Summary
Restenosis (RS) following percutaneous angioplasty (PTA) of renal artery stenosis (RAS) might have an unfavourable impact on renal function and blood pressure (BP) outcomes. We demonstrated in a group of 210 patients with 248 treated lesions, who underwent successful PTA procedure for RAS, that the average RS rate was 14%, accounting for 60% in inflammatory, 17% in atherosclerotic, and 0% in fibromuscular dysplasia RAS. Lack of the systolic blood pressure/diastolic blood pressure and estimated glomerular filtration rate improvement following PTA, as well as inflammatory aetiology and lower stent diameter, were associated with 4.19-, 2.93- 5.61-, and 2.76-fold risk increase of RS, respectively. Repeated PTA was effective, but recurrent RS occurred in 20% of cases.
Introduction
Percutaneous transluminal angioplasty (PTA) is a therapeutic option in patients with symptomatic renal artery stenosis (RAS) [1–3]. In fibromuscular dysplasia (FMD) this kind of treatment is the first-line therapy, whereas in atherosclerotic stenosis indications for PTA are limited to special clinical settings. The use of stents is determined by the RAS aetiology and anatomy [3, 4].
The immediate result of PTA is characterised by a high success rate and fairly low periprocedural complication rate [5–7]. However, the clinical improvement following PTA of RAS is uncertain [5–8]. The effect of PTA is probably a complex issue, as both the effect of PTA on renal function and systolic/diastolic blood pressure (SBP/DBP), as well as cardiovascular adverse events is at least controversial [6, 9, 10]. Furthermore, the long-term result of PTA is limited by the unwelcome occurrence of recurrent stenosis (RS) that may additionally impact the final effect of PTA. The RS rate following RAS procedures is estimated at 6–40% [5–8, 11]. However, the determinants of RS are poorly established.
Among the potential risk factors of RS following PTA, the RAS aetiology, the presence of previous cardiovascular disease, RAS severity exceeding 90%, bare metal stent (BMS) use, or renal artery reference calibre are mentioned [12–14]. Protective use of statins before PTA was postulated [15]. Nevertheless, data concerning the determinants of RS following PTA for RAS are rather inconsistent and poorly demonstrated.
Furthermore, the optimal treatment of RS has not been established. Potential treatment options include: balloon angioplasty with or without drug coating, cutting balloon angioplasty or deployment of a second conventional stent, repeat stenting with drug-eluting stents, or endovascular brachytherapy [16–18]. Other innovative modalities include: polytetrafluoroethylene (PTFE)-covered stents or carbon coating stents [16–18]. However, their long-term effects remain unknown.
Aim
Therefore, the aim of our study was to determine predictors of primary RS and the results of RS treatment in patients with symptomatic RAS following endovascular treatment.
Material and methods
In this prospective all-comers study, 210 patients aged 64.6 ±12.8 years (20–85) underwent 248 successful PTAs of RAS, with or without stent implantation. Thirty-nine patients underwent bilateral PTAs. We analysed freedom from the RS in index lesion.
Inclusion criteria were de novo unilateral or bilateral RAS of at least 60% with either accelerated hypertension despite three or more blood lowering medications, including at least one diuretic, drug-resistant hypertension (SBP and/or DBP values of > 140 mm Hg and/or 90 mm Hg, respectively), despite the aforementioned pharmacological treatment, and/or hypertension crisis.
Also, patients with progressive renal impairment and/or episode of acute renal failure associated with angiotensin-converting enzyme inhibitor (ACEI) treatment were included in the present study. Other inclusion criteria were pulmonary flash oedema, congestive heart failure, or severe angina/acute coronary syndrome that could not been explained by coronary artery status.
Patients with well controlled BP on blood lowering agents or renal atrophy (kidney length < 7 cm in women and < 8 cm in men), and patients not willing to participate in the study or with a follow-up period shorter than 6 months following PTA were excluded from the present study.
The prevalence of the cardiovascular risk factors was evaluated. Blood samplings for renal function assessment were collected on patient admission to the department, prior to any intervention, immediately after signed, informed consent was obtained from the patients.
Baseline and the change in levels of serum creatinine (SCC), eGFR, SBP, and DBP as well as the number of blood lowering regiments were analysed prior to PTA, at 12-month and final follow-up (F-U) visits, and whenever at the point of RS diagnosis.
The glomerular filtration rate was estimated from the Modification of Diet in Renal Disease (MDRD) formula, according to following equation: MDRD = 175 × creatinine [mg/dl] – 1.154 × age [years] – 0.203 × 0.742 [if female].
SBP and DBP measurements were performed in compliance with the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report published in 2003 and ESH/ESC Guidelines for the management of arterial hypertension published in 2013 [19, 20]. In brief, the mean SBP and DBP value was averaged from at least two BP measurements, preceded by 5 min of rest and repeated within a two-minute interval.
The study protocol was reviewed and approved by the Local Ethical Committee. All the patients gave their informed consent for participation in the study. The study was performed in accordance with the Declaration of Helsinki.
Revascularisation procedure for RAS
Renal angiography was performed from radial or femoral vascular access using a Coroscop system (Siemens AG, Munich, Germany) equipped with Quantcor version 4.0 quantitative analysis software. Angiography was performed in two modified projections that best displayed the lesion. Eligibility criteria were determined on the basis of contemporary published guidelines for percutaneous revascularisation of the RAS [1–3].
Patients were premedicated with a loading dose of aspirin of 300 mg, followed by 75 mg/day given indefinitely, and a loading dose of clopidogrel of 300 mg, followed by 75 mg/day for 1 to 6 months. During the procedure unfractionated heparin was administrated according to patient weight and ACT. Periprocedurally, routinely patients were given 1.5–2.0 l of fluids IV to prevent contrast-induced nephropathy.
The significance of RAS was determined by quantitative angiography (COROSCOP, Siemens, and Quantcor QCA V4.0 software for quantitative analysis, Erlangen, Germany). An RAS range of 50–69% of diameter of stenosis was assumed borderline, and additional invasive criteria were taken into consideration to confirm RAS significance (resting mean translesional pressure gradient > 10 mm Hg, systolic pressure gradient > 20 mm Hg, or renal fractional flow reserve induced by dopamine 50 µg/kg, rFFR ≤ 0.8).
The first-line revascularisation technique in FMD-related RAS was PTA without stenting. Atherosclerotic lesions were treated with PTA with stent implantation, and a renal protection device was used in 1 case. RAS caused by vasculitis was managed with stenting, favouring drug eluting stent (DES) implantation. DES was also preferred in patients with a single functioning kidney, small vessel diameter, and when the patient had a history of restenotic lesion in the other arterial bed.
Balloons were sized to the diameter of the reference segment of the vessel, and the patient’s symptoms were assessed during each balloon inflation.
During revascularisation procedure, predilatation vs. direct stenting technique depended on the clinical circumstances and the operator’s decision. In all cases with stent implantation, a balloon expandable stent was used. The choice of stent was conditioned by the operator’s decision, taking into account a variety of factors such as vessel anatomy, treated lesion, and stent availability. As a consequence, a heterogeneous group of stents was implanted. Procedural success was defined as residual diameter stenosis less than 30%.
RS was defined as recurrence of at least 50% reduction of the arterial lumen diameter within the stent or the adjacent 5 mm of vessel segments. When symptomatic RS was confirmed the patient was refed for repeated revascularisation.
Primary patency was defined as patency of the target lesion following endovascular intervention, and secondary patency as the final patency of the target lesion after re-intervention.
Follow-up period
The study participants were evaluated at 6 and 12 months after the procedure in the outpatient setting. Thereafter, the assessment was performed at yearly intervals. The follow-up evaluation included clinical assessment, blood pressure and renal function measurement, and duplex ultrasonography (DUS). If the patient died between month 6 and 12, the parameters from the last follow-up visit were taken into statistical analysis.
Hypertension cure was defined as BP values below 140/90 mm Hg in patients with withdrawn hypertensive medications.
During the median observation period of 48 (Q1; Q3: 23; 80) months, the incidences and predictors of RS, treatment for RS, and recurrent RS were analysed.
RS was initially diagnosed with DUS based on the peak-systolic aortic and renal artery velocities and intra-renal flow parameters [21]. The RAS was confirmed with either CT-angiography or directly during the invasive angiography preceding the PTA procedure. In some patients stenosis severity was established with translesional resting and hyperaemic gradients. Data on RS were collected during the follow-up visits.
Statistical analysis
The Student’s t-test was used for comparison of continuous variables, and a χ2 test was used to compare proportions of categorical variables. Means of the analysed parameters across groups were tested by analysis of variance test. Frequencies were compared by χ2 test for independence.
We analysed the influence of renal function and BP parameter changes, as well as patient-and procedure-related factors on the incidence of RS and recurrent RS. To ensure reliable cut-off values of BP and renal function parameter changes, which were potentially associated with risk of RS, Receiver Operating Characteristic (ROC) curves were constructed. The area under the ROC curve (AUC) was calculated as well as the 95% confidence interval (CI). The ROC analysis was followed by the uni- and multivariate Cox model.
To establish the factors that could affect RS incidence, the clinical, procedural, and angiographic variables were assessed by a Cox univariate hazard analysis, and in cases with a trend toward a difference (p < 0.15), they were included in a multivariate stepwise Cox proportional hazards analysis. The results of the multivariate Cox proportional hazards analysis were expressed as hazard ratio (HR) and 95% confidence interval (CI).
Seven-year Kaplan-Meier RS-free survival curves for primary and secondary target lesion patency, as well as RS rate depending on RAS aetiology were constructed.
Statistical analyses were performed with Statistica version 13.0 software (StatSoft, Inc., Tulsa, OK). P < 0.05 was considered statistically significant.
Results
Baseline clinical and procedural characteristics of the study participants are presented in Table I. In brief, out of 210 patients with 248 lesions referred to PTA, 225 (90.8%) lesions were diagnosed with atherosclerosis, 9 (3.6%) with fibromuscular dysplasia (FMD), 10 (4%) with vasculitis, and the remaining 4 (1.6%) with trauma-related vessel injury resulting in RAS. All FMD-related lesions underwent successful balloon angioplasty without stenting because there was no indication for stent implantation after balloon angioplasty. All arteritis-related lesions were stented, while only two atherosclerosis-related RAS underwent plain balloon angioplasty.
Table I
Baseline clinical and procedural characteristics of the study participants (n = 210)
Arterial hypertension was diagnosed in all subjects, while renal failure (eGFR < 60 ml/min/1.73 m2) was diagnosed in 125 (59.2%) patients. Unilateral PTA was performed in 139 (66.2%) patients, and bilateral or PTA of the one functioning kidney in 39 (18.6%) and 32 (15.2%) patients, respectively. The mean stenosis diameter before PTA in the whole study group was 73.6 ±15.5%, and it was reduced to 13.5 ±8.5% post PTA. In particular, the stenosis degree was reduced from 80.4 ±30% to 11.6 ±12% in arteritis-related RAS, from 73.5 ±13.9% to 13.9 ±9.3% in atherosclerotic RAS, and from 75.1 ±10 to 12 ±9% in FMD-related lesions (p = NS). DES were implanted in 25 (10.1%) and BMS in 212 (85.5%), while plain balloon alone as the ultimate method of revascularisation was performed in 11 (4.4%) lesions.
Median follow-up was 48 months (Q1, Q3: 23, 80 months). Mean SBP and DBP values after PTA, as compared to baseline values, were significantly reduced from 150.2 ±24.6 to 132.2 ±18.2 mm Hg (p < 0.001), and from 82.5 ±13.4 to 75.4 ±11.5 mm Hg (p < 0.001), respectively. Also, the number of blood lowering agents was reduced significantly from 3.5 ±1.3 to 3.2 ±1.4 (p = 0.003) (Figure 1). In line, significant mean eGFR increased from 54.5 ±23 to 59.4 ±3.9 ml/min/1.73 m2 (p = 0.001), but no SCC (p = 0.299) were observed (Figure 1).
Figure 1
Baseline vs. 12-month values for: A – systolic blood pressure (SBP), B – diastolic blood pressure (DBP), C – number of blood lowering medications, D – serum creatinine concentration (SCC), E – estimated glomerular filtration rate (eGFR) by MDR formula

During the follow-up period, RS was identified in 36 revascularized vessels, in 30 (14.4%) patients. Patients with diagnosed RS in comparison to the non-RS group were characterised by higher prevalence of hyperlipidaemia (p = 0.007) and diabetes (p = 0.07), inflammatory aetiology of revascularised lesion (p < 0.002), use of predilatation (p = 0.006), and more frequently had lower stent diameter (p = 0.001) (Table II).
Table II
Comparison of clinical, angiographic, and procedural data in patients and lesions with RS (n = 30/36) and without RS (n = 180/212)
Patients at the point of RS identification, as compared to RS-free patients, presented with lack of clinical response in terms of changes in SBP (1.4 ±17.6 vs. −15.8 ±25.8 mm Hg; p = 0.01) and DBP (2.64 ±10.1 vs. −6.5 ±14.1 mm Hg; p = 0.002) and clear noticeable deterioration of renal function: SCC (22.4 ±55.2 vs. −3.6 ±43.9 µmol/l; p = 0.002), as well as eGFR (–1.85 ±18 vs. −5.34 ±19.5 mm Hg; p = 0.045) (Table III).
Table III
Comparison of baseline and follow-up parameters of renal function and blood pressure in groups with and without restenosis
SBP decrease of less than −1 mm Hg (AUC = 0.778; 95% CI: 0.66–0.86; p < 0.001; sensitivity: 75%; specificity: 77%), DBP less than −2 mm Hg (AUC = 0.720; 95% CI: 0.63–0.81; p < 0.001; sensitivity: 77%; specificity: 63%), SCC increase of 22 µmol/l (AUC = 0.621; 95% CI: 0.51–0.72; p = 0.019), as well as no decrease of eGFR (AUC = 0.621; 95% CI: 0.51–0.72; p = 0.020), and stent diameter equal or lower than 5 mm (AUC = 0.683; 95% CI: 0.58–0.77; p = 0.002) were identified as the best cut-off values to discriminate the risk of RS by the ROC analysis. These cut-off values were analysed with univariate Cox proportional hazard analysis initially, followed by the multivariate Cox analysis (Table IV).
Table IV
Univariate and multivariate Cox proportional hazards analysis for risk of restenosis. Only parameters with p-value < 0.1 in a Cox univariate hazard analysis were included in a multivariate stepwise Cox proportional hazards analysis
In multivariate Cox regression analysis: lack of BP decrease (HR = 4.19, 95% CI: 1.67–10.3; p = 0.002), eGFR increase less than 0.17 ml/min/1.73 m2 (HR = 2.93; 95% CI: 1.08–7.91; p = 0.033), stent diameter ≤ 5 mm (HR = 2.76; 95% CI: 1.09–6.97; p = 0.031), and inflammatory aetiology of RAS (HR = 5.61; 95% CI: 1.83–17.2; p = 0.003) occurred as independent predictors of RS risk increase (Table IV).
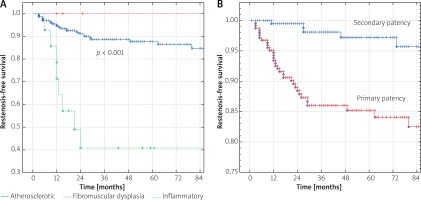
The 7-year Kaplan-Meier RS-free survival rate in the whole group was 82.5% for primary and 96.5% for secondary patency. Curves differed significantly depending on the RAS aetiology (Figure 2 A). The rates of freedom from RS at 1, 2, 3, and 7 years after PTA were 100% in FMD, while 95.6, 92, 88, and 83.9% in atherosclerosis, as well as 71.4, 39.7, 39.7, and 39.7% in vasculitis (p < 0.001).
Figure 2
Kaplan Meier curves: A – restenosis-free survival based on the RAS aetiology, B – primary and secondary renal artery patency in the whole study group
During mean follow-up, overall 28/36 (77.8%) lesions in 24/30 (80%) patients were referred for further invasive assessment. Of those, 15 focal and 13 diffused restenotic lesions were confirmed on angiography and referred for re-PTA. The remaining 6 patients with RS, after detailed evaluation of clinical and haemodynamic data, were arranged in the observational group and continuation of medical therapy.
In patients treated with rePTA the baseline vessel diameter at the point of RS was 74.6 ±16.1%, and it was reduced to 19.4 ±10% after re-intervention. Secondary success rate defined as residual diameter stenosis less than 30% was 91.7% (22 out of 24 patients).
The re-PTA intervention comprised balloon angioplasty alone in 14 lesions, drug eluting balloon in 7, bare metal stent implantation in 1, and drug eluting stent implantation in 6.
Recurrent RS was noted in 5 out of 24 (20.8%) patients/5 out of 28 (17.8%) lesions treated with index rePTA.
The Kaplan-Meier RS-free survival rates were 93.4, 85.2, and 84.1% for primary RS, and 99.5, 98.1, and 95.7% for secondary patency at 1, 3, and 5 years after PTA, respectively (Figure 2 B).
Discussion
RAS is the most common cause of secondary hypertension with incidence estimated between 1% and 5% in the general population [22, 23]. In patients with atherosclerotic lesions recognised in coronary or supra-aortic arterial beds, the prevalence of RAS is much higher, between 10–20% [24–26].
Invasive lesion management has been a treatment option for patients with malignant or resistant hypertension, hypertension crisis, or pulmonary flash oedema, when the effect of blood lowering treatment is suboptimal, and includes a variety of techniques such as percutaneous stent-assisted angioplasty or surgical reconstruction [27].
All endovascular procedures are affected by recurrent stenosis, and this main drawback of PTA of RAS has an average reported incidence rate of between 6.5% and 40% [18]. However, univocally different risk factors for RS in extra-coronary territory are postulated [28–30].
The effect of stent implantation in atherosclerotic origin RAS, compared to medical treatment alone, has a small impact on BP control, and an even weaker impact on renal function preservation in the majority of randomised clinical trials, but better results have been reported in single-centre cohort studies [5, 31].
Furthermore, the diagnosis of RS is limited by the blurred clinical picture. Firstly, the impact of PTA on BP and renal function is unpredictable and diversified; secondly, there are no pathognomonic symptoms indicative of RS; and finally, the effect of RS on clinical parameters is poorly investigated. The novelty of our present study was the identification of potential links between the change in BP and renal parameters and the incidence of RS. Our major finding is that the lack of significant decrease in either SBP (less than −1 mm Hg drop) and DBP (less than −2 mm Hg drop) at 6-12 months following successful procedure was independently related to a 4.15-fold RS risk increase, while lack of renal function improvement (eGFR increase of less than 0.17 ml/min/1.73 m2) was associated with 2.93-fold risk of stenosis recurrence in multivariate Cox proportional hazard analysis.
In line, Zeller et al., in a group of 447 patients who underwent 619 renal artery interventions, found an RS rate of 19% at 5 years [32]. Of these RS, 81% were associated with recurrent symptoms: recurrent hypertension in 84%, or continuing deterioration in renal function in 16%. Also, Lederman et al. observed that RS tended to be more common among patients who had renal functional deterioration or lack of BP decrease after the PTA [13].
The index vessel diameter – another predictor of RS identified in our present study – was also reported by other authors [13, 14, 33, 34]. While stent diameter cut-off values related to RS risk differ between the studies, the general rule was that smaller vessels have a higher RS rate, e.g. in the Lederman study, the RS rate was 36.0% for vessels with a reference diameter < 4.5 mm, compared with 15.8% in vessels with reference diameter 4.5 to 6.0 mm, and 6.5% in vessels with reference diameter exceeding 6.0 mm (p < 0.001) [13].
Consistently, Vignali et al. and Djavidani et al. reported a lower rate of RS in patients with stent diameter of 6 mm or more, compared with smaller diameters [14, 34]. Vessel size is also reflected by lower patency rates. In small-diameter renal arteries (< 3.5 mm) treated with DES in patients with atherosclerotic renal artery stenosis, the 1-, 2-, and 5-year patency rates were 71%, 63%, and 38%, respectively [35].
The RAS disease has heterogeneous aetiology, hence both the clinical and survival outcomes differ with respect to whether arteritis, FMD, or atherosclerosis is its background [36, 37].
Iwashima et al. paid attention to differences between RS risk factors depending on the RAS aetiology. In atherosclerotic lesions, independent predictors of RS were initial degree of RAS > 90% (HR = 3.95; 95% CI: 1.14–24.95) as well as the presence of cardiovascular disease (2.84; 95% CI: 1.16–8.51) [11]. While FMD was associated with RS risk itself (HR = 2.65; 95% CI: 1.10–5.95), of note the stenting rate in FMD patients was 34% in this study [11].
In our present study, the seven-year Kaplan-Meier RS-free survival curves differed significantly depending on the RAS aetiology. The rates of vessel patency at 1, 2, 3, and 7 years after PTA were 100% in FMD, while 95.6, 92, 88, and 83.9% in atherosclerosis, as well as 71.4, 39.7, 39.7, and 39.7% in vasculitis (p < 0.001).
It is well known that balloon angioplasty without stenting is sufficient in the majority FMD cases with high patency rates and cure of hypertension in the majority of patients [37]. In general, acute effect and long-term durability after PTA for FMD-related lesions are good in most treated patients, especially in the case of lesions characterised by a “string of beads” appearance limited to the main artery. In such cases redo procedures are needed in 6–34% of treated patients [11, 37, 38].
In our study group all FMD-related lesions were eligible for revascularisation limited to balloon angioplasty alone without the need of stent implantation. However, it should be emphasised that our good results regarding acute and long-term patency of treated FMD-related lesions may as well reflect serendipity conditioned by no need of stenting and the small group of treated lesions. Indeed, these results should not be generalised and taken for granted because a 100% RS-free rate after FMD revascularisation has not been reported.
The study by Park et al. concerning long-term outcome of endovascular treatment of RAS related to Takayasu arteritis demonstrated better long-term patency and similar clinical benefit on renovascular hypertension for balloon angioplasty compared with stent placement and concluded that in this kind of RAS aetiology stent placement should be reserved for obvious angioplasty failure [36]. Furthermore, our study, with stenting in the majority of cases, indicated fast loss (60% in 2 years) of the vessel patency in vasculitis when a stent was implanted.
In atherosclerotic RAS the other potential risk factor of RS, supported by some researchers, but not in our study, is the stent type. Published data concerning the impact of BMS and DES on restenosis prevention resulted in conflicting conclusions, favouring DES implantation in two out of three publish studies. Hence, in patients with small renal arteries the use of DES seems reasonable [12, 39, 40].
In the study by Corriere et al. decreased risk of RS was associated with preoperative statin use (HR = 0.35; 95% CI: 0.16–0.74; p = 0.006) and increased preoperative DBP (HR = 0.70 per 10 mm Hg increase in preoperative DBP; 95% CI: 0.49–0.99; p = 0.049) [15]. However, statins were not confirmed in the study by Jundt et al., who reported history of stroke to be an independent risk factor of RS in patients with RAS and renal impairment at baseline [35].
In our study, patients with RS treated with repeated angioplasty showed recurrence in 20% of cases. This is in line with results of Stone et al. and Zeller et al. [16, 32].
Our patients were innumerous and were managed by different techniques, thus complex analysis is not possible. The data from Zeller et al. indicated that re-occurrence of RS was more likely in smaller vessel diameters with an incidence of 57% in 3-4 mm; 42% in 5 mm; 20% in 6 mm, and 14% in 7 mm vessel diameters [32]. Nevertheless, repeated endovascular treatment of RS is possible and effective.
Conclusions
The average RS rate was 14%, accounting for 60% in inflammatory, 17% in atherosclerotic, and 0% in FMD RAS at 24 months following PTA. Lack of the SBP/DBP and eGFR improvement following PTA, as well as inflammatory aetiology and lower stent diameter are independently associated with increased risk of RS. Repeated PTA is effective, but recurrent RS occurs in 20% of cases.








