Mediastinal tumors are relatively rare lesions and are characterized by wide morphological diversity. For this reason, their diagnosis may be a challenge, requiring a multi-specialist approach and a good anatomical knowledge of the mediastinum (superior, anterior, middle and posterior compartments). Examples of mediastinal tumors include thymic lesions, nonthymic cysts, lymphomas, germinal cell tumors, benign connective tumors and undifferentiated malignant tumors [1]. Among them, chest wall tumors are a very rare group of mediastinal tumors, representing less than 5% of all thoracic malignancies. They can arise from mediastinal soft tissues or skeletal structures, and about 20% of them are diagnosed incidentally on imaging studies. These lesions require oncologic vigilance, as up to 50% of them may present malignant character [2].
In this report, we present an example of a posterior mediastinal tumor that was nonspecific on imaging studies and the difficulties arising from postoperative examinations of the collected material, summarized by a short literature overview about this group of thoraco-oncological lesions. A 34-year-old patient was admitted to our Clinic of Thoracic Surgery due to a nodular lesion involving most of the right lung field detected incidentally in a chest X-ray performed 2 weeks earlier. The patient was in good general condition and did not present with symptoms of local tumor growth, cough, hemoptysis, shortness of breath, chest pain, or general symptoms such as fever, night sweat, pruritus, sudden weight loss, or deterioration of physical performance. The patient suffered from chronic hypothyroidism and allergic rhinosinusitis, and there was a family history of lung cancer.
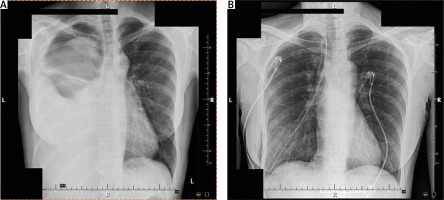
The chest X-rays performed in posterior-anterior (PA) projection and left lateral projections revealed a significant amount of fluid in the right pleural cavity, shadowing in the upper part of the pleural cavity that may have represented a tumor lesion, and displacement of mediastinal structures to the left side (Figure 1 A).
Additionally, chest computed tomography (CT) confirmed the presence of fluid, mediastinal shift, flattening of the right hemidiaphragm and compression of the right lung. Furthermore, a circular and well-demarcated extrapulmonary lesion was described on the posterior wall of the right pleural cavity at the level of ribs IV to VII with the largest dimension of approximately 9 cm. The nature of the lesion was heterogeneous with enhancement in the solid parts; it was vascularized from the intercostal arteries and presented single calcifications. Adjacent skeletal structures showed no signs of destructive infiltration, the left lung and pleural cavity remained without pathological changes, and mediastinal hilar lymph nodes were not enlarged. A diagnosis of extrapulmonary mediastinal tumor of thoracic anatomical structure origin was made, and the patient was referred for surgical resection.
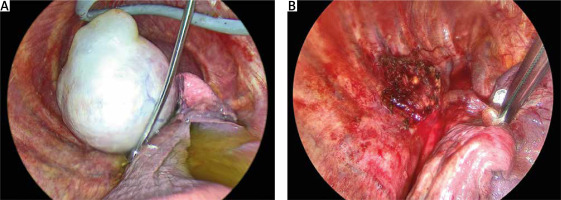
Under general anesthesia, skin incisions were made for the video-assisted thoracoscopic surgery (VATS) procedure, and 1500 ml of clear, straw-colored fluid was urgently aspirated from the right pleural cavity. A whitish encapsulated tumor, 12–15 cm in diameter, adjacent to the posterior mediastinum and associated with the spinal column, was visualized, and an additional 1200 ml of fluid was aspirated. The tumor pedicle attached to the 4th and 5th thoracic vertebrae was identified and cut with a bipolar electrosurgical instrument; the tumor was separated from the spine and removed (Figure 2). Hemostasis was controlled with tissue adhesive, a drain was placed, and the material (fluid, tumor) was sent for examination. The postoperative course was uncomplicated, with chest X-rays confirming normal lung fields without the presence of fluid or any pathological findings (Figure 1 B).
Cytology of the pleural fluid revealed numerous groups of atypical epithelioid cells that did not correspond to Schwann benign nerve sheath tumor characteristic of that location, but to unidentified malignant tumor cells. However, tumor histopathology unequivocally specified schwannoma cells. At the follow-up visit, due to the discrepancy in the results, a positron emission tomography (PET) scan of the chest was administered. It showed no features of malignant pleural neoplasm, and complementary radiotherapy was abandoned.
Mediastinal schwannoma is a rare tumor of this area; its mediastinal incidence is estimated at about 9% of all cases of this tumor originating from the peripheral nerve sheath. Typical symptoms that may occur include shortness of breath, coughing or chest discomfort, but an asymptomatic course is also possible. The tumor is a benign lesion, and thoracic surgery remains the gold standard treatment [3]. Despite this, cases of malignant tumors of the nerve sheath origin, also called malignant schwannomas, are also described in the literature. These rare tumors can typically arise from a neurofibroma, but formation from a benign schwannoma is also not excluded. Such tumors present malignant cells with large hyperchromatic twisted nuclei, showing aggressive tissue infiltration and foci of necrosis [4]. The case described here showed a non-aggressive mediastinal schwannoma, but these tumors can also have a component of atypical cystic degeneration, hypercellularity, necrosis, or presence of hemorrhages. For this reason, these mediastinal tumors can appear as malignancies, and some rare subtypes (e.g. cellular schwannoma) can even be misdiagnosed as sarcomas [4, 5]. The presence of atypical malignant cells in pleural fluid described in this report may result from the aforementioned factors. There are also reports of extremely rare cases of infected schwannoma, when inflammation can explain the presence of fluid with pathological cells, often with necrotic changes that may raise suspicion of neoplastic transformation. A similar pleural fluid pattern could be observed in malignant tumors such as mesothelioma, but it may also result from transformation of benign lesions [6, 7]. In the present case, the PET scan did not show pleural metastasis, but in the case of rare mediastinal tumors, it is always worth considering them as a significant oncological problem and applying more frequent follow-up visits after treatment.