Summary
When used by experienced operators, excimer laser coronary artery angioplasty is a well-established therapy that can be used during percutaneous coronary intervention to treat a wide range of coronary lesions including heavily calcified stenosis. The novel Auryon laser system (AngioDynamics, Inc.) uses a 0.9 mm probe specifically designed for percutaneous coronary intervention. The device was previously used only for the treatment of peripheral artery disease; however, there is potential for its use in the treatment of high calcium and complex epicardial stenosis. This study analyzed the effectiveness and safety of laser angioplasty with the Auryon laser for the treatment of heavily calcified lesions.
Introduction
Despite the increasing use of percutaneous coronary intervention (PCI) with drug-eluting stents (DES) for the treatment of obstructive coronary artery disease, not all cases of coronary stenosis can be adequately treated with balloon angioplasty and/or stenting alone [1]. Heavily calcified stenosis can be subjected to various debulking techniques such as non-compliant balloons, cutting or scoring balloons, intravascular lithotripsy (IVL), or rotational atherectomy. With the exception of rotational atherectomy, which requires a dedicated guidewire [2], currently available devices have failed to demonstrate predictable effectiveness in complex fibrocalcific lesions. In this context, excimer laser coronary artery (ELCA) angioplasty is considered a well-established therapy that can be applied to treat a wide range of coronary lesions during PCI when used by experienced operators. Several studies have demonstrated high technical and procedural success rates with low incidence of major adverse cardiac events (MACE) using ELCA therapy [3–5]. Unlike other calcium modification technologies, this technique has the procedural advantage of not requiring any other device to pass through the lesion other than the usual 0.014-inch guidewire. The novel solid-state Auryon laser system [6, 7] (AngioDynamics, Inc.), which uses a 0.9 mm probe favorable for PCI, was previously used only for the treatment of peripheral artery disease (PAD). This study sought to analyze the safety and effectiveness of laser angioplasty with the Auryon laser system for the treatment of heavily calcified coronary lesions. Written in collaboration with and on behalf of the Cardiovascular Laser Society (CLS – www.cardiovascularlasersociety.com), this study introduces the successful use of this innovative device to treat high calcium and complex epicardial stenosis in 20 patients, further advancing the field of laser atherectomy for the percutaneous treatment of complex coronary lesions, as the Auryon laser is the most advanced commercially available device for this condition. The Auryon laser system is an innovative laser with solid state technology (Nd:YAG) and not gaseous like the Philips CVX 300 laser (XeCl). This made it possible to reduce the size of the generator significantly (around 80 kg) and to give particular characteristics to the laser beam produced, which has a wavelength of 355 nm compared to the 308 nm of the Philips system. The Auryon system is designed to provide an optimized wavelength, pulse width, and amplitude to remove lesions while preserving the endothelium of the vessel wall. Table I specifies the technical characteristics of the two systems. The new laser can be set with 2 energy settings: 50 mJ/mm2 and 60 mJ/mm2. The maximum energy generated with the Auryon system is 60 mJ/mm2. The Auryon System is designed to deliver an optimized wavelength, pulse width, and amplitude to remove calcified lesions while preserving vessel wall endothelium. The Auryon System produces a photon energy of 3.5 eV, which is low enough to be nonreactive to vessel endothelium, but high enough to vaporize calcium. The new Auryon laser is much more powerful than the previous one, and for this reason it does not require a contrast medium to amplify the penetration force into the plaque. In essence, this is what differentiates it from others on the market: the greater power of the laser beam, due to which contrast medium is not necessary. However, the greater power is balanced by hyperselectivity for C-C and C-O bonds, which are those that bind the calcium particles. This effect limits the potential action on the rest of the vascular wall and therefore also notably reduces the potential risk of perforation [8, 9].
Table I
Excimer and Auryon laser systems
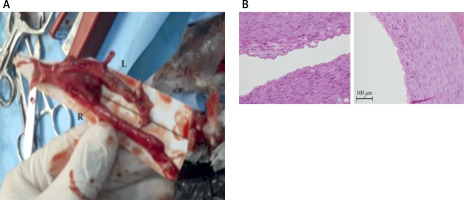
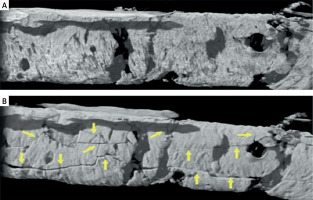
The 355 nm wavelength is important because it is highly absorbed in the blood, resulting in increased photomechanical effects, and absorbed at a shallower depth in the endothelium, resulting in preservation of the vessel wall [10, 11]. Furthermore, the 3.5 eV photon energy produced is high enough to ablate lesions but low enough to preserve the vessel wall [12] with a 3 times higher affinity for the lesion tissue than for the vessel wall, reducing the risk of perforations [13]. The Auryon laser therefore has minimal interaction with the vascular wall, reducing intraprocedural interference (dissection, perforation) to a minimum. It can also avoid the inflammatory response by reducing vascular remodeling [14] and improving long-term patency (Figure 1). The shorter pulse width < 25 ns allows for the delivery of greater power to ablate calcified lesions without the use of high energies and contrast medium as with the Philips system. Plasma formation allows calcium vaporization without thermal ablation [13] (Figure 2). Each tissue type interacts differently with a given wavelength. Longer wavelengths are absorbed at shallower depths than shorter wavelengths, resulting in lower photon energies [12]. Other important factors are pulse width and amplitude. Higher amplitude is achieved with shorter pulses, which can deposit energy before thermal diffusion occurs [15–17]. To localize effects to target tissue without thermal damage, the energy delivered must be faster than the time it takes for heat to spread [12]. The Auryon laser system then allows one to carry out the ablation and simultaneously observe the fluoroscopic image without any interference [14].
Material and methods
The FARO (Laser For complex coronary Artery lesion pReparatiOn) Study is a prospective, single-arm, single-center, pilot study which aimed to: 1) investigate the primary safety endpoint defined as freedom from major adverse events (MAEs) at 30 days from the Auryon laser procedure; 2) assess the primary efficacy endpoint, defined as average reduction in residual diameter stenosis of greater than 50% from baseline prior to any adjunctive therapy achieved by the Auryon laser catheter alone; 3) investigate the effects of angiographic and intravascular optimal coherence tomography (OCT) on the calcific plaque burden; and 4) investigate the effectiveness of the first- and second-generation 0.9 mm Auryon laser catheters. The study received approval from the Ministry of Health and Research Ethics Committee. Patients were not eligible if they were under 18 years of age or had established contraindications such as active cancer, pregnancy, or major bleeding. Inclusion criteria were: 1) moderate/severe coronary calcification (calcium arch from 180° to 270°) or otherwise requiring, according to the judgment of the investigator, rotational atherectomy or IVL; 2) estimated vessel size of 2.5 mm or larger; and 3) the possibility to perform OCT prior to the procedure. A pragmatic sample of 20 patients gave informed consent to participate in the study; we evaluated patient characteristics including age, cardiovascular risk factors, angiographic data (lesion complexity, number of stenoses, chronic total occlusion), calcium arch, thrombolysis in myocardial infarction (TIMI) flow before and after revascularization, PCI success, and acute-stent thrombosis. Intracoronary imaging with OCT at baseline and at the end of the procedure was performed. Angiogram and OCT were assessed by an independent core lab. For this pilot study, we treated the first 5 patients with the first-generation Auryon 0.9 mm catheter, while the remaining patients were treated with the optimized second-generation Auryon 0.9 mm catheter.
Results
A total of 20 subjects (20 lesions) were enrolled. Mean age was 69.2 years and 90% were male. Diabetes mellitus was present in 45% of the enrolled patients (Table II). Mean ± standard deviation (SD) lesion length was 40.1 ±21.4 mm. Lesions were de novo (60%) or in-stent restenosis (ISR) (40%); 25% of patients had under-expanded ISR. Mean ± SD percent stenosis at the target lesion as assessed by the core lab was 85 ±13.1%. Thirty-five percent of the lesions were balloon-uncrossable, while 75% were balloon-undilatable. All lesions were severely calcified as assessed by coronary angiography and intravascular imaging (Table III).
Table II
Demographic and disease characteristics of patients
Table III
Auryon laser system procedure details
Procedural outcomes
A successful result, defined as < 30% residual stenosis and TIMI 3 flow after PCI, was achieved in 95% of cases. Mean ± SD procedural time was 37 ±18 min.
Safety outcomes
One case of perforation of a degenerated saphenous vein graft after high pressure balloon angioplasty dilation, not related to Auryon laser treatment, was resolved after covered stent implantation. In 1 case, a distal embolization was observed after successful left anterior descending (LAD) PCI. One case of transient slow flow after Auryon laser treatment was observed in a patient with severe left ventricular dysfunction, without a hemodynamic effect during an LAD PCI performed with Impella support. Only two flow-limiting vessel dissections after Auryon laser treatment were recorded, but both resolved after subsequent balloon dilation and/or stent implantation. Another distal dissection was related to hydrophilic guidewire manipulation and not related to the laser device. Only 1 case of clinically relevant periprocedural myocardial infarction (with no significant sequelae) was observed. Significant periprocedural myocardial injury was observed in 80% of treated patients, with a mean troponin I peak of 3505 pg/ml after the procedure, which is expected for complex PCI. There were no cases of contrast-induced nephropathy. At a mean ± SD follow-up of 125 ±63 days after execution of laser-assisted PCI, no death or MACE was observed in the study cohort.
Discussion
The Auryon laser (AngioDynamics, Inc.) is a new solid-state third harmonic pulsed Nd:YAG laser system with a long wavelength and short pulse width cleared by the United States Food and Drug Administration for the treatment of infrainguinal arterial disease including ISR. The Auryon laser demonstrates improved ablation safety and efficiency for interventional medical procedures in calcified coronary arteries. The unique physical characteristics of the Auryon laser, including the 355-nm wavelength and a 10- to 25-ns pulse width with 40-Hz frequency, allow for efficient ablation with three times higher affinity for lesion tissue as opposed to vessel endothelium [8]. Furthermore, the Auryon laser can debulk thrombotic to severely calcified atherosclerotic lesions, providing a range of therapeutic potential across the disease severity landscape. Among peripheral artery disease, the Auryon laser provided a low rate of target-lesion revascularization (TLR) at 6-month follow-up in the EX-PAD-03 investigational device exemption study, a low rate of deep dissections, and a low rate of overall bailout stenting. The possibility of sparing adventitial damage, which has been linked to an increase in TLR and restenosis, has contributed to less restenosis and the need for TLR among infrainguinal PAD procedures. This is the first time this system has been used on highly calcified coronary artery occlusions, demonstrating the potential for improved efficacy and safety in coronary artery disease as well. This pilot study explored the theory that laser angioplasty may produce better preparation of severely and complex calcified lesions, leading to a larger final lumen after stent implantation. The first 5 patients underwent this technique with the first-generation 0.9 mm laser catheter, while the remaining 15 patients were treated with the more efficient second-generation 0.9 mm catheter. The second-generation catheter included a hydrophilic coating and a more radiopaque tip. The 0.9 mm catheters are over-the-wire and compatible with any type of 300 cm 0.014-inch guidewire; in the future, we expect a more versatile monorail type probe. The laser system is compact compared to other machines and has a short warm-up time [15–17]. The final results of this pilot study investigating the safety and efficacy of the Auryon laser in this field are encouraging.
Conclusions
The results from this pilot study investigating the use of the Auryon laser for the treatment of heavily calcified lesions are encouraging; positive impressions include the ease of use and the safety and effectiveness in the treatment of severely calcified lesions. Improvements to the 0.9 mm catheter including a monorail type probe with greater flexibility and a more radiopaque tip are anticipated. The Auryon laser is effective and safe in the ablation of atherosclerotic and restenotic tissue of coronary artery disease. The device has a high safety profile including a low risk of distal embolization. However, larger studies are needed to support these initial observations.