Introduction
Renal cell carcinoma (RCC) accounts for 3–5% of all malignancies and about 80% of renal malignancies [1]. At the time of diagnosis of RCC, about 30% of patients have metastases [2]. Renal cell carcinoma metastases commonly affect the lungs, liver, bones, and brain [3] and extremely rarely the vagina – there are less than 100 cases described in the literature [2].
We describe a case of a 60-year-old patient referred for treatment in our clinic due to the presence of a tumour mass in the vagina with severe bleeding. Subsequently, this turned out to be a metastasis from RCC.
Case report
A 60-year-old patient was referred to the Gynaecological Oncology Clinic at Dr. Georgi Stranski University Hospital, Pleven, due to a tumour formation in the vagina, which bled profusely during a gynaecological examination. The patient did not report any previous surgeries or illnesses. The gynaecological examination showed an intense bleeding, soft tumour formation with dimensions 4/6 cm at the entrance of introitus vaginae (Fig. 1).
Blood tests showed normal indicators except for haemoglobin – 90.0 and platelets – 641.0.
The tumour formation was excised en bloc with clear margins.
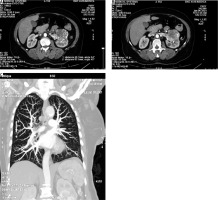
Postoperatively, a whole-body computed tomography (CT) was performed (because the removed formation did not appear like a primary carcinoma of the vagina). The computed tomography scan showed pathological changes in the left kidney and lungs. A lobulated, heterogeneous tumour formation in the middle third of the left kidney, measuring 63/55 mm (Fig. 2 A), and infiltration with tumour thrombosis of the left renal vein (Fig. 2 B) was manifested. In the lungs, bilateral, mostly apical nodular lesions up to 3 mm in size were detected. A solid nodule with dimensions of 7 mm was visualized along the right intralobular fissure (Fig. 2 C).
Fig 2
Computed tomography imaging. A) computed tomography finding with tumour formation; B) infiltration of the left renal vein with tumour thrombosis; C) solid nodule along the right intralobular fissure
The patient was discharged on the second day after recovery from anaemic syndrome without complications.
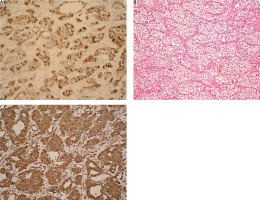
The histological results of the surgical intervention are – soft tissues with metastases of clear-cell renal cell carcinoma, necrosis, and haemorrhage (Fig. 3).
Fig 3
Histological findings. A) moderate expression of epithelial membrane antigen, ICH 100×; B) metastasis of clear-cell renal cell carcinoma, forming acinar structures of cells with abundant cytoplasm and centrally located monomorphic nuclei, He 100×; C) strong positivity in the tumour population, Vimentin 100×
After diagnosis, the patient was referred to a urology clinic for further treatment.
Discussion
Globally, renal cancer is the seventh most common cancer in men and the tenth most common cancer in women [1]. RCC accounts for 3% of all adult malignancies and 85% of all primary renal tumours [4]. Renal cell carcinoma is the most common renal carcinoma and the second most common urological carcinoma [5]. Renal cell carcinoma metastasizes in about 30% of cases [6, 7] and can be lymphatic, haematogenous, transcoelomic, or by direct invasion [8]. Most commonly, it affects the lungs, bones, adrenal glands, liver, lymph nodes, and brain [2]. Much less often, it can metastasize to the thyroid, orbit, nasal structures, vagina, gallbladder, pancreas, sublingual tissues, and soft tissues of distal extremities [8]. Metastases can be synchronous – 18%, and metachronous – 50% [9]. Vaginal metastases are extremely rare in RCC. Even less common is its primary manifestation as a vaginal tumour [2, 10, 11]. When RCC metastasizes to the vagina, the formation is usually single, located in the lower one-third of the vagina [12]. Carcinomas metastasizing to the vagina usually originate in the left kidney – tumour emboli passing through the left renal vein to the ovarian vein and uterovaginal plexus [13].
In 1906, Penham described the first case of RCC- associated vaginal metastasis [14]. Since then, less than 100 such cases have been described in the literature, and RCC has been primarily manifested with vaginal metastasis in only 3 of them.
In our case we report an RCC originating from the left kidney and metastasizing to the lower third of the vagina. Regardless of the size of the primary tumour, the patient had no complaints until she found a formation at the entrance to the vagina. This formation bled excessively during the subsequent gynaecological examination, necessitating the patient to be referred to our clinic. Due to the unusual appearance of the formation, we suspected that it was not a primary vaginal tumour. However, we removed it radically because patient presented with heavy bleeding and anaemia. For this reason, a whole-body CT scan was performed immediately after surgery – a renal carcinoma was diagnosis of radiologists. After the histological diagnosis, the patient was referred for further treatment.












