A 75-year-old man was hospitalized due to symptoms of infective endocarditis (IE), including fever and weight loss, persisting for 2 months. Five years earlier, the patient received a Medtronic Hancock II 25 mm biological aortic valve and a 34 mm Maquet vascular prosthesis during ascending aortic aneurysm repair. Furthermore, a TAVI-in-valve procedure was carried out 3 months earlier due to symptomatic, severe stenosis of the prosthetic valve (Medtronic Evolut R 26 mm). IE symptoms appeared 1 month after the procedure. Laboratory tests revealed elevated C-reactive protein, leukocytosis and anemia. Transthoracic (TTE) and transesophageal (TEE) echocardiography revealed a well-saturated lesion measuring 15 × 20 mm in the aortic valve annulus. Cardiac computer tomography (CT), which was performed 2 days after TEE, confirmed vegetations (8 × 4 mm) on the graft leaflet and changes that could correspond to washed-out perivalvular abscesses on the aortic valve annulus (Figure 1 A). Streptococcus gallolyticus was grown in blood cultures. We administered empirical antibiotic therapy with ampicillin and cloxacillin, continuing ampicillin alone after obtaining an antibiogram. The inflammatory markers continued to decrease during the treatment and the control blood cultures were sterile. The patient has received apixaban 2 × 5 mg due to atrial fibrillation.
Figure 1
A – Computed tomography image of the heart before the acute coronary syndrome episode, with lesion on the graft leaflet from the left main coronary artery side indicated. B – Computed tomography image of the heart after an episode of acute coronary syndrome, with lesion on the graft leaflet from the left main coronary artery side indicated. C – Blocked left superficial femoral artery. D – Left superficial femoral artery after thrombectomy and stent implantation. E – Embolism material in the left main coronary artery trunk. F – Left main coronary artery (LM) image after balloon angioplasty within LM trifurcation, with small embolic material in the peripheral left anterior descending artery segment indicated
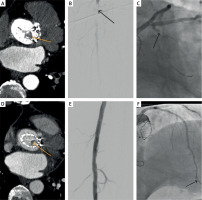
In the third week of hospitalization, symptoms of acute ischemia of the left lower limb occurred. The arteriography, performed urgently, showed embolic material within the left superficial femoral artery. Doctors performed a mechanical thrombectomy using Rotarex and implanted a stent. The procedure achieved an optimal effect, fully restoring arterial flow (Figures 1 C, D).
Two days later, the patient experienced severe chest pain with hypotension and changes in the electrocardiogram – ST segment depressions in II, III, aVF and elevation in aVR. Emergency coronary angiography revealed embolic material at the trifurcation site of the left main coronary artery (LM), almost completely occluding its lumen (Figure 1 E). After inserting the EBU 3.756F catheter (ClimberTerumo) and the Asahi SionBlue guidewire into the left anterior descending branch (LAD), the operator attempted to aspirate the embolic material using a standard aspiration catheter. However, due to its size, hardness, and difficult access, it was ineffective.
Due to the deteriorating general condition of the patient and development of cardiogenic shock, the operator attempted to displace the embolic material to the smallest branch of the trunk–the circumflex branch (Cx). He introduced another SionBlue guidewire into the intermediate branch (RI) and then, using slow dilations with an NC3.0/15 mm balloon (PanteraLeo, Biotronik) to 14 atm in the distal part of the LM towards the LAD and the RI, moved the embolic material to the Cx. Eptifibatide bolus i.c. and i.v. infusion were administered. We observed improved flow in the LAD and RI (with only small embolic fragments remaining in the distal LAD segment) (Figure 1 F).
The patient’s general condition gradually improved. The follow-up TTE showed no significant decrease in the left ventricular ejection fraction; it remained about 40%. Akinesis of only two segments appeared: the apical and basal segment of the lateral wall. A follow-up CT scan revealed a much smaller lesion in the graft (Figure 1 B). In the following days, we continued antibiotics (for 43 days), along with anticoagulant (apixaban) and antiplatelet therapy (clopidogrel). The patient’s discharge home, in fairly good condition, occurred 20 days after the acute coronary syndrome.
ST-elevation myocardial infarction [1, 2] or acute limb ischemia [3] may be linked to IE. These conditions in IE patients following TAVI-in-valve procedures are reported here for the first time.








