Dear Editor,
Sudden and massive arterial bleeding caused by the occurrence of tracheo-innominate artery fistula (TIF) in severely ill patients such as those with acute respiratory distress syndrome (ARDS), although rare (reported incidence 0.1-1%) [1], is always challenging and most commonly results in a lethal outcome. The reported survival rate after massive bleeding from TIF is 14.3% [2]. However, such a complex case may be even more complicated if the scenario occurs in an improvised COVID-19 intensive care unit (ICU), which significantly aggravates the situation and lessens the chances for survival. Hence, we report here our experience of a case of massive arterial bleeding from the TIF in a young male patient with COVID-19-caused severe ARDS and veno-venous extracorporeal membrane oxygenation (VV ECMO). Moreover, we discuss the problems that endanger patient outcomes and highlight the importance of rapid decision-making in a multidisciplinary team even in the difficult environment of improvised ICUs during the COVID-19 pandemic.
A 37-year-old man with COVID-19 illness and severe ARDS was referred to our centre from the local hospital 20 days after the first symptoms of the disease, owing to the failing mechanical ventilation and the need for VV ECMO. His past medical history is notable for acute lymphoblastic leukaemia in remission for the past 8 years.
Upon arrival at our centre, the patient was immediately placed on VV ECMO (with cannulas in the right femoral and internal jugular vein). Anticoagulation was achieved with continuous unfractionated heparin guided by APTT. The persistent severe form of ARDS and the need for prolonged mechanical ventilation prompted the introduction of technically uncomplicated percutaneous tracheostomy six days later. Percutaneous tracheostomy was performed using the Seldinger technique and the Smiths Medical Portex Percutaneous Tracheostomy Kit. To ensure proper placement of the tracheal cannula, the tracheostomy was performed under direct visual guidance using an Ambu aScope 4 Broncho bronchoscope. The puncture site of the trachea was between the 2nd and 3rd tracheal cartilage. A size 9 tracheal cannula was placed and fixed with four stitches to prevent dislocation.
Five days after the placement of the tracheal cannula, excessive bleeding around the insertion place was observed. The consultant ENT specialist found a completely obstructed tracheal cannula and deflated the cuff, aiming to replace the cannula. This manoeuvre resulted in dramatic arterial bleeding from all upper respiratory tract openings. The bleeding was temporarily stopped by digital compression. The massive bleeding transfusion protocol was initiated, gene-ral anaesthesia was induced, but gas exchange was performed exclusively by ECMO. At the same time, the surgical team started emergency bleeding exploration in the ICU (Figure 1). The patient was found to have communication between the innominate artery and the trachea which opened upon deflating the cuff of the tracheal cannula. Salvage surgery included reconstruction of the innominate artery with a Dacron graft (Figure 2). During the 5-hour procedure, the patient received massive volume resuscitation, guided by the clinical condition and point-of-care testing, including 21 litres of crystalloids, 6 litres of colloids, 23 doses of erythrocyte concentrates, 7 doses of fresh frozen plasma, 8 doses of platelets and 7 g of fibrinogen. The patient maintained continuous urine output, whereas ECMO flow was stable and with satisfactory venous oxygen saturation resulting in the highest lactate level of 3.5 mmol L–1.
FIGURE 1
The surgical intervention was performed in an improvised intensive care unit with inadequate equipment. The cardiac surgeon (1) is working without surgical loupes, with protective glasses only and under a small source of light (2). The ventilator is turned off (3), and the gas exchange was performed via VV ECMO only

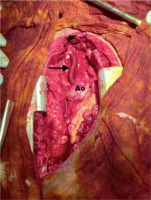
FIGURE 2
The damaged part of the innominate artery was resected, and the anastomosis of the innominate artery and ascending aorta (Ao) was performed with a Dacron graft (blackarrow). The surgical field was cleaned with povidone-iodine
After the procedure, the patient’s neurological status remained preserved. However, the tracheal defect was established as irreparable; therefore the defect was bridged with a new endotracheal tube to maintain ventilation. Owing to the prolonged in-hospital stay and many indwelling catheters and cannulas present, the patient developed severe sepsis caused by several nosocomial pathogens including fungi. However, despite undertaking all available measurements, the patient’s respiratory function was severely and irreversibly damaged, and in the condition of severe sepsis, the patient died after 108 days of ECMO support.
TIF communication is a rare but ominous condition which occurs as a consequence of erosion of the tracheal wall by the tracheostomy cannula tip and pulsatile contact with the innominate artery adjacent to the erosion site [3]. Massive arterial bleeding caused by the appearance of TIF, if it occurs in a non-operating-room (non-OR) environment, is very difficult to treat resulting in survival. The survival rate among patients who are brought to the OR is approximately 25% [1]. Furthermore, patients undergoing emergent surgical management of TIF are at increased risk of neurological and even multiorgan damage in cases of significant blood loss, possible persistent hypotension, hypoxia and challenging and therefore prolonged surgical intervention on the innominate artery.
Our case demonstrated that this catastrophic scenario can be successfully managed even in suboptimal conditions. Although challenging in a medical and technical way, this case clearly highlights the utmost importance of multidisciplinary communication and rapid organization in similar cases, especially in the setting of an improvised ICU during the COVID-19 pandemic.
The problems that impeded the management of complex cases in the COVID-19 pandemic were numerous. Firstly, an enormous number of patients requiring intensive care overwhelmed the hospitals, which prompted the reorganization of hospital resources [4, 5]. This resulted in improvised COVID-19 ICUs, with suboptimal equipment [4, 6]. Secondly, owing to the scarcity of adequately educated ICU personnel, many medical professionals were redistributed from their departments to COVID-19 ICUs, as well [5]. Thirdly, notwithstanding the redeployment of medical staff, increased workload, tiredness and exhaustion were important factors in the everyday life of healthcare professionals during the pandemic, additionally reducing their work capacity and endangering their decision-making [4, 6]. Fourthly, the protective equipment required in COVID-19 units in a certain amount impairs communication, diminishing an individual’s ability to react adequately in emergency situations, which might be fatal if a misunderstanding happens [7, 8]. Although our patient was in the improvised setting of a COVID-19 ICU, the prompt response of intensive care nurses, intensive care specialists, anaesthesiologists, cardiothoracic surgeons and other medical specialists who were redistributed to work in the COVID-19 ICU resulted in the successful management of life-threatening massive arterial bleeding from the TIF.
Considering the acquired experience of COVID-19 illness and its complications during the pandemic, the entire medical community and healthcare systems should raise awareness of the paramount importance of interdisciplinary communication and rapid problem-solving, particularly in managing such a vulnerable population of most severely ill ICU patients.
Besides interdisciplinary communication among specialists in a hospital, it is worth emphasizing the value of a well-established network between local hospitals and expert centres to provide the best care for patients in a timely manner.
Reporting on the management of complex cases in challenging environments of improvised ICUs during the COVID-19 pandemic is essential to emphasize the role of the deliberation of such cases in a multidisciplinary team and to accentuate the importance of prompt and clear communication for positive outcomes.




