Cardiac surgery for ascending aorta diseases is possible via a full median sternotomy (FMS), partial sternotomy, or – nowadays increasingly often – a right anterior mini-thoracotomy (RAMT). RAMT causes less trauma for patients and, by sparing the sternum, facilitates quicker recovery. The thoracotomy approach is well described for minimally invasive aortic valve and mitral valve surgery [1]. Given the satisfactory outcomes, cardiac surgeons have been expanding the portfolio of RAMT surgery, performing more demanding procedures through this approach. Herein, we report outcomes of 3 patients who underwent minimally invasive ascending aorta replacement isolated or combined with aortic valve replacement (AVR).
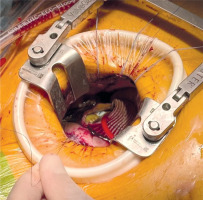
A 49-year-old male patient underwent ascending aorta replacement for ascending aorta aneurysm (AAAsc) in May 2024 (Figure 1). He presented to our department with exertional dyspnea (NYHA class II functional status) and chest pain (CCS class II functional status) and had a history of hypertension and dyslipidemia. Surgery was performed with cardiopulmonary bypass (CPB) and femoral cannulation. CPB time and cross-clamp (XC) time were 129 and 81 minutes, respectively. The ascending aorta was replaced with a 30 mm woven vascular graft in the supracoronary position with the distal anastomosis 2 cm below the origin of the brachiocephalic trunk. The patient was extubated 2 hours after surgery, and his post-operative course was uncomplicated. The patient was discharged home on postoperative day 6.
Approximately 1 month after the initial discharge from hospital, the patient was readmitted to our ward due to improper wound healing. The issue was managed with negative-pressure wound therapy (NPWT) for 10 days and wide-spectrum antibiotics. After reassessing the wound, it was closed again with no further complications. Six months later, the patient attended a follow-up in our outpatient clinic, and the wound had healed properly.
A 69-year-old male patient underwent ascending aorta and non-coronary sinus replacement for aneurysm of ascending aorta and aortic sinus, and AVR for aortic insufficiency in September 2024. His native aortic valve was bicuspid, defined as type I according to the Sievers classification. He presented to our department with exertional dyspnea (NYHA class II functional status) and had a history of hypertension, dyslipidemia, and COPD. Surgery was performed with CPB and femoral cannulation. CPB time and XC time were 242 and 198 minutes, respectively. The aortic valve was replaced, along with the non-coronary sinus and ascending aorta. The patient required reoperation due to bleeding, with a right anterior thoracotomy (RAT) approach. His post-operative period was difficult, necessitating transfusion of 5 units of packed red blood cells (pRBC) in the ICU. It was possible to extubate him after 28 hours upon arrival at the ICU, and a new onset of atrial fibrillation occurred on ward. The patient was discharged home on postoperative day 7. At the follow-up visit 2 months after initial discharge, the patient was feeling well, the wounds were healing properly, and no complications had occurred.
A 66-year-old male patient underwent ascending aorta replacement for AAAsc and AVR for aortic insufficiency in November 2024. His native aortic valve was bicuspid, defined as type I according to the Sievers classification – left and right coronary cusps were fused and heavily diseased. He presented to our department with exertional dyspnea (NYHA class II functional status) and had a history of hypertension, dyslipidemia, and heart failure. Surgery was performed with CPB and femoral cannulation. CPB time and XC time were 165 and 141 minutes, respectively. The aortic valve was replaced, and an aortic prosthesis was implanted in the supracoronary position. It was possible to extubate the patient early, 3 hours after arrival at the ICU. The patient required transfusion of 2 units of blood on ward. No other complications developed. The patient was discharged home on postoperative day 6. At the follow-up visit, 3 months after discharge, the patient was feeling well, without dyspnea or any other complaints. The wound had healed properly.
RAMT may be a suitable approach for ascending aorta replacement in patients with AAAsc (Figure 2). As is well known in patients undergoing mitral valve or aortic valve surgery, such a minimally invasive approach is associated with less blood transfusion, quicker recovery, and shorter hospital stay [2, 3]. Rayner et al. reported in a meta-analysis comparing FMS to minimally invasive approaches, including RAMT, that more pRBC units were transfused in patients undergoing surgery via FMS. This paper also reports that patients in the MICS group spent less time in the ICU, and their overall length of stay was also shorter [4]. Notably, Lim et al. concluded that 5-year survival after AVR was significantly higher in the RAMT group than in patients who underwent partial sternotomy [3].
Research by Durdu et al. confirmed that the abovementioned variables have the exact same output in patients undergoing ascending aorta surgery [5]. In our experience, only 1 patient’s post-operative course was complicated, yet it is difficult to assess whether it was due to the approach or combining two procedures in one surgery, along with extended CPB and XC time. Another factor that prolonged surgery was replacing the non-coronary sinus, instead of performing the Bentall procedure – a decision made with great difficulty. The incidence of re-exploration for bleeding in patients being operated on via RAMT may not differ from patients undergoing FMS [6]. Despite these difficulties, it was possible to discharge this patient just 7 days after the procedure.
In contrast to other patients, who were discharged after 6 days, this proves that even when the postoperative period is complicated, the minimally invasive approach facilitates quicker recovery. Gilmanov et al. compared octogenarians undergoing AVR through RAMT and FMS, and their research showed that half of the patients in the RAMT group were discharged after 6 days, while in the FMS group it was only one-third of patients [6]. At the time of discharge, all our patients were in a good clinical condition.
Only 1 patient needed rehospitalization, due to superficial improper wound healing after RAMT. However, this complication should not be associated with the type of procedure performed through such an approach; thus, it should not affect our statement that replacement of the ascending aorta with minimally invasive techniques is still feasible and, in some situations, even preferable. Durdu et al. noted that wound infections occurred less frequently in the RAMT group than in patients undergoing full sternotomy, and when they did occur, their negative impact on the patients were much less severe [5].
Our second patient was operated on through the RAMT approach due to COPD with a low FEV1 value, measured at 1.2 l. It was our objective to avoid sternotomy in this patient. The postoperative bleeding which occurred could have been due to dense pleural adhesions that were encountered upon entering the pleura – these being very commonly observed in COPD patients who have multiple exacerbations and infections. Stolinski et al. stated in their paper that RAMT surgery could be a better choice for patients suffering from pulmonary disease, such as COPD. Their patients who underwent AVR through the RAMT approach experienced faster mobilization and recovered more efficiently, and their mechanical ventilation times were significantly shorter than in patients operated via median sternotomy [7]. Similar results were achieved by Gilmanov et al. [6].
Apart from the retrospective and observational nature of this paper, what limits our study is the small sample size (n = 3) and short follow-up period. However, no patients undergoing ascending aorta surgery via the RAMT approach were excluded.
In conclusion, we recommend this approach for ascending aorta surgery, especially for patients with advanced age or serious comorbidities, such as pulmonary disease. Our experience is small in terms of ascending aorta surgery via RAMT but vast in procedures for valvular heart disease with this approach. Nevertheless, it should be performed with due caution by surgeons with little experience in minimally invasive techniques.