Variables that contribute to elevated risk during percutaneous coronary intervention (PCI) have been well defined and can be categorized into two major groups: 1) patient-specific, such as advanced age, poor left ventricular function, severe comorbidities, clinical presentation with acute coronary syndrome or cardiogenic shock; and 2) procedural-specific, such as complex anatomy, involvement of left main coronary artery or major bifurcations, heavy calcifications, chronic total occlusions, last patent vessel. Clinical features make these patients at high risk for standard coronary artery bypass grafting; nonetheless, they are also at high risk of intra-procedural complications with PCI and, whenever they are left untreated, they face a poor prognosis. High-risk PCI remains a challenge in modern interventional cardiology.
Catheter-based devices for mechanical circulatory support (MCS) aim both to overcome the inability of the heart to provide an adequate output and to sustain blood circulation and hemodynamics (Table I). Mechanistically, left ventricular support devices unload the failing left ventricle by reducing pre-load (volume unloading), after-load (pressure unloading) or both, whereas circulatory support increases mean arterial blood pressure. The ultimate goal is to improve or maintain myocardial, cerebral, mesenteric, renal, and peripheral tissue perfusion. MCS devices are routinely used during procedures on complex, higher-risk and indicated patients (CHIP), which are currently referred to as “protected PCI”. CHIP may frequently suffer intra-procedural sustained hypotension, which in turn jeopardizes coronary perfusion gradient. Loss of coronary perfusion leads to profound myocardial ischemia, which quickly depresses the already impaired left ventricle and may lead to cardiovascular collapse and cardiac arrest.
Table I
Overview of mechanical cardiac support (MCS) devices
Intra-aortic balloon pump (IABP) is the simplest form of MCS (Table I). IABP aims to augment coronary and systemic blood flow during diastole while decreasing myocardial oxygen consumption and both left ventricular wall stress and workload. It only modestly enhances cardiac output. The demonstration of the protective role of elective IABP in protected PCI is still a controversial issue. Beyond historical positive data from observational studies [1], the largest randomized trial so far, the Balloon Pump-Assisted Coronary Intervention Study (BCIS-1), yielded negative results in the short term [2], but demonstrated a 34% relative reduction in all-cause mortality at a median follow-up of 51 months [3]. Despite discouraging evidence also in the setting of cardiogenic shock complicating acute myocardial infarction [4] and a class III European recommendation for routine IABP use in this setting [5], IABP is still widely used during elective complex PCI [6]. IABP is actually an inexpensive, readily available device that is associated with ease of use and post-implantation management and a low incidence of thrombotic and bleeding complications [7].
More complex and invasive MCS systems (Table I), such as Impella (Abiomed, Danvers, Massachusetts) devices, provide a definitely higher hemodynamic support and – in the pivotal randomized trial – yielded a reduction of post-discharge major adverse events and an improvement in ventricular function and heart failure symptoms [8]. However, Impella or even Veno-Arterial Extra Corporeal Membrane Oxygenation (VA-ECMO) devices require large-bore vascular access (Table I), which entail an appropriate learning curve and are associated with a high burden of complications [9]. Moreover, technical feasibility of vascular access remains a key issue for MCS device implantation as these patients frequently have tortuosity and extensively calcific disease in the ilio-femoral arteries that create additional challenges to the interventionalist. Recent non-randomized data, although flawed by possible unmeasured residual confounding, have raised questions about the association of Impella devices with higher rates of adverse events and costs [10]. Although VA-ECMO provides full cardiopulmonary support, it may require left ventricular venting or unloading to prevent increased myocardial oxygen demand secondary to high filling pressures and volume induced by circulatory support, which can precipitate further myocardial ischemia. This imposes additional complexity on management because a second device aimed at reducing afterload (either IABP or Impella) may be needed beyond the support of an experienced cardiac perfusionist.
Basically, the unmet need in high-risk complex PCI is to achieve stable procedural hemodynamics with few hypotensive events, allowing for more extensive atherectomy and greater and more complete revascularization, which is expected to provide long-term benefits [11]. An illustrative case of IABP-protected PCI is presented in the Figure 1. To this purpose, the authors of the elegant randomized single-center study published in the present issue [12] of Advances in Interventional Cardiology/Postępy w Kardiologii Interwencyjnej investigated whether IABP assistance with a 10 ml larger than standard (MEGA) balloon provides better clinical results or, at least, an improvement in hemodynamic support in CHIP undergoing high-risk PCI as compared with standard IABP or with no support. Notably, patients with cardiogenic shock or recent acute coronary syndrome were excluded per the protocol; therefore the results apply only to non-emergent elective procedures.
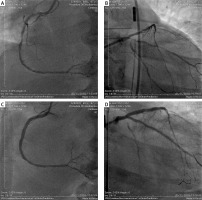
Figure 1
An illustrative example of complete revascularization with IABP-protected PCI in a diabetic 67-year-old male CHIP with stage IV chronic kidney disease, poor left ventricular function and recent pulmonary edema, having received surgical turndown. Top panels, baseline angiography demonstrating significant lesions in right coronary artery (A) and critical calcific disease involving left main bifurcation, left anterior descending and circumflex arteries (B). Bottom panels, final result after implantation of 2 long drug-eluting stents (DES) in right coronary artery (C) and, after extensive rotational atherectomy, implantation of 2 DES in the left main bifurcation with double-kissing crush technique and 1 additional DES in left anterior descending and circumflex arteries (D)
Being small in magnitude (n = 36), this study did not have the power to detect any difference in hard end-points across randomized groups, which were as high as expected (in-hospital MACE 19%, in-hospital major bleeding 33%, cardiovascular death during follow-up 25%). However, the authors have to be commended for having used a separate arterial line to constantly record arterial pressure in order to define a new hemodynamic composite endpoint. Interestingly, they observed a trend towards lower hypotension load and maximum hypotensive episodes with MEGA balloon, that mechanistically led to less periprocedural myocardial damage.
To observe hemodynamic parameters is indeed a crucial issue during protected PCI and to set hemodynamic endpoints may represent a new line of research.
Cardiac power output [(cardiac ouput × mean arterial pressure)/451] [13], expressed in watts, couples both adequacy of systemic blood flow and maintenance of appropriate blood pressure (flow domain and pressure domain of the cardiovascular system, respectively), and thus is a reliable measure of cardiac pumping function. Together with serial biochemical evaluation of arterial lactate, which expresses the inadequacy of tissue perfusion, cardiac power output can be used to define, diagnose and accurately monitor cardiogenic shock. In turn, cardiogenic shock is the natural setting to evaluate the different hemodynamic performances of MCS devices. Yet, it appears not realistic in the setting of an elective protected PCI, as complex and risky as possible but lasting no more than a few hours, the attempt to implement such a complex evaluation that requires pulmonary artery catheterization and prolonged multiparametric observation. Beat by beat evaluation of cardiac power (PWR) is the continuous equivalent of cardiac power output (CPO) but still requires clinical validation and additional invasiveness [14].
Ultimately, hypotensive episodes demonstrated by continuous arterial pressure monitoring may represent a reasonable surrogate indicator of transient coronary and end-organ hypoperfusion. In the pivotal trial of Impella, indeed, the intra-procedural decrease in mean arterial pressure was consistent with the reduction of cardiac power output [15].
In conclusion, given the limited prospective, randomized, multicenter data with use of advanced MCS in protected PCI and despite the contemporary increasing use [10], the relative role of the diverse, commercially available MCS devices in patients undergoing high-risk PCI is yet to be completely defined. However, we hardly can expect new conclusive evidence because of the difficulties and the ethical implications in performing randomized studies in this setting. In addition, the lack of a reliable risk tool to indicate use of MCS during PCI is an unmet need that warrants further research. IABP remains the easiest and fastest MCS device with the lowest rate of complications and the lowest complexity in post-implantation management. This still makes IABP irreplaceable in all those contexts in which drug therapy alone is not sufficient to support and stabilize hemodynamics and at the same time the use of more invasive devices is not feasible. A small additional IABP balloon volume is a promising option to provide a simple, cheap and effective increase in hemodynamic support that deserves confirmation in larger prospective studies. To use a separate arterial line during CHIP procedures makes it possible to constantly calculate derivative parameters that may prove useful as surrogate indicators of hemodynamic derangement in the era of modern MCS.







