Introduction
Smoking is clearly documented as the most important etiological factor in the development of lung cancer. Eighty-ninety-four percent of patients suffering from lung cancer are smokers or past smokers with on average 30–50 pack-years of tobacco use [1–4]. Smoking may also increase pulmonary and circulatory morbidity after various types of surgery, which is caused by chronic bronchitis and atherosclerosis of coronary vessels induced by tobacco smoke. According to several authors, postoperative complications occur 1.4 to 4.3 times more frequently among smokers in comparison with non-smokers [4, 5]. It seems that the most prone to morbidity are patients undergoing a lung cancer resection who did not quit smoking prior to surgery. The morbidity rate among surgically treated lung cancer patients varies between 10% and 50% in the case of lobectomy and 35% to 80% after pneumonectomy [6, 7]. the majority of clinicians are confident that smoking cessation causes undeniable health benefits and it is indicated at each stage of diagnosis and treatment regimens among patients with lung cancer [8]. On the other hand, there are inconsistent reports about the significance of smoking cessation in the short preoperative period, i.e. a few days or weeks before the planned surgical procedure [4, 9, 10]. Some reports even suggest a paradoxical increase in the pulmonary complication rate among patients who quit smoking just before surgery, and the authors of these reports recommend surgery deferral up to 8 weeks from the cessation if possible [9, 11].
Aim
The aim of this study was to evaluate the impact of smoking cessation and its moment in the preoperative period on frequency and type of postoperative complications in patients treated surgically due to non-small cell lung cancer (NSCLC).
Material and methods
Two hundred eighty-six patients surgically treated for NSCLC in 2010–2015 were analyzed in this study. Informed consent was obtained from each patient and the study was approved by the Ethics Committee. The history of smoking was obtained before the procedure using a self-report questionnaire. The data about surgical procedures and postoperative complications were collected from medical files of thoracic surgery, intensive care unit departments and outpatient clinics. The patients were divided into five groups depending on prior smoking history:
group I – current smokers and past smokers who quit smoking less than 2 weeks before surgery (n = 67),
group II – past smokers who quit 2 weeks to 3 months before surgery (n = 106),
group III – past smokers who quit 3 months to 1 year before surgery (n = 30),
group IV – past smokers who quit more than 1 year before surgery (n = 71),
group V – lifelong non-smokers: patients who have never smoked (n = 12).
In preoperative functional assessment of the respiratory system and circulatory system the following tests were performed: pulmonary function tests, capillary blood gases, diffusing capacity of the lung for carbon monoxide (DLCO), 6-minute walk test, stair climb test, ECG, echocardiography. Surgical procedures were performed under general intravenous anesthesia with double-lumen intubation of the right and left bronchi and through anterolateral thoracotomy (n = 214) or VATS (video-assisted thoracoscopic surgery) (n = 72).
The following pulmonary complications were encountered: postoperative pneumonia, atelectasis that required fiberoptic bronchoscopy, respiratory failure with prolonged mechanical ventilation or need for reintubation, pulmonary embolism, prolonged air leak more than 5 days, residual pneumothorax and bronchopleural fistula.
Myocardial infarction, cardiac arrhythmias and hypotonia with need for catecholamine infusion were defined as cardiac complications.
All complications occurred during postoperative hospitalization or up to 30 days after surgery.
Statistical analysis
Statistical analysis was conducted using Statistica 10 software (TIBCO Software Inc. Palo Alto, CA, USA). Mann-Whitney U test, χ2 test with Yates correction, Spearman test and segment regression test were used. For all tests the statistical significance level was set at p = 0.05.
Results
There were 198 men and 88 women aged 29 to 81 (average 63) in the analyzed group of patients. Two hundred and four patients underwent lobectomy, 36 pneumonectomy, 33 bilobectomy and 13 wedge resection. Histopathological examination revealed squamous cell carcinoma in 150 cases, adenocarcinoma in 111 cases, giant cell carcinoma in 20 cases and carcinoid in 5 cases. The cancer staging system followed the 7th edition of the TNM classification (UICC 2009). In 58.4% of patients there were no metastases in regional lymph nodes, in 26.6% metastases in N1 lymph nodes were observed and in 15% N2 disease was confirmed. Neoadjuvant (induction) chemotherapy was used in a group of 14 patients (4.9%). Table I shows demographic and clinical data of the analyzed population.
Table I
Demographic and clinical data
Among 286 analyzed patients 274 (95.8%) were smokers or past smokers. Only 12 (4.2%) were lifelong non-smokers. Two hundred and thirty-two (81.1%) patients quit smoking before surgery, including 164 less than 1 year before surgery (1–40 weeks, mean: 9 weeks). Sixty-eight patients discontinued smoking more than a year before surgery (1–30 years, mean: 9.8 years). Data of smoking history are presented in Table II.
Table II
Smoking history data
In groups of current smokers and past smokers (groups I, II, III, IV) the majority were male. In the group of life-long non-smokers (group V) the number of men and women was equal. The average age was the lowest in group V (61 years) and the highest in group IV (66 years). The lowest average amount of pack-years was observed in group IV (32.9) whereas the highest was in group II (39.4). The shortest total duration of smoking was noted in group IV (average 36 years) whereas the longest was in group III (average 46 years). Squamous cell cancer constituted the majority in all groups of smokers (groups I, II, III, IV) whereas in group V adenocarcinoma was most frequently confirmed. The most frequent surgical procedure in each group was lobectomy.
Complications during the postoperative period occurred in 115 (40.2%) patients. Pulmonary complications occurred in 61 (21.3%) patients, circulatory in 51 (17.8%) and other complications in 19 (6.6%). Types and rates of individual complications are presented in Table III. Mann-Whitney U test showed no significant differences between groups with and without pulmonary complications, respectively in: number of smoked cigarettes per day (p = 0.354), duration of smoking (p = 0.975), pack-years (p = 0.917) and moment of smoking cessation (p = 0.466). Similarly, there were no significant differences between groups with and without circulatory complications, respectively in: number of daily smoked cigarettes (p = 0.746), duration of smoking (p = 0.382), pack-years (p = 0.932) and moment of smoking cessation (p = 0.528). Spearman rank correlation showed no significant relationship between circulatory morbidity and: number of smoked cigarettes (p = 0.705), duration of smoking (p = 0.387), pack-years (p = 0.946). Similarly, there was no correlation between pulmonary morbidity and: number of smoked cigarettes (p = 0.368), duration of smoking (p = 1.000) and pack-years (p = 0.905). Moreover, this test showed no significant correlation between moment of smoking cessation and pulmonary (p = 0.443) or circulatory morbidity (p = 0.543).
Table III
Postoperative complications
Pulmonary and circulatory complication rates among individual groups of patients are presented in Table IV. Statistical analysis showed no significant differences in morbidity between groups. The χ2 test with Yates correction showed no significant difference between occurrence of pulmonary complications among never smokers (1 from 12 patients – 8.3%) and among current smokers or past smokers (59 from 274 patients – 21.5%) (p = 0.461).
Table IV
Incidence of pulmonary and circulatory complications among individual groups of patients
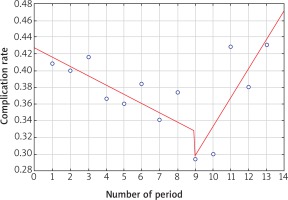
There was an analysis conducted to define the period of time in which smoking cessation is associated with the smallest complication rate. Complication rates were calculated in 3-week periods up to the 12th week of cessation before surgery and then one period from the 11th to the 52nd week and one period after the 11th week of smoking cessation before surgery. It was calculated to compensate for the unequal number of patients in groups and conduct significant statistical analysis of segmental regression. A breaking point was noted in the 9th period; i.e. among patients who quit smoking between 8 and 10 weeks before surgery the complication rate was the smallest. Analysis showed decreasing complication rates from the 1st period to the 9th period (p = 0.026) and from the 9th to the 13th period complication rates increased (p = 0.040). Calculations are presented in Table V and Figure 1.
Discussion
Studies conducted on populations of patients who underwent various surgical procedures prove that smoking is, beside age, type of surgery, and coexistent diseases, a crucial factor related to increased postoperative complication rate [8, 9, 11, 12]. Mills et al. in a meta-analysis of 15 randomized studies and 6 observational studies confirmed a decrease in complication risk altogether, pulmonary complication risk and wound healing complication risk among patients who quit smoking before surgery [8]. The influence of tobacco smoking on occurrence of complications concerns mainly pulmonary complications, because long-term exposure to components of tobacco smoke contributes to an increase in the serum carboxyhemoglobin level, chronic bronchitis, dysfunction of ciliated epithelium, increase in thick secretion in the respiratory tree and dysfunction of macrophages in lungs, which reduces the efficiency of local defense mechanisms [12–14]. Patients suffering from lung cancer who are qualified for surgical treatment are particularly susceptible to pulmonary complications because 90% of them are long-term smokers and surgery involving resection of part or the whole lung leads to restriction of respiratory function. Moreover, long-term smoking is a frequent cause of coexistent COPD and ischemic heart disease. Thirty-four percent of patients suffering from lung cancer are treated for COPD and 10% suffer from coronary artery disease [15–17]. In a prospective study conducted by Mason et al. including 7965 patients surgically treated for lung cancer the mortality among smokers or past smokers was 5 times higher than that among never smokers (1.5% vs. 0.3%) [18] even though in several other studies a significant difference in perioperative mortality between smokers and never smokers was not found [4, 6, 19]. Smoking cessation in the long term causes undeniable health benefits, but the impact of cessation in the period shortly before surgery on complication risk decrease is considered ambiguous among researchers. The majority of clinicians are convinced of the benefits caused by smoking cessation even in the immediate period before surgery. On the other hand, the authors of a few studies noted a paradoxical increase in complication rate among patients who quit smoking within a few weeks before surgery [9, 11, 18]. Myers explains this fact by an increase in thick secretion production and decrease in cough reflex directly after smoking cessation, which causes higher risk of atelectasis and postoperative pneumonia [20]. The question arises whether to advise smoking cessation in the group of long-term smokers shortly before surgery, exposing them to additional stress and in that case which moment to quit is the most beneficial considering potential complications. Bluman et al. analyzed a group of 410 patients who underwent surgical procedures in the field of general surgery, orthopedics, urology, cardiac surgery and vascular surgery, noting a higher pulmonary complication rate among current smokers in comparison to patients who quit at least 2 weeks before surgery and never smokers (22%, 12.8%, 4.9%, respectively). However. in the group of smokers there was noted 6.7 times greater risk of pulmonary complications among patients who reduced smoking immediately before surgery in comparison to the group continuing smoking up to the day of the operation. Patients who quit smoking within 4 weeks before surgery had a greater risk of pulmonary complications the closer the day of cessation was to the surgery [9]. Warner et al. recommend 8 weeks and Nakagawa et al. at least a 4-week period of smoking abstinence before surgery to lower the risk of pulmonary complications [11, 12]. Furthermore, Barrera et al. during analysis of 300 patients who underwent anatomical lung resection due to primary or secondary neoplasm did not observe an increase in pulmonary complication frequency in the group that quit smoking in the last 2 months before the surgical procedure. The pulmonary complication rate and postoperative pneumonia frequency were significantly lower in the group of never smokers in comparison to recent smokers and past smokers and the low value of postoperative predicted DLCO and smoking more than 60 pack-years were significant factors which increased the pulmonary complication risk [4]. Likewise, a meta-analysis conducted by Wong et al. including 25 studies (21 381 patients who underwent various types of surgery including thoracic surgery and cardiac surgery) proved greater relative risk of pulmonary complications among patients who smoked to the day of the operation in comparison to never smokers. The pulmonary complication risk among patients who quit smoking more than 4 weeks before surgery was significantly lower in comparison to patients who did not quit before the operation and in the case of more than 8 weeks of abstinence, risk was comparable to never smokers. The authors did not observe significant differences between groups of smokers and never smokers according to cardiovascular complications and the moment of cessation had no influence on risk of occurrence of these complications [21].
In our study, in the group of 286 patients surgically treated for NSCLC, duration of smoking as well as number of smoked cigarettes had no significant influence on the frequency of all complications or on incidence of either pulmonary or circulatory complications. Although the rate of pulmonary complications among never smokers was notably lower than among current smokers and past smokers (8.3% vs. 21.5%, respectively), the difference was not statistically significant. However, it should be underlined that there was a small number of never smokers in the study group (12 out of 286 patients), which could affect the results of statistical analysis. Similarly, Shimizu et al. in a group of 194 patients surgically treated for lung cancer did not observe significant relations between history of smoking and complication rate [22]. The authors explain the fact of a low postoperative complication rate among never smokers and smokers by more frequent detection of early stage lung tumors thanks to screening programs using a low-dose CT scan, which causes an increase in the rate of videothoracoscopic resections, regularly decreasing the number of pneumonectomies and extensive procedures as well as causing a noticeable improvement of perioperative care, effective COPD treatment, implementation of a respiratory rehabilitation program and precise functional assessment during qualification for surgery. In Barrera’s and Nakagawa’s previously cited studies, there were differences in the frequency of respiratory complications between the groups of smokers and non-smokers; however, similarly to our work, between individual subgroups of smokers separated according to the history of smoking such differences were not observed [4, 12]. Results of analysis conducted in our study confirm the opinions presented in the other studies that the preoperative time of smoking abstinence should be at least 8 weeks. Likewise in the present study segmental regression analysis of individual periods in the preoperative time proves that the most beneficial moment for smoking cessation is the time between 8 and 10 weeks before surgery. According to British recommendations, the latency time between the general physician’s suspicion of lung cancer and surgical treatment should not exceed 2 months. In Polish healthcare system conditions this period is 2 to 6.5 months [23]. This time should be effectively used to persuade patients to quit smoking from the beginning of the diagnostic process, which may lead to a decrease in postoperative complication risk.
Conclusions
Among patients surgically treated for NSCLC, duration of smoking and number of smoked cigarettes have no significant influence on frequency and type of postoperative complications. Based on our analysis, we conclude that the best moment to quit smoking before the operation is the period between the 8th and the 10th week preceding surgery.