Introduction
Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic inflammatory skin disease. Its clinical manifestation is characteristic recurrent, chronic, painful and purulent lesions [1–4]. Purulent inflammation of the apocrine sweat glands may cause a range of negative physical and psychosocial effects [5]. The purulent inflammation of the apocrine sweat glands is obstruction of the follicle-sebaceous follicle. It is initiated by pro-inflammatory cytokines (IL-1β and TNF-α), mediators of activated Th1 and Th17 T helper cells (IFN-γ and IL-17). Moreover, neutrophils, macrophages and plasma cells are involved in the development of the disease [6]. HS mainly affects the areas of the body with blisters, such as the armpits, groins, anus-genital area, buttocks and the sub-nipple area [1, 2]. The exact aetiology and pathogenesis of HS remains unclear [7, 8]. HS may have mild, moderate, and severe courses. Treatment with topical or systemic antibiotics is widely used as the first-line treatment for mild disease in the early stages. In chronic cases (Hurley II/III), surgical methods should be considered [9, 10]. It has been shown that health-related quality of life improves significantly after surgical treatment [11, 12]. The most important aspect of the surgical treatment of HS is a wide excision. Later, the most problematic aspect is the wound closure, due to the wide excision (very large wounds, e.g. buttocks). In such cases, the use of reconstructive techniques such as skin flaps, skin grafts or both is required [9, 10]. In the course of a correct assessment of the diseased area that needs to be excised, there is an urgent need to implement the device that would reliably support the physician’s decision [4]. Such a device might be the laser speckle contrast analysis (LASCA). LASCA can significantly improve the results of surgical treatment and may allow for monitoring of treatment (healing). This is based on preoperative, intraoperative and postoperative studies of patients treated surgically for hidradenitis suppurativa.
Laser speckle contrast analysis is quite a new and unique device which can find applications in multiple diagnostic approaches in dermatology and dermatosurgery. The laser speckle contrast analysis was introduced in 1982 by Briers [13]. Following Briers et al. theoretical and practical description of LASCA works on the following principles: when coherent light enters a tissue and is randomly scattered in it, it produces a random interference pattern called a speckle pattern [14, 15]. If movement is found in the tissue (e.g., erythrocytes in blood vessels), the contrast in the spot pattern will change accordingly as the movement of scattering particles causes shifts in the laser light. This phenomenon can be quantified by computational analysis of the speckle contrast and thus information on the microcirculatory blood flow can be obtained [16, 17]. This process is very complex and results from multiple dispersion of erythrocytes from different parts of the tissue, as well as from the different flow patterns of erythrocytes within the capillaries [15].
Speckle contrast is defined as the ratio of the spatial standard deviation to the mean speckle intensity, is measured to quantify the degree of local blurring in the speckle image, which is directly related to tissue blood perfusion when no or minimal scattering from static tissue elements is present [18].
As a result, LASCA has been proven effective in estimating relative blood flow in the retina [19–21] and exposed brain [22–24] and skin microcirculation [25]. This paper is the world’s first presentation of usefulness of laser speckle contrast analysis in diagnosis and surgical treatment of hidradenitis suppurativa.
Aim
The aim of this study was to evaluate the usefulness of LASCA in the surgical treatment of hidradenitis suppurativa.
Material and methods
In HS surgical treatment at the Centre for Burns Treatment in Siemianowice Śląskie, Poland, in 2019–2022, we performed standard preoperative, intraoperative and postoperative speckle laser examinations to assess the vascular perfusion of the surgical sites. The device used was Laser Speckle Contrast Analysis (Perimed AG). This study included 18 patients treated surgically at the Centre for Burns Treatment in Siemianowice Śląskie with specific LASCA findings. Inclusion criteria: male and female patients with hidradenitis suppurativa I–III grade according to Hurley Scale. Exclusion criteria: pregnant women, breastfeeding women, no cancer within the last 5 years (no history of BCC found), current biological and pharmacological treatment for HS. Surgical treatment consisted of a wide excision of lesions located in the armpits, groin, buttocks and intimate areas. We used the basic and advanced methods of reconstructive surgery available at our Centre: 1) rotation flap reconstruction, 2) autogenous skin grafts, 3) mixed treatment (split thickness skin graft and skin flap reconstruction or split thickness skin graft with Acellular Dermal Matrix). Laser speckle examinations were undertaken pre-operatively, intraoperatively and post-operatively with follow up to 2.5 months after the surgical treatment.
LASCA, also known as laser speckle contrast imaging (LSCI), is a method that instantly visualizes microcirculatory tissue blood perfusion. It is an imaging technique that combines high resolution and high speed. When an object is illuminated by laser light, the backscattered light will form an interference pattern consisting of dark and bright areas. This pattern is called a speckle pattern. If the illuminated object is static, the speckle pattern is stationary. When there is a movement in the object, such as red blood cells in a tissue, the speckle pattern will change over time. A camera with a fixed exposure time will record these changes in the speckle pattern as motion blurring. The LASCA examination was performed on specific days: before admission, immediately before the procedure, immediately after the procedure and in days following the procedure. The measuring device was placed 30 cm from the test object. The examination lasted 20 s, with an image width 20.1 cm, height 19.0 cm; 16 frames, 1 colour photo per 10 s, and resolution 0.78 mm.
Results
Figures 1–4 contain the images of circulatory perfusion of the treated area. Figure 1 represents the process of examination using the LASCA device.
Figure 1
Patient during measurement on LASCA device (patient after reconstruction of buttocks area after wide excision of HS)
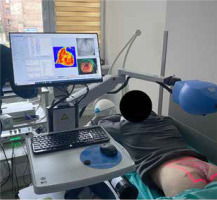
Figure 2
A1–A2 – patient before surgical treatment – image taken in the outpatient clinic. B1–B2 – image taken before the operation (a progression of HS is seen – red colour), C1–C2 – image taken after the surgical procedure (co-graft of ADM and STSG and rotation flap) – pale STSG and pale rotation flap (ischemia) can be seen, D1–D2 – image taken 4 days after the operation, E1–E2 – image taken 2.5 months after surgical treatment (normal healing process), F1–F2 – image taken 3 months after surgical treatment (fully healed)

Figure 3
A1–A2 – patient with HS before the surgical treatment, B1–B2 – image of the right axilla with HS before the wide excision – we found the area without HS and we saved more skin in the rotation flap, C1–C2 – image post-op 3 days after surgical treatment (rotation flap), D1–D2 – image post-op 4 days after surgical treatment – the healing process starts, E1–E2 – image of successfully reconstructed right axilla 2 weeks post-op (normal healing process), F1–F2 – the patient fully healed (2 months post-surgical treatment)

Figure 4
A1–A2 – the patient with HS before admission, B1–B2 – image of the buttocks with HS before the wide excision, C1–C2 – image post-op 3 days after surgical treatment (rotation flap), D1–D2 – 3 weeks after the surgical procedure (progress of the normal healing process), E1–E2 – image 2 months post-op, F1–F2 – the patient fully healed (7 months post-surgical treatment) – no recurrence found in the suspected area

Table 1 shows the results and findings of laser speckle contrast analysis examinations.
Table 1
Basic characteristics of the patients, and results and findings of laser speckle contrast analysis examinations
We classified the results into 3 groups: 1) detected perfusion impairment of the local skin flap after wound closure, 2) assessment of focal HS, and 3) assessment of the healing process.
The group with detected perfusion impairment of the local skin flap after wound closure
Out of 14 cases of local flap ischemia, massive skin flap necrosis was detected in only 1 case. In the remaining cases, intensive PRP (platelet rich plasma) treatment was initiated in addition to anticoagulant therapy (low molecular weight heparins in prophylactic doses). Only 1 case did not respond effectively to treatment. However, we already had a picture of what we can expect to deal with in later stages of treatment in this patient.
Assessment of focal HS
In this group, we found 1 case where the extent of resection was larger before the surgery was originally planned for a very wide excision with split thickness skin graft. However, in the operating theatre, we discovered that the extent of resection could be smaller as the HS foci were localized so that we could save some skin and perform skin local flap reconstruction.
In this group, we also found 1 case, an additional HS focus, which was not visible mid-operatively in the planned extent of skin resection. This led us to perform a complete procedure in the treated area, without leaving a HS focus that was not visible.
Assessment of the healing process
In this group, we present the results of patients in whom we monitored the entire healing process until full healing under the supervision of an outpatient clinic. We were definitely able to assess how the healing process was going, what dressings to use, and we could even give the patient an approximate idea of how much longer it might take.
Discussion
In the surgeon’s daily work, a device that can support diagnostics and assessment of the degree of skin damage in the present wound may be useful. This type of assistance can be especially valuable in the case of HS. Due to the fact that the course of HS may be dynamic and may be characterized by periods of withdrawal and subsequent relapse, there is an urgent need to implement a device in everyday clinical practice that will allow for reliable monitoring of the course of the disease. It may be proposed that LASCA could be such a device. The aim of the study was to present the diagnostic possibilities of the LASCA device in patients suffering from HS. In accordance with the results obtained in our study it might be proposed that LASCA allows for early detection of post-operative complications like ischemia of the local skin flap so that appropriate treatment can be initiated in a timely manner. Laser speckle contrast analysis allows for detection of additional foci that may not be visible. In our study the 14 rotation flaps were prepared. In all cases LASCA was useful in monitoring and evaluating the condition of the flap. In 13 analysed cases the process of healing went without any undesirable events (small ischemia of the flap). However, in 1 case the necrosis of the flap occurred. This phenomenon could be predicted already on day 0 after surgery as the results of the LASCA image analysis revealed a large ischemic area within the lobe. This phenomenon at this stage was not visible in traditional observation. Therefore, it can be concluded that LASCA has proved to be extremely useful in detecting the ischemic necrosis at the early stage. This observation correlates directly with the results of Lyu et al. [26]. Lyu’s research team used LASCA to assess the incidence of ischemic necrosis of flaps in a mouse model. The results clearly showed that the device is useful in the evaluation and monitoring of the healing process [25].
In addition to assessing the healing process, it is very important to correctly assess the area of lesions in order to correctly define the extent of the surgical excision of the diseased tissue. In our study it was found that LASCA might be helpful in adequate assessment of the excision area. In 2 cases it was proved that the resection had to be more extensive than previously planned. It could prevent the early relapse of the disease. Similar results were obtained in the works of other authors. LASCA has been shown to be useful in non-invasive assessment of the extent of cutaneous wound regions [27].
Due to the fact that HS is a rare disease and LASCA is a relatively new diagnostic tool, it is difficult to properly and broadly discuss the results obtained by our team. There is a deficit of research papers on this subject. Nevertheless, on the basis of the obtained results as well as other studies, it can be concluded that LASCA is a useful tool supporting the assessment of the extent of the wound as well as its healing progress. However, further studies using laser speckle contrast analysis in the treatment of hidradenitis suppurativa should be conducted. It is thought that it may have wide applications in dermatological surgery, evaluation of clinical treatments such as biologic drug programs and also in other dermatoses.
Conclusions
LASCA is a great device with which we can evaluate wound healing after surgical procedures (STSG and skin local flaps). LASCA allows for early detection of post-operative complications like ischemia of the local skin flap so that appropriate treatment can be initiated in a timely manner. Laser speckle contrast analysis allows for detection of additional foci that may not be visible. Further studies using laser speckle contrast analysis in the treatment of hidradenitis suppurativa should be conducted. It is thought that it may have wide applications in dermatological surgery, evaluation of clinical treatments such as biologic drug programs and also in other dermatoses. LASCA is a device with which we can evaluate HS lesions before the surgery and the process of wound healing after surgical procedures (STSG and skin local flaps).








