A 49-year-old female patient on chronic dialysis for the last 13 years was referred for a dysfunctional left side-to-side Brescia-Cimino fistula created in another institution, 14 years previously. She had a history of nephrectomy after a severe traumatic injury at the age of 16. Her medication included clopidogrel 75 mg o.d., omeprazole 20 mg o.d. and sevelamer carbonate 800 mg, 2 tbs t.i.d. The efferent cephalic vein was thrombosed, and cannulation was impossible via a serpentine and kinked basilic vein in the forearm. Hemodialysis was performed by a permanent tunneled catheter placed in the right jugular vein. After a color duplex ultrasound evaluation, forearm cephalic vein thrombosis was confirmed, but the fistula functioned via the patent afferent wrist cephalic vein. This vein was draining in the forearm basilic vein, through a dilated venous network at the dorsal aspect of the hand. The flow volume was 700 ml/min. Deep veins were patent. This anatomic venous configuration resembles the venous outflow of an ulnar-basilic vein (Figure 1). Preoperative percutaneous digital subtraction venography revealed normal patency of the upper arm cephalic, basilic, and central veins.
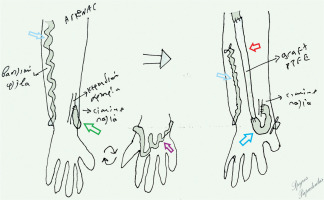
Figure 1
The distal venous part of the radiocephalic fistula (green arrow) drains to a dilated and kinked basilic vein (blue arrows) through a venous network at the dorsal aspect of the hand
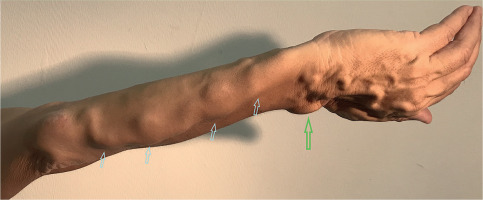
The patient underwent interposition of a synthetic 4–7 mm graft (Intering, W.L Gore & associates, Arizona) in the forearm. The afferent cephalic vein was axially transected and the distal part was ligated. The proximal part was anastomosed end-to-end with the straight tube graft after cranial reversal of the vein, as it had a caudal direction. The graft was subcutaneously tunneled in the forearm and the proximal part was anastomosed end-to-end with the basilic vein at the elbow level after division of the vein. The distal part of the basilic vein was ligated (Figures 2 and 3). Postoperatively, the dilated forearm basilic vein and the dorsal venous network were regressed. The basilic vein was kinked and partially stenotic, so it could not be used. Had this not been the case, the basilic vein could have been prepared at the medial aspect of the forehand and, after distal division, placed along the same route as the synthetic graft. The fistula has remained patent and functional since the operation (for the last 5 months) (Figure 4).
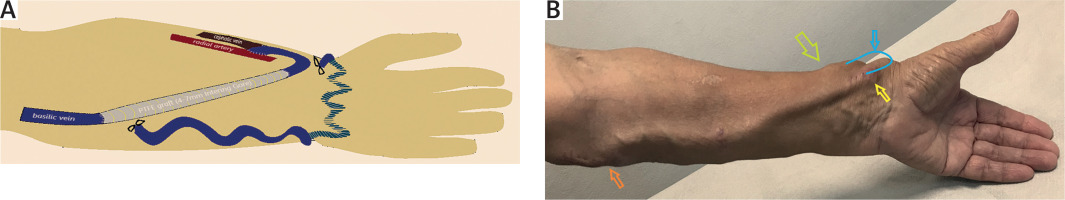
Figure 3
A – Graphic representation of the operative outcome. B – The patient at 6-week follow-up (green arrow: radiocephalic anastomosis, blue arrow: the distal venous part was reversed and anastomosed with the graft (yellow arrow), orange arrow: proximal anastomosis)
Higher flow rates, increased vein dilatation, and functional maturation were achieved with end-to-side radio-cephalic fistulas compared to side-to-side anastomoses in some reports [1, 2]. Other reports have not shown the superiority of one method over the other in terms of patency and functional maturation [3–6]. However, some authors found that the side-to-side configuration in radiocephalic fistulas may be complicated with palmar and digital venous hypertension in up to 5–10% [7–9]. Thus, in cases of side-to-side radial-cephalic fistula construction, due to the surgeon’s preference for technical facilitation, distal cephalic ligation is usually performed after completion of the anastomosis [7, 10, 11]. European Society for Vascular Surgery (ESVS) guidelines do not comment on or advise a specific choice between the two techniques [12]. This venous configuration as described in our patient is highly uncommon. The most surprising finding was the lack of concomitant venous hypertension in the fingers. We were not able to find a similar case after a thorough search in the literature. Thus, we cannot provide alternative reconstruction procedures reported in such a patient in the literature. On the other hand, interposition grafting to treat arteriovenous fistula complications such as venous aneurysms or stenoses are common practice in access surgery [13–15].
In conclusion, although the side-to-side configuration without distal ligation in radiocephalic fistulas is not a preferred method in our institution, the presence of the distal venous part in our patient kept the fistula patent after thrombosis of the proximal cephalic vein. This gave an option for a salvage procedure in this Brescia-Cimino fistula with an exceptional outflow to the basilic vein.