Introduction
Atherosclerosis, underlying coronary artery disease (CAD), is best characterized as a low-grade inflammatory condition, where cholesterol particles – mostly oxidized low-density lipoproteins (ox-LDL) – infiltrating the vessel wall act as an antigen and initiate an inflammatory response [1]. This approach has been explored for many years now but does not allow for a full understanding of the disease. Recently, the actin cytoskeleton and associated regulatory proteins have been gaining attention as contributors to the pathophysiology of CAD [2]. Among these, profilin 1 (Pfn1) is an emerging player in the field [3, 4]. Research showed that Pfn1 was overexpressed in atherosclerotic lesions in comparison to the healthy vessel wall [5]. In mice a deletion of one copy of the PFN1 gene increased the production of nitric oxide, lowered the expression of adhesion molecules and hindered macrophage infiltration, thereby protecting against atherosclerosis [6]. In diabetic atherosclerosis models, Pfn1 was overexpressed in endothelial cells exposed to advanced glycation end-products, accompanied by hallmarks of endothelial dysfunction [7]. Pfn1 was also implicated in the pathophysiology of acute coronary syndromes. It was found within thrombi retrieved from culprit arteries and correlated with symptom duration, as well as final Thrombolysis in Myocardial Infarction flow [8, 9].
So far there has been very little research on Pfn1 in humans, and it has never been assessed in relation to atherosclerosis risk factors or the severity of atherosclerosis estimated by coronary angiography.
Aim
To assess serum concentrations of Pfn1 in relation to risk factors and extent of coronary artery disease.
Material and methods
The study was approved by the institutional ethical board (decision no. 122.6120.270.2015; 17th December 2015) and was conducted in accordance with the principles listed in the 1964 Declaration of Helsinki. We enrolled consecutive patients with CAD qualified for coronary angiography, who presented with chronic coronary syndrome (CCS) or myocardial infarction (MI). Exclusion criteria were as follows: an MI other than type 1, an MI with symptom duration of more than 24 h, prior coronary artery bypass grafting, active inflammation, thrombosis in vessels other than coronary arteries, an active neoplasm (diagnosed and/or treated within the last year), a stroke (ischemic or hemorrhagic) within 3 months prior to admission, known pro-thrombotic conditions, chronic anticoagulation, and estimated glomerular filtration rate < 30 ml/min/1.73 m2.
We checked patients for the presence of typical atherosclerosis risk factors and co-existing conditions. Hypertension was defined as a blood pressure ≥ 140/90 mm Hg measured on two separate occasions, a history of hypertension or chronic use of antihypertensive drugs. Hypercholesterolemia was defined as total cholesterol of more than 5.0 mmol/l and/or low-density lipoprotein (LDL)-cholesterol of more than 3.0 mmol/l, or in patients with lipid-lowering pharmacotherapy. Diabetes mellitus was coded when the patient had a prior diagnosis or if glycemia and/or glycated hemoglobin (HbA1c) concentrations met the definitions included in the appropriate guidelines [10]. Active smoking was defined as smoking 10 or more cigarettes/day within the last 6 months prior to admission. Obesity was coded when a patient’s body mass index was 30 kg/m2 or above. A family history of CAD was coded when a family member in the first degree (parents, siblings, children) experienced myocardial revascularization, MI and/or cardiovascular death before the age of 55 for men and 65 for women.
Multivessel disease was defined as significant stenosis (≥ 50% for left main and 70% for other vessels) of three or more epicardial coronary arteries with a diameter of at least 2 mm [11].
The severity of coronary atherosclerosis was also assessed using the Gensini Score [12]. Even though it is widely used in clinical practice, we did not assess the SYNTAX score, as it is a measure of lesion complexity more than an indicator of atherosclerotic burden. We analyzed whether the patient had experienced an acute coronary syndrome or percutaneous coronary angioplasty in the past. Moreover, we searched for correlations between plasma Pfn1 and standard laboratory parameters.
Profilin 1 concentration measurement
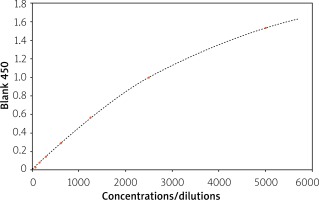
A 2.6 ml sample of venous blood was collected into an EDTA-coated tube from each patient on admission, prior to the procedure. The samples were centrifuged at 1600 g for 10 min. The supernatant was collected and stored at –80°C, until further use. Pfn1 concentration was determined using the enzyme-linked immunosorbent assay (ELISA). We used the human profilin 1 SEC233Hu ELISA kit (Cloud-Clone Corp., Houston, USA) with a detection range of 78–5000 pg/ml. This is a test employing the biotin-avidin-horseradish peroxidase system. 100 μl of undiluted serum sample was inserted per well. The spectrophotometric reading was performed at 450 nm, immediately after using the stop solution. A calibration curve was prepared by measuring the absorbance at the same wavelength using serial dilutions of a given standard [13]. The calibration curve is shown in Figure 1.
Statistical analysis
Continuous variables were checked for normal distribution by the Shapiro-Wilk test. Pfn1 concentrations were compared using the Mann-Whitney test and presented as median and 25–75% interquartile range (IQR), as the data did not fulfil the assumption of normality of distribution. The Spearman correlation test was used to compare two numerical variables. The level of significance was assumed at α = 0.05.
Results
We included a hundred patients with CAD admitted for coronary angiography: 65 with MI and 35 with CCS. There was no difference in serum Pfn1 levels between patients with MI and CCS. We found that median Pfn1 concentrations were significantly lower in patients with diabetes (p = 0.008), family history of CAD (p = 0.043) and multivessel disease (p = 0.018). We did not find a correlation between Pfn1 concentration and Gensini score (rho = 0.086; p = 0.779). For the association between Pfn1 and LDL we obtained values of rho = 0.198, p = 0.056; and for Pfn1 and C-reactive protein (CRP), rho = 0.309, p = 0.076. The results are shown in Tables I and II.
Table I
Profilin 1 serum concentrations with regard to known atherosclerosis risk factors and severity of coronary artery disease
Table II
Spearman’s correlations between serum profilin 1 concentrations and standard laboratory results
Discussion
This is the first study showing that in patients with symptomatic CAD, serum Pfn1 levels are lower in patients with diabetes, family history of CAD and multivessel disease.
Pfn1 and diabetes
Previous studies using animal and in vitro models suggested detrimental effects of Pfn1 in diabetes-associated atherosclerosis. Li et al. found that exposing human endothelial cells to advanced glycation end-products led to an increase in Pfn1 expression and cytoskeletal rearrangement. This was accompanied by a decrease in nitric oxide release, as well as a rise in intercellular adhesion molecule 1 and asymmetric dimethylarginine [7]. Pfn1 expression was higher in aortic endothelial cells of diabetic rats, compared with specimens without diabetes. Inducing Pfn1 expression in these cells led to a rise in intercellular adhesion molecule 1 expression, as well as apoptosis. Importantly, endothelial cells treated with LDL and ox-LDL showed higher Pfn1 expression [14].
Our results seem to be counterintuitive in the context of the above. This may be due to the fact that serum Pfn1 does not have to reflect its intracellular levels. Another explanation could be that serum Pfn1 may undergo carbonylation, which is a common mechanism of posttranslational modifications under persistent hyperglycemia [15]. Carbonylation is known to alter protein structure and function [16]. This could lead to weaker binding with the ELISA antibody and lower detection. To confirm this, a larger study is needed focusing on Pfn1 structure under chronic hyperglycemia as well as on markers of glycemia control and duration of the disease.
Pfn1 and family history of CAD
We found a lower Pfn1 concentration in patients with a family history of CAD. Although we assessed the protein and not the gene itself, it cannot be ruled out that genetic variants of the PFN1 gene leading to structural and functional changes are relevant in CAD. Lower ELISA readings could be a result of three phenomena: instability of a mutant protein, a tendency to form aggregates or a conformational change leading to a weaker interaction with the antibody employed in the test. In fact, Pfn1 mutations have been reported in other human diseases, foremostly in amyotrophic lateral sclerosis [17]. The best characterized mutations include C71G, M114T, G118V and E117G. All of these mutants have an altered tertiary structure and easily form aggregates (with the C71G being the most prone to aggregation) [18], while M114T causes conformational changes to the core of the protein, impairing its stability [19]. Taking into account that this is a preliminary result, it may be reasonable to search for an association between genetic variants of the PFN-1 gene and cardiovascular outcomes.
Severity of CAD
The relationship between Pfn1 concentration and the extent of coronary lesions is unclear. We found no association with a history of MI or percutaneous coronary intervention (PCI). We found that patients with multivessel disease had lower serum profilin, but we did not confirm this result using the Gensini method. This result requires further studies.
Basic laboratory results
Although there were non-significant associations between Pfn1 and LDL (p = 0.056) and CRP (p = 0.076), these results require further evaluation in a larger group of patients.
Study limitations
The small sample size and data overlap between the compared groups does not allow us to draw clinically applicable conclusions at this point. Also, due to the fact that we analyzed coronary angiograms, we did not include healthy volunteers as a control group, which might have been a valuable addition when analyzing the role of variables such as diabetes or family history of CAD. This is to be considered in future studies on the subject.
Conclusions
Although preliminary, this is the largest study conducted so far on Pfn1 in CAD in humans. Lower levels of serum Pfn1 in diabetes and associations with family history of CAD and multivessel disease were shown for the first time and may suggest different regulation of its release from cells in these conditions or, possibly, a change of structure (due to a genetic mutation or post-translational modification). The role of the cytoskeleton and associated proteins is a potential new direction in the studies on atherosclerosis.