Introduction
We report a case that, to our knowledge, is the first report of membranous dysmenorrhoea (MD) during assisted reproductive technology. Membranous dysmenorrhoea is an uncommon clinical condition characterized by the spontaneous sloughing of endometrium in one piece retaining the shape of the uterus. The most common symptom of MD is a colic type of abdominal pain because of uterine contractions and because of the passage of the tissue through the non-dilated cervix. Only a limited number of cases have been published in the literature. Various hypotheses have been described regarding the MD pathophysiology. For example, endometrial infections, integrin abnormalities, and high levels of progesterone have been considered as causative agents [1]. Increased progesterone levels, due to endogenous or exogenous causes, may cause thickening of the endometrium, first with dilatation of spiral arteries and then vasoconstriction and incomplete desegregation of endometrium, which acts as a foreign body and as a trigger for uterine contractility with the consequent tissue discharge [1]. In this regard, progesterone is an essential hormone for embryo implantation and maintenance of the pregnancy, and its supplementation is necessary in women undergoing artificial frozen embryo transfer (FET) cycles because of the absence of corpus luteum [2], so the exogenous administration of progesterone may be a predisposing factor for the development of MD.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from each participant included in the study.
Case report
This report describes a case of a patient who first underwent an artificial FET cycle using vaginal progesterone with subsequent MD, and then a successful artificial FET cycle using subcutaneous progesterone. Our report follows the Consensus-based Clinical Case Reporting Guideline Development, validated by the Enhancing the QUAlity and Transparency of Health Research Network. The patient signed informed consent for the procedure she underwent, to allow data collection for research purposes and the publication of this case report. Considering the anonymized data collection and description of the case, formal approval by the Institutional Review Board was exempted.
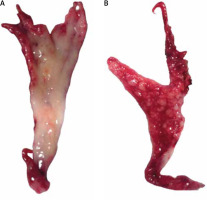
A 35-year-old nulligravid Caucasian woman with a history of infertility due to partner’s oligoasthenospermia underwent her first IVF cycle with a non-elective freeze-all strategy to avoid the risk of ovarian hyperstimulation syndrome. The patient had never received previous progesterone-based therapies. She then underwent an artificial FET cycle with oral administration of oestradiol valerate, 6 mg/day, and the subsequent administration of vaginal progesterone administration, 200 mg, 3 times a day. The patient underwent an ultrasound-guided embryo transfer (ET), and she continued the therapy until the pregnancy test. Sixteen days after ET the patient started her menstrual period with an intense colic abdominal pain, and she noticed the discharge of a gross whitish membranous tissue from her vagina (Fig. 1). The histological examination of the tissue reported endometrial mucosa with a decidual modification of the stroma and glands. After this event, the patient underwent another FET artificial cycle with oral administration of oestradiol valerate, 6 mg/day, and subsequent subcutaneous progesterone administration, 25 mg, once a day for 3 days, then twice. The patient underwent another ultrasound-guided ET, and the pregnancy test result was positive. The patient continued the ongoing therapy during the first trimester, and she delivered a healthy baby at term after an uneventful pregnancy.
Discussion
Membranous dysmenorrhoea should be considered because the approach to provide an appropriate endometrial preparation for FET is still a matter of debate. Vaginal preparations have been demonstrated to be better tolerated than injective drugs [3], although there are no data on clear superiority of either vaginal or injective progesterone preparations in artificial FET cycles [4]. Of note, hormonal pharmacokinetics change with the different route of administration: levels of progesterone are very high in endometrial tissue when using vaginal progesterone administration; conversely, the highest serum levels are achieved using IM administration [5]. A subcutaneous route of administration of progesterone is available, and its non-inferiority compared with the vaginal preparations in artificial cycles has already been demonstrated [6]. For this reason, the progesterone route of administration should be addressed and considered in all reproductive treatments, for its key role in IVF outcomes [7].
The role of progesterone supplementation in IVF cycles seems important for membranous dysmenorrhoea cases. Although MD is also known as ‘the disease of theories’ because the aetiology is still unknown, some cases of decidual cast expulsion have been observed following high levels of progesterone. Hyperprogesteronism seems to play an important role in the aetiopathogenesis of MD [1, 8]. Increased progesterone levels, due to endogenous or exogenous causes, may cause thickening of the endometrium, first with dilatation of spiral arteries and then vasoconstriction [8, 9]. This may cause the incomplete desegregation of endometrium, which acts as a foreign body and as a trigger for uterine contractility with the consequent tissue discharge. The role of infections has been also hypothesized by some authors due to the presence of micro-abscesses in discharged tissue [10]. In our case we hypothesized that exogenous progesterone played a role in the development of this condition because a different protocol for progesterone administration was shown to be useful in preventing MD recurrence. A comparison of serum progesterone levels would not have been useful because of hormones pharmacokinetic chances with the different route of administration and serum progesterone levels do not match with endometrial progesterone levels [4]. Taken together these insights, in reproductive medicine the main role of such peculiar case reports consists in helping the IVF consultants to reach the optimal progesterone supplementation, considering the endometrial impact.
Conclusions
In our case report, the vaginal progesterone administrated in the first treatment may have caused hormone levels in the tissue to be too high. Our patient was probably predisposed to develop MD, and the subcutaneous route of progesterone administration has been able to guarantee satisfactory progesterone levels to ensure pregnancy and to avoid the development of MD. Our report seems to support the role of progesterone in the pathogenesis of MD, but more studies are needed to clarify the aetiology and the pathophysiology of this pathologic condition.