomes for TAVI patients with and without CAD are varied in the literature. In a study from 2010, performed on a group of 171 patients with and without CAD, Dewey et al. demonstrated a higher risk of 30-day (13.1% and 1.2%, p = 0.002, respectively) and 1-year mortality (35.7% and 18.4%, p = 0.01, respectively) among patients with CABG and PCI [14]. In a group of 164 TAVI patients, Khawaja et al. revealed a similarly higher mortality in CAD patients (CAD defined as over-70% stenosis of coronary arteries, or over-50% in the case of the left main coronary artery). Thirty-day mortality was 16.7% and 3.8% respectively, and mortality after 1 year was 31.5% vs. 14.4% [17]. In addition, Huczek et al., based on the PolTAVI registry, demonstrated a higher risk of death in patients with CAD treated with TAVI in comparison with patients without CAD in mid-term observation (8.7% vs. 5.1%, log-rank p = 0.039) [24]. However, the outcomes of numerous other studies did not show the impact of CAD on the prognosis for patients who underwent TAVI [8, 10–12, 15, 16].
Several issues must be taken into account in order to discuss these discrepancies. First of all, this may result from the inadequacy of risk scores used to evaluate patients admitted for cardiac surgery, but not for TAVI. The TAVI is significantly less risky for patients, especially in the case of percutaneous TAVI under deep sedation and when the safest access route may be applied. It seems necessary to develop dedicated risk calculators exclusively for TAVI. Furthermore, the issue concerning the risk of mortality associated with CAD in patients after TAVI should be addressed. Based on the studies mentioned below, CAD as a risk factor itself has a limited impact on survival in short- and mid-term observations as compared to other factors presented in TAVI patients. According to the GARY registry, 1-year mortality among patients who underwent TAVI is 19.9% [25]. This is an outcome comparable to the outcome achieved by us. The GARY registry indicated that among the pre-operative factors, 1-year mortality is affected by the following: higher risk according to the Logistic EuroSCORE, previous mitral insufficiency ≥ grade 2, low-gradient AS, previous decompensation, previous myocardial infarction, renal failure, NYHA class IV, female gender. Among procedural and postprocedural factors, the following were associated with a poorer prognosis: intraprocedural conversion to surgery, peri-interventional stroke, residual aortic insufficiency ≥ grade 2, post-intervention myocardial infarction and pulmonary embolism. A registry from the UK indicates that 1-year mortality between 2007 and 2009 was 21.4%, whereas 3-year mortality was 38.8%. The independent risk factors of mortality within 3 years included renal insufficiency, a Logistic EuroSCORE of ≥ 18.5%, chronic lung disease and low ejection fraction. Within 5 years, the mortality risk factors additionally included coronary artery disease and age [26].
On the basis of these registries, it may be concluded that CAD is a mortality risk factor only after 5 years in the UK registry, while in the GARY registry CAD is expressed in the form of such factors as previous or post-intervention myocardial infarction.
Such a limited impact of CAD on the outcomes of TAVI, not only in the registries but also in the above-mentioned clinical studies, may result from pre-TAVI revascularization by means of either previous CABG or PCI. Both PCI and CABG performed prior to TAVI may cause the proportion of patients with full revascularization before TAVI to be high, and therefore their prognosis to be better [27]. Likewise, patients suffering only from stable CAD instead of AS exhibit good prognoses after successful revascularization. Serruys et al. argue that in patients with three-vessel coronary artery disease with or without left main involvement, the incidence of repeat revascularization or death within 1-year observation is 13.5% and 4.4% in the case of PCI, and 5.9% and 3.5% respectively in the case of CABG. The average age of the patients and the risk according to EuroSCORE were 65.2 ±9.7 years and 3.8 ±2.6% in the case of PCI and 65.0 ±9.8 years and 3.8 ±2.7% in the case of CABG, respectively [28].
On the other hand, the authors of the SYNTAX study found that the incidence of repeat revascularization and death within 5 years was 25.9% and 13.9% in the case of PCI, and 13.7% and 11.4% in the case of CABG, respectively [29]. Based on this study, it can be expected that the necessity of additional revascularization of coronary arteries within 5 years would be 11.7–25.9%.
The mortality rate of the SYNTAX study patients with complete revascularization is low even 5 years after the index procedure as compared to the high mortality rate after TAVI in the UK registry [26]. In addition, on the basis of their 3.5-year observation, Rodes-Cabau et al. [30] argued that half of the deaths of the patients who had undergone TAVI were due to extracardiac causes, whereas myocardial infarction, as a cardiac cause, resulted in a mortality rate of 3.9%.
It is likely that 3–6 months of post-procedural treatment with a dual antiplatelet therapy (DAPT) in patients after TAVI may usually contribute to lower mortality in those who also suffer from CAD. Patients who were treated with PCI during or before TAVI receive a prolonged (up to 12 months) DAPT [31].
On the basis of the presented outcomes, CAD cannot be considered as a factor that worsens the short-term and mid-term prognosis for patients treated with TAVI as opposed to CAD patients undergoing SAVR [32]. Our population was a high-risk surgery group according to the risk scores, and the presented results pertain to patients of this particular risk profile. It is likely that after switching to intermediate- and low-risk patients admitted for TAVI, the presence of CAD may affect the prognosis in a different way. This possibility should be investigated further.
Conclusions
Patients with CAD are characterized by a significantly higher risk of surgical treatment, higher incidence of hypertension and likelihood of a pacemaker implanted prior to the procedure during selection and qualification for TAVI. The short- and mid-term outcomes for high-risk TAVI patients with and without CAD are comparable.