Summary
Levels of kinesiophobia are high in patients with coronary artery disease, especially in those with a history of myocardial infarction. Kinesiophobia is associated with shortness of breath and disease duration, while angina is the only significant predictor of kinesiophobia in patients with coronary artery disease. Kinesiophobia is a predictor of physical performance and health-related quality of life in coronary artery disease.
Introduction
The most recent European Cardiovascular Statistics show that cardiovascular diseases (CVD) are the leading cause of mortality in Europe especially in middle-income countries [1]. Turkey is among the countries with high cardiovascular mortality, in which CVD was the leading cause of death (36.8% of all deaths) in 2019 [2, 3]. Mortality due to CVD is projected to increase by about 2.3 fold in males and about 1.8 fold in females by 2030 due to aging and increased rates of diabetes and obesity [4, 5]. In addition to hypertension, tobacco use, obesity, hypercholesterolaemia, and diabetes, sedentary lifestyle is an important modifiable risk factor for CVD. The latest European Society of Cardiology guideline highlights the importance of physical activity (PA) and exercise as a part of optimizing lifestyle for the prevention of CVD [6]. However, the World Health Organization estimates that 60% to 85% of people in the world have sedentary lifestyles, and insufficient PA causes almost 3.5% of all deaths each year [7]. Similarly to the general population, the PA level is far from ideal in patients with CVD. The percentage of cardiac patients performing the recommended amount of PA has been reported to be 17% [8].
Barriers for ideal PA level after a cardiac event potentially include anxiety and fear of movement, also called as kinesiophobia, which is “an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to painful injury or re-injury”, which was first described for chronic musculoskeletal pain [9, 10]. There are limited data regarding fear of movement in patients with CVD, who tend to have a high level of kinesiophobia, probably based on the anxiety and inability to cope with fear of exercising, which that may trigger their symptoms – mostly angina, resulting in an avoidance of activity or movement. In 2 studies, the level of kinesiophobia was reported to be high among 45.5% and 20% of the study populations, including cardiac patients [11, 12]. Elevated levels of kinesiophobia and fear avoidance belief to PA were also detected in patients with coronary artery disease (CAD) and rheumatic heart disease [13].
Regular PA and exercise have been proven to prevent and manage CVD. Kinesiophobia might be an important factor for PA and exercise restrictions in this population. We believe that identifying predictors of kinesiophobia and high-risk patients will help to prevent sedentary behaviour and increase exercise participation among cardiac patients.
Aim
The objectives of the study were as follows: 1) evaluate kinesiophobia, 2) investigate its relationship with physical performance, patients’ symptoms and limitations, health-related quality of life (HRQOL), and disease history; 3) determine predictors of kinesiophobia; and 4) explore the degree to which kinesiophobia is associated with physical performance and HRQOL in patients with CAD.
Material and methods
Fifty-two patients previously or newly diagnosed with CAD by the Department of Cardiology, Izmir Katip Celebi University, Atatürk Training and Research Hospital between December 2020 and April 2021 were enrolled in this cross-sectional study. All the patients were hospitalized in the Cardiology Inpatient Unit in were physiologically and clinically stable during the study period. Twelve (23.1%) patients received medical therapy alone, while 35 of them (67.3%) had undergone percutaneous coronary intervention (PCI) of one vessel (n = 26, 74.3%), 2 vessels (n = 8, 22.8%) and 3 vessels (n = 1, 2.9%) for the right coronary artery (n = 16, 30.8%), left anterior descending artery (n = 15, 28.8%), and circumflex artery (n = 14, 26.9%). Median time since PCI was 3 months. Moreover, 5 (9.6%) patients had a history of coronary artery bypass graft (CABG) surgery, while 4 of them were candidates for CABG. Median time since CABG was 11 months. Within the whole group, 23 (44.2%) patients had a history of myocardial infarction (MI). The medications of the patients were as follows: antithrombotics (63.7%), β-blockers (51.9%), statins (42.3%), ACE inhibitors (37.2%), calcium channel blockers (26.9%), antidiabetics (21.2%), angiotensin receptor blockers (7.7%), nitrates (7.7%), and diuretics (5.8%).
Exclusion criteria were as follows: unstable angina, coronary artery bypass graft (CABG) ≤ 3 months, left ventricular ejection fraction < 45%, severe aortic stenosis, systolic blood pressure > 180 mm Hg and diastolic blood pressure > 120 mm Hg, 2nd or 3rd atrioventricular block, acute pulmonary embolism, deep vein thrombosis, pulmonary oedema, acute respiratory failure, and musculoskeletal or neurological disorders limiting the application of physical performance tests.
The study was conducted in accordance with the ethical standards of the Helsinki Declaration and was approved by the Institutional Non-Invasive Research Ethics Board (2020/29-50, Protocol Number: 5821-GOA). All the participants gave written consent to participate in the study after receiving appropriate verbal and written information.
Demographic (age, gender, body mass index) and clinical variables (time of diagnosis, left ventricular ejection fraction, medications, etc.) were recorded. The level of kinesiophobia was measured using the Turkish version of the Tampa Scale of Kinesiophobia for Heart (TSK-H) [14]. The scale consists of 17 items and 4 sub-dimensions measuring kinesiophobia associated with cardiac disease and the avoidance exercise. Each item is scored based on a 4-point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). The total score varies between 17 and 68. Higher scores indicate a higher level of kinesiophobia. A cut-off score of 37 points is used to define low levels of kinesiophobia (< 37 points) and high levels of kinesiophobia (≥ 37 points) [15]. The intraclass correlation coefficient of the original scale was 0.83, and Cronbach’s α was 0.78, while Cronbach’s α for the Turkish version was 0.75. The 5× Sit-to-Stand (5-STS) test, Timed Up and Go (TUG) test, and 6-Minute Walk Test (6-MWT) were used to assess physical performance. The 5-STS test is an outcome measure used to determine mobility, functional lower extremity strength, and balance capacity. The test was performed with the patients’ hips and knees flexed at 90° and feet in contact with the ground, sitting in a chair (42–45 cm) without arm support. The patients were asked to get up and sit down 5 times as quickly as possible, and the time to complete the test was recorded [16]. TUG test was used to assess mobility and balance. The patient was asked to get up from a chair (42–45 cm), walk 3 m to a marked point at their usual pace, return to the chair, and sit down again. The test was timed from the instruction “go” to when the patient was seated [17]. 6-MWT test was used to evaluate functional capacity of the patients. The test was administered according to the American Thoracic Society guidelines. The participants were asked to walk as fast as possible for 6 min in a 30-metre corridor. During the test, the standard expression “you are doing very well” was used to encourage the patient every minute, and the 6-minute walking distance was recorded at the end of the test [18]. The expected 6-MWT distances according to age, gender, height, and body weight were calculated according to the reference values described in the study of Enright and Sherrill [19]. Patients’ symptoms and limitations, and HRQOL were assessed with the Turkish version of the Cardiovascular Limitations and Symptoms Profile (CLASP). The CLASP consists of 37 items, with 4 main symptom areas, including angina, shortness of breath, ankle swelling, and tiredness, and 5 sub-domains of functional capacity (mobility, social life and leisure activities, activities within the home, concerns and worries, and gender) [20]. The Likert-type scale is assessed for both physical and functional domains. Each subdomain, which includes 4–6 questions, is evaluated individually. The questions are evaluated as “normal”, “mild”, “moderate”, and “severe” according to the level of functional disorder. The obtained scores vary for each subdomain: angina – 5–15, shortness of breath – 5–14, ankle swelling – 3–10, tiredness – 3–9, mobility – 4–16, social life and leisure activities – 3–7, activities within the home – 4–12, concerns and worries – 3–12, and gender (female and male) – 3-12. The quality of life decreases as the scores increase. Cronbach’s α values were found to be 0.92 for CLASP total, 0.81 for angina, 0.92 for shortness of breath, 0.97 for ankle swelling, 0.93 for tiredness, 0.88 for mobility, 0.85 for social life activities, 0.70 for activities within the home, 0.80 for concerns and worries, and 0.94 for gender [20].
Statistical analysis
All data were analysed using the Statistical Package for Social Sciences statistical software package (version 23.0, IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test and histograms were used to check normality of distribution. Continuous variables were presented as median and interquartile ranges (25th–75th percentile) because most of the data were not normally distributed. Categorical variables were presented as numbers and percentages. Spearman’s correlation coefficient was used to assess the correlations between kinesiophobia, physical performance, patients’ limitations and symptoms, HRQOL, age, and disease duration. The strength of correlations was classified as very weak (r = 0–0.19), weak (r = 0.2–0.39), moderate (r = 0.40–0.59), strong (r = 0.6–0.79), and very strong (r = 0.8–1). To identify predictors of kinesiophobia in patients with CAD, multiple regression analysis was used. We used simple linear regression analysis to explore the degree to which kinesiophobia is associated with physical performance and HRQOL. The levels of kinesiophobia among patients with and without previous MI were compared using the Mann-Whitney U test, and simple linear regression analyses was also used to assess the effect of previous MI on kinesiophobia. Statistical significance was considered at p < 0.05.
Prior to the study, the power analysis was performed using G Power 3.0.10 software based on the results of the study of Ufuk Yurdalan et al. [21], and a minimum of 43 subjects was found adequate considering 95% (5% type I error level) confidence interval and 80% power.
Results
Fifty-two patients diagnosed with CAD were included in the study (median age 58 years). The demographic and clinical characteristics of the patients are summarized in Table I. Forty-one (78.8%) patients had a history of smoking, 34 (65.4%) patients had hypertension, 21 (40.4%) patients had obesity, 20 (38.5%) patients had diabetes mellitus, and 15 (28.8%) patients had hyperlipidaemia.
Table I
Demographic and clinical characteristics of the patients
[i] Data expressed as median and interquartile range (25th–75th). BMI – body mass index, CAD – coronary artery disease, PCI – percutaneous coronary interventions, CABG – coronary artery by-pass graft, MI – myocardial infarction, LVEF – left ventricular ejection fraction, COPD – chronic obstructive pulmonary disease.
Table II shows the kinesiophobia, physical performance, limitations and symptoms, and HRQOL of the patients. According to the cut-off score of TSK-H (≥ 37 points), 43 (87.2%) patients presented high levels of kinesiophobia. The CLASP scores indicated normal level for shortness of breath, mild levels of angina and tiredness, mild limitations in physical and social functions, and moderate levels of concerns and worries (Table II).
Table II
Kinesiophobia, physical performance, limitations, symptoms, and health-related quality of life in patients with CAD
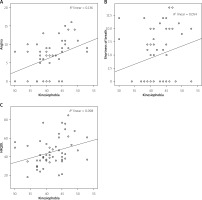
There was a moderate positive correlation between kinesiophobia and 5-STS duration (r = 0.480, p < 0.001), while kinesiophobia was strongly and positively correlated with TUG test duration (r = 0.634, p < 0.001) (Figures 1 A, B). A strong negative correlation was found between kinesiophobia and 6-MWT distance (r = –0.621, p < 0.001) (Figure 1 C). There were positive correlations between kinesiophobia and angina (r = 0.424, p = 0.002), shortness of breath (r = 0.302, p = 0.029), and total CLASP score (r = 0.377, p = 0.006) (Figures 2 A–C, respectively). Duration of CAD was correlated with kinesiophobia (r = 0.379, p = 0.006), 5-STS duration (r = 0.291, p = 0.036), and 6-MWT distance (r = –0.319, p = 0.021). Age was positively correlated with kinesiophobia (r = 0.341, p = 0.013), 5-STS duration (r = 0.425, p = 0.002), and TUG duration (r = 0.559, p < 0.001), while it was negatively correlated with 6-MWT distance (r = –0.531, p < 0.001). All the correlations are presented in Table III.
Table III
Correlations between kinesiophobia, physical performance, patients’ limitations and symptoms, HRQOL, age, and disease duration
| TSK-H | 5 STST | TUGT | 6 MWT | Angina | SoB | HRQOL | CADD | Age | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | p | r | p | r | p | r | p | r | p | r | p | r | p | r | p | r | p | |
| TSK-H | – | – | 0.480 | < 0.001 | 0.634 | < 0.001 | –0.621 | < 0.001 | 0.424 | 0.002§ | 0.302 | 0.029* | 0.377 | 0.006§ | 0.379 | 0.006§ | 0.341 | 0.013* |
| 5 STST | 0.480 | < 0.001 | – | – | 0.724 | < 0.001 | –0.472 | < 0.001 | 0.200 | 0.156 | 0.254 | 0.070 | 0.265 | 0.058 | 0.291 | 0.036* | 0.425 | 0.002§ |
| TUGT | 0.634 | < 0.001 | 0.724 | < 0.001 | – | – | –0.669 | < 0.001 | 0.364 | 0.008§ | 0.339 | 0.014* | 0.327 | 0.018* | 0.217 | 0.123 | 0.559 | < 0.001 |
| 6 MWT | –0.621 | < 0.001 | –0.472 | 0.002§ | –0.669 | < 0.001 | – | – | –0.532 | < 0.001 | –0.284 | 0.041* | –0.498 | < 0.001 | –0.319 | 0.021* | –0.531 | < 0.001 |
| Angina | 0.424 | 0.002§ | 0.200 | 0.156 | 0.364 | 0.008§ | –0.532 | < 0.001 | – | – | 0.149 | 0.292 | 0.564 | < 0.001 | 0.141 | 0.317 | 0.194 | 0.168 |
| SoB | 0.302 | 0.029* | 0.254 | 0.070 | 0.339 | 0.014* | –0.284 | 0.041* | 0.149 | 0.292 | – | – | 0.658 | < 0.001 | 0.055 | 0.697 | 0.072 | 0.614 |
| HRQOL | 0.377 | 0.006§ | 0.265 | 0.058 | 0.327 | 0.018* | –0.498 | < 0.001 | 0.564 | < 0.001 | 0.658 | < 0.001 | – | – | 0.189 | 0.181 | 0.168 | 0.235 |
| CADD | 0.379 | 0.006§ | 0.291 | 0.036 | 0.217 | 0.123 | –0.319 | 0.021* | 0.141 | 0.317 | 0.055 | 0.697 | 0.189 | 0.181 | – | – | 0.336 | 0.015* |
| Age | 0.341 | 0.013* | 0.425 | 0.002§ | 0.559 | < 0.001 | –0.531 | < 0.001 | 0.194 | 0.168 | 0.072 | 0.614 | 0.168 | 0.235 | 0.336 | 0.015* | – | – |
Figure 1
A – Correlation between kinesiophobia and 5-STS test duration. B – Correlation between kinesiophobia and Timed Up and Go Test duration. C – Correlation between kinesiophobia and 6-Minute Walk Test distance
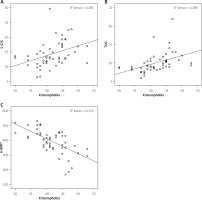
Figure 2
A – Correlation between kinesiophobia and angina. B – Correlation between kinesiophobia and shortness of breath. C – Correlation between kinesiophobia and health-related quality of life
To identify predictors of kinesiophobia (dependent variable) in patients with CAD, multiple regression analysis was used. The model included age, angina, shortness of breath, and disease duration as independent variables, which were significantly associated with kinesiophobia according to Spearman’s correlation coefficients. In the method of regression analysis, all the independent variables are given equal importance in the model. The results of multiple linear regression analysis to determine the predictors of kinesiophobia in CAD patients are shown in Table IV. The Multiple linear regression model summary showed an R2 value of 0.21, which indicates that the independent variables in the model (age, angina, shortness of breath, and disease duration) predict 21% of the variance in the extent of kinesiophobia. The assumptions related to the regression analysis, including normality, linearity, independency, homoscedasticity, and multicollinearity were examined and found to be unviolated. The F statistics value was less than 0.05, indicating that the overall model was fit. Variance Inflation factor values were less than 10, while tolerance values were greater than 0.20, indicating no multicollinearity in the model. Among the entire independent variables, only angina was a significant predictor of kinesiophobia (β = 0.33, t[47] = 2.56, p < 0.05, pr2 = 0.12). Therefore, for every unit increase in angina, kinesiophobia increased by 0.35 units (Table IV).
Table IV
Predictors of kinesiophobia in patients with coronary artery disease
| Model | Unstandardized coefficients | Standardized coefficients | 95.0% confidence interval | Collinearity statistics | |||||
|---|---|---|---|---|---|---|---|---|---|
| B | Std. error | Beta | T | Sig. | Lower bound | Upper bound | Tolerance | Variance inflation factor | |
| (Constant) | 33.58 | 3.7 | 9.08 | 0.000* | 26.143 | 41.02 | |||
| Age | 0.07 | 0.07 | 0.13 | 0.98 | 0.333 | –0.07 | 0.21 | 0.86 | 1.16 |
| Angina score | 0.35 | 0.14 | 0.37 | 2.55 | 0.014* | 0.07 | 0.62 | 0.94 | 1.06 |
| Shortness of breath score | 0.20 | 0.13 | 0.19 | 1.50 | 0.142 | –0.07 | 0.45 | 0.98 | 1.02 |
| Disease duration | 0.02 | 0.01 | 0.26 | 2.01 | 0.051 | 0.00 | 0.04 | 0.90 | 1.11 |
| F | 4.48 | 0.004§ | |||||||
We also used simple linear regression analysis to explore the degree to which kinesiophobia is associated with physical performance and HRQOL. In each model kinesiophobia was the independent variable, while 5-STS test duration, TUG test duration, 6-MWT distance, and HRQOL were dependent variables. The assumptions related to the regression analysis, including normality, linearity, independency, homoscedasticity, and multicollinearity were examined and found to be unviolated. According to each model, kinesiophobia predicts 15% of 5-STS test duration, F (1, 50) = 8.74, p < 0.01, R2 = 0.15; 20% of TUG test duration, F (1, 50) = 12.32, p < 0.01, R2 = 0.20; 38% of 6-MWT distance; F (1, 50) = 30.06, p < 0.001, R2 = 0.38, and 10% of HRQOL, F (1, 50) = 5.43, p < 0.05, R2 = 0.10 (Table V). Kinesiophobia is a significant predictor of both physical performance and HRQOL. For every unit increase in kinesiophobia, 5-STS and TUG test duration increased by 0.33 and 0.24 units, respectively, while 6-MWT distance and HRQOL decreased by 9.93 and 0.97 units, respectively (Table V).
Table V
Effects of kinesiophobia as a predictor of physical performance and health-related quality of life
| Model | Unstandardized coefficients | Standardized coefficients | 95.0% confidence interval | Collinearity statistics | |||||
|---|---|---|---|---|---|---|---|---|---|
| B | Std. error | Beta | T | Sig. | Lower bound | Upper bound | Tolerance | Variance inflation factor | |
| (Constant) | 0.40 | 4.74 | 0.08 | 0.933 | –9.11 | 9.91 | |||
| Kinesiophobia | 0.33 | 0.11 | 0.39 | 2.96 | 0.005§ | 0.11 | 0.56 | 1.00 | 1.00 |
| Dependent variable: 5 STS test duration | |||||||||
| (Constant) | –0.03 | 2.87 | –0.01 | 0.992 | –5.80 | 5.45 | |||
| Kinesiophobia | 0.24 | 0.07 | 0.45 | 3.51 | 0.001§ | 0.10 | 0.38 | 1.00 | 1.00 |
| Dependent variable: TUG test duration | |||||||||
| (Constant) | 806.74 | 76.12 | 10.60 | < 0.001 | 653.83 | 959.63 | |||
| Kinesiophobia | –9.93 | 1.81 | –.61 | –5.48 | < 0.001 | –13.60 | –6.30 | 1.00 | 1.00 |
| Dependent variable: 6-MWT distance | |||||||||
| (Constant) | 4.90 | 17.43 | 0.28 | 0.78 | –30.11 | 39.92 | |||
| Kinesiophobia | 0.97 | 0.42 | 0.31 | 2.33 | 0.024* | 0.13 | 1.80 | 1.00 | 1.00 |
| Dependent variable: Total CLASP score | |||||||||
We also divided our patients into 2 groups according to the presence of previous MI and found a statistically significant difference in terms of TSK-H score. The level of kinesiophobia was higher in patients with previous MI (n = 23, median score 44) compared to patients without a history of MI (n = 29, median score 40) (p = 0.031). However, according to simple linear regression analysis, previous MI was not a predictor for kinesiophobia (p = 0.056).
Discussion
The main finding of the current study indicates a high level of kinesiophobia in patients with CAD, especially in subjects with MI history. Angina is a significant predictor for kinesiophobia, while kinesiophobia significantly and negatively effects physical performance and HRQOL.
Kinesiophobia or fear of movement is an underestimated outcome measure in clinical practice including exercise-based cardiac rehabilitation (CR) among patients with cardiac diseases. However, it is an important factor, which presents in the majority of cardiac patients, often limiting activity and movement at various stages of the disease, and hindering patient compliance to rehabilitation programs. In our CAD patient group, high levels of kinesiophobia were detected in 87.2% of the subjects, which was similar to previously reported ratios including 85.3%, 74.5%, and > 70% [21–23]. Our findings indicate that angina is a significant predictor for kinesiophobia in CAD patients. We used CLASP to evaluate patients’ symptoms and limitations and HRQOL, which differs from other outcome measurements because it identified patient-specific problems such as ankle swelling, shortness of breath, angina, and tiredness, and their severity. Although our patient group presented normal levels of shortness of breath and mild levels of angina, these two symptoms were significantly correlated with kinesiophobia. Moreover, angina was the only significant predictor for kinesiophobia among all other variables. Our results indicate that the beliefs, anxiety, and/or misconceptions among cardiac patients regarding PA and movement potentially aggravate their primary symptoms, probably angina, hence leading to kinesiophobia. The median total score of CLASP was 42 in our patient group (increasing scores indicated lower quality of life). As the level of kinesiophobia increased, HRQOL decreased among our CAD patients, and kinesiophobia was found to be a significant predictor for HRQOL. Similarly to our results, previous studies have reported low levels of HRQOL in CAD patients with high levels of kinesiophobia [12, 22].
Our findings also indicate that kinesiophobia is a predictor of physical performance. In our study, we used the 5-STS test, TUG test, and 6-MWT to evaluate physical performance. The 6-MWT is a widely used clinical test to assess functional capacity in patients with cardiac diseases. In a previous study, 6-MWT distance was negatively associated with kinesiophobia in CABG candidate CAD patients [21]. Similarly, our results have shown a strong negative correlation between 6-MWT distance and kinesiophobia in patients with CAD. The median 6-MWT distance of our patients was 406 m, while the median 6-MWT distance was found to be 481 m among 556 stable coronary heart disease patients in a study by Beatty et al. [24]. Moreover, distances between 87–419 m, including our patients’ median walking distance, were indicated as the lowest test result in that study, which was a significant risk factor for subsequent cardiovascular events [24]. According to the reference values, our patients could achieve 76% of the expected 6-MWT distance, while a walking distance < 82% predicted was considered as “abnormal” [25]. These findings have shown the reduced physical capacity of our patient group. Parallel to our findings, Baykal Şahin et al. reported lower aerobic exercise capacity in CAD patients with a high level of kinesiophobia, compared to those with a low level of kinesiophobia [22]. In addition to the 6-MWT, we used the 5-STS and TUG tests to assess mobility, functional lower extremity strength, and balance capacity. The median duration of the 5-STS test was 13.17 s in our patient group, with a median age of 58 years. According to the reference values for 5-STS test duration, 11.4 s was considered as “normal” for the individuals between 60 and 69 years of age [26]. The median result for TUG test duration was 9.23 s, while 9 s was considered as “normal” for the individuals between 60 and 69 years of age [27]. The physical performance of our patients deteriorated as their age increased. Moreover, our results indicate a relationship between kinesiophobia and physical performance and age. Previous studies have mostly focused on the relationship between fear of movement and the PA level in patients with cardiac diseases [12, 22]. Indeed, there are no data regarding the association between kinesiophobia and physical performance. However, in one study by Bäck et al., patients with high levels of kinesiophobia were found to perform worse in muscle endurance tests compared to patients with low levels of kinesiophobia, which could be assumed to be in relation to physical performance [12]. In the same study, an increase from medium to high level of PA significantly decreased the risk of developing a high level of kinesiophobia in patients with CAD [12]. Although we have not evaluated the PA level in our patient group, we think that possible sedentary behaviour due to kinesiophobia probably had deleterious effects on physical performance parameters. We also found that disease duration was significantly correlated with kinesiophobia, 5-STS test duration, and 6-MWT distance. Similarly, Şahin et al. reported a positive relationship between disease duration and kinesiophobia [22]. These findings suggest that kinesiophobia is not only a problem during acute stages of cardiac diseases but is also present in patients with long disease duration.
The majority of our patient group had undergone PCI (67.3%), while only 5 of them had undergone CABG. Therefore, we are unable to compare the level of kinesiophobia in our patient group according to treatment methods. However, a major surgical approach could potentially increase fear of movement, possibly due to pain, sternal restrictions, and anxiety. Further studies should include more homogenous patient groups to clarify the effects of clinical features on kinesiophobia. However, as an important clinical feature, history of MI resulted in an increase in kinesiophobia in our patient group. CAD patients with a history of MI presented higher levels of kinesiophobia compared to those without previous MI. This finding highlights the necessity of extra attention to overcome fear of movement after MI, to increase participation in activity and exercise-based CR programs. Moreover, development of treatment strategies for excessive fear of movement in patients experiencing MI should be included in multidisciplinary rehabilitative approaches. Similarly to our findings, Bäck et al. reported a significantly higher presence of history of MI in CAD patients with high levels of kinesiophobia compared to patients with low levels of kinesiophobia [12]. Ahlund et al. found a significant reduction in fear-avoidance beliefs among patients with MI attending exercise-based CR compared to the baseline values, indicating the positive effect of exercise-based CR on kinesiophobia [28]. It has been already reported that high levels of kinesiophobia resulted in lower rates of adherence to CR [29]. Moreover, attending CR programs is proven to reduce the level of kinesiophobia [12, 22]. Therefore, we believe that routine clinical assessment and treatment strategies for kinesiophobia in patients with cardiac diseases is of great importance for successful secondary prevention.
The main limitations of our study were the relatively the small sample size and the lack of PA level measurement, which are potentially affected by kinesiophobia. Moreover, physical inactivity may also be a risk factor for lower HRQOL and physical performance in patients with CAD. However, our patient group included the inpatients of a Cardiology Department, and most of the patient-centred, self-report PA measurements rely on the participants’ recall ability, including a particular time (for example the last 7 days). Because the patients were staying at the hospital, these questionnaires could not provide accurate data for the PA level. Further studies including more homogenous patient groups, using objective PA assessments, such as accelerometers, are needed to clarify the possible association between PA level and kinesiophobia. We also could not explore the effect of the treatment method (invasive or surgical) because the majority of our population had undergone PCI (67.3%) while only 9.6% had undergone CABG. Further studies should also be designed to investigate the possible effects of treatment methods and medications specifically on angina, kinesiophobia, physical performance, and HRQOL.
Conclusions
Patients with CAD developed high levels of kinesiophobia, especially those with a history of MI. Disease duration and shortness of breath were positively correlated with kinesiophobia, while angina was a significant predictor of kinesiophobia. Kinesiophobia, itself is also a significant predictor of physical performance and HRQOL in CAD patients.








