Introduction
Injuries represent a significant challenge within the healthcare system, leading to high rates of disability and mortality among affected individuals. The World Health Organization reports that injuries are responsible for 5 million deaths globally, with approximately 50% of fatalities occurring in individuals aged 15 to 44. This situation notably impacts the economic and productive workforce, particularly in developing nations, underscoring its social and economic ramifications [1].
Thoracoabdominal injuries, which are a subset of combined injuries, make up 40% of cases and occur concurrently with trauma to organs in two separate serous cavities. These injuries often result in severe hemorrhaging, shock, and peritonitis, necessitating prompt surgical intervention [2–4]. However, diagnostic and tactical errors – ranging from 30% to 70% – along with postoperative complications and a mortality rate of 30%, remain prevalent in treating this patient population. Consequently, there is a pressing need to explore and enhance both new and existing methods for diagnosing and treating thoracoabdominal injuries [5–8].
Aim
The aim of this study is to improve surgical management for thoracoabdominal injuries by developing an optimal diagnostic and treatment algorithm based on the use of endovideosurgical techniques.
Material and methods
The study was conducted through a comparative analysis of 190 (100.0%) patients diagnosed with chest and abdominal injuries at the Andijan branch of the Republican Scientific Center for Emergency Medical Care between 2017 and 2022. Patients were categorized into two primary groups based on their diagnostic and treatment methods. The comparative group included 122 patients who received standard traditional diagnosis and treatment methods between 2017 and 2020. In the comparison group, all 122 (100.0%) patients were categorized based on the nature of their injuries as follows: thoracic injuries – 31 (25.4%), abdominal injuries – 59 (48.4%), and combined thoracic and abdominal injuries – 32 (26.2%) patients. In contrast, the main group consisted of 68 patients who were treated in the period 2021 to 2022, employing enhanced surgical techniques derived from endovideosurgery practices. In the main group (68 patients), thoracic injuries were observed in 20 (29.4%), abdominal injuries in 28 (41.2%), and combined thoracic and abdominal injuries in 20 (29.4%) patients (Table I).
Table I
Distribution of patients based on the nature of their injuries
The ages of the patients ranged from 18 to 88 years, with the largest cohort comprising 126 individuals (66.3%) aged between 18 and 44 years. Injury severity was assessed using the New Injury Severity Score (NISS). The average severity scores for chest injuries in the main and comparative groups were 12.05 ±1.34 and 12.32 ±1.15 points (p = 0.878), respectively, while the scores for abdominal injuries were 13.57 ±1.04 and 13.51 ±0.84 points (p = 0.962). In patients with combined chest and abdominal injuries, the main group recorded an average NISS of 19.35 ±1.45, compared to 19.22 ±1.33 in the comparative group (p = 0.947).
Differentiated surgical management for the diagnosis and treatment of thoracoabdominal injuries
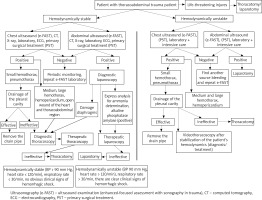
To enhance treatment outcomes for patients with thoracoabdominal injuries, an advanced diagnostic and treatment algorithm was implemented for those in the main group. This algorithm began with an assessment of the patient’s hemodynamic status. If the patient exhibited hemodynamic instability (systolic blood pressure < 90 mm Hg, heart rate > 120 beats per minute, respiratory rate > 30 breaths per minute, or signs of clinical hemorrhagic shock) and there were indications of vital organ injury (e.g., massive intrapleural or abdominal bleeding due to large vessel damage, pericardial tamponade, endobronchial bleeding, or terminal conditions), prompt thoracotomy and/or laparotomy were performed. If hemodynamic instability was present without signs of vital organ injury, an ultrasound examination was conducted following the extended Focused Assessment with Sonography for Trauma (e-FAST) protocol for both the chest and abdomen. If e-FAST revealed small to medium hemothorax or pneumothorax during chest examination, pleural drainage was undertaken. If necessary, the drainage tube could be removed, or video-assisted thoracoscopy could be performed. In cases where pleural drainage was ineffective, thoracotomy was warranted. If e-FAST indicated a significant hemothorax or hemopericardium, thoracotomy was also indicated. If the abdominal e-FAST results were positive, laparotomy was performed. In the event that both chest and abdominal e-FAST results were negative, further investigation was required to identify the source of bleeding, followed by a repeat e-FAST.
For patients with stable hemodynamics (systolic blood pressure > 90 mm Hg, heart rate < 120 beats per minute, respiratory rate < 30 breaths per minute, and no overt signs of hemorrhagic shock) and thoracoabdominal injuries, an extensive ultrasound examination of the chest and abdomen, along with computed tomography, X-ray, laboratory tests, and other instrumental assessments, was carried out. If these evaluations indicated a small hemothorax or pneumothorax, pleural drainage was performed. If this intervention was ineffective, or if stab wounds to the heart or thoracoabdominal area, medium to large hemothorax, or hemopericardium were identified, video-assisted thoracoscopy was utilized. If video-assisted thoracoscopy revealed diaphragmatic injury, video-assisted laparoscopy was performed in the subsequent stage to address this damage. If video-assisted thoracoscopy did not resolve the injury, thoracotomy was performed. During abdominal cavity examinations, if damage was noted (e.g., free gas or fluid), video laparoscopy was conducted to address the injury. Additionally, positive results from rapid analyses for abdominal cavity fluid, such as elevated alkaline phosphatase and amylase levels, indicated potential hollow organ injury that required intervention. If video laparoscopic approaches were unsuccessful, conversion to laparotomy was performed (Figure 1).
Results
Surgical tactics and procedures performed on the comparison group of patients
Traditionally and generally accepted diagnostic and treatment methods were applied to all 122 patients in the comparison group.
In this group, out of a total of 31 (100.0%) patients with thoracic injuries, pleural cavity drainage (PD) was sufficient for 13 (41.9%) patients. In 10 (32.3%) patients, pleural cavity drainage was initially performed, followed by thoracotomy (PD + thoracotomy) at a later stage, and in 8 (25.8%) patients, thoracotomy was performed directly. Among those who underwent thoracotomy, 6 (19.4%) patients had diagnostic procedures.
All 59 (100.0%) patients with abdominal trauma in the comparison group underwent laparotomy. In this group, diagnostic laparotomy carried out in 15 (25.4%) patients.
The following procedures were performed among all 32 (100.0%) patients with combined thoraco-abdominal injuries: primary surgical intervention + thoracotomy in 3 (9.4%) patients, primary surgical intervention + laparotomy in 3 (9.4%) patients, pleural drainage followed by laparotomy in 15 (46.9%) patients, and combined thoracotomy and laparotomy in 11 (34.3%) patients. Consequently, diagnostic thoracotomy was performed in 3 (9.4%) patients, while diagnostic laparotomy was performed in 6 (18.8%) patients.
Surgical management for main group patients
In all 68 patients of the main group, a surgical tactic developed based on endovideosurgical methods was used in diagnosis and treatment.
In the treatment of all 20 thoracic-injured patients of the main group, the following surgical procedures were utilized: pleural drainage for patients with chest trauma in 6 (30.0%) cases, PD combined with video-assisted thoracoscopy in 2 (10.0%) cases, video-assisted thoracoscopy alone in 8 (40.0%) cases, video-assisted thoracoscopy combined with thoracotomy in 1 (5.0%) case, and thoracotomy alone in 3 (15.0%) cases. No patients underwent diagnostic thoracotomy among thoracic-injured patients.
In all 28 patients with abdominal injuries in the main group, traditional surgical methods were used in some cases, while minimally invasive surgical methods were used in others. In this cohort, video laparoscopy was performed in 17 (60.7%) patients, video laparoscopy followed by laparotomy in 2 (7.1%) patients, and laparotomy was carried out in 9 (32.1%) patients directly. Diagnostic laparotomy was conducted on 1 (3.6%) patient in this group.
For all 20 patients with combined chest and abdominal injuries in the main group, the surgical interventions included: PD followed by laparotomy and video-assisted thoracoscopy in 6 (30.0%) patients, thoracotomy combined with video-assisted laparoscopy in 4 (20.0%) patients, laparotomy combined with PD in 2 (10.0%) patients, thoracotomy and laparotomy in 3 (15.0%) patients, and video-assisted thoracoscopy followed by video-assisted laparoscopy in 5 (25.0%) patients.
An analysis of the outcomes associated with the proposed surgical tactics and techniques for managing thoracoabdominal injuries was conducted, focusing on operational characteristics, postoperative complications, and mortality rates.
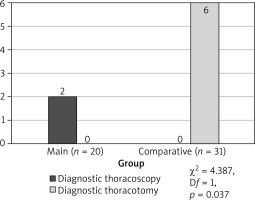
Regarding thoracic injuries, the implementation of endovideosurgery methods and enhanced surgical tactics resulted in the avoidance of diagnostic thoracotomy in the main group. Instead, diagnostic thoracoscopy was performed in 2 (10.0%) patients. In contrast, the comparison group underwent diagnostic exploratory procedures in 6 (19.4%) patients (χ2 = 4.387; Df = 1; p = 0.037) (Figure 2).
Following the operations with thoracic injuries in the comparative group, 9 (29.0%) patients experienced various complications. Specifically, wound suppuration was observed in 4 (12.9%) patients, pleural empyema in 2 (6.5%) patients, and reactive pleurisy in 3 (9.7%) patients. In contrast, only 1 (5.0%) patient in the main group developed a postoperative complication, which was a surgical wound suppuration. Additionally, there was 1 (3.2%) fatality in the comparative group due to acute blood loss, whereas no deaths occurred in the main group.
The analysis of the duration of surgical procedures, patient activation times, and the length of hospital stays yielded the following results: the average duration of surgery in the main group was 46.8 ±8.4 minutes, compared to 86.0 ±9.6 minutes in the comparative group (t = 3.07; p = 0.004). Patient activation occurred at an average of 12.4 ±1.6 hours postoperatively in the main group, while activation in the comparative group took place after 19.0 ±2.0 hours (t = 2.53; p = 0.015). The length of hospital stay for patients in the main group was 5.1 ±0.4 days, whereas those in the comparative group stayed for 7.8 ±0.6 days (t = 3.73; p < 0.001) (Table II).
Table II
Duration of surgery, postoperative patient activation time and hospital stay for thoracic injuries
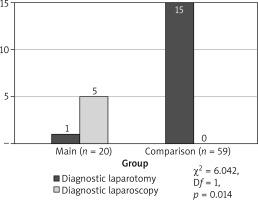
In patients with abdominal trauma, the implementation of endovideosurgery and enhanced surgical tactics led to a significant reduction in the need for diagnostic laparotomies, decreasing from 25.4% to 3.6% (a sevenfold reduction) (χ2 = 6.042; Df = 1; p = 0.014). Specifically, in the comparative group, diagnostic laparotomy was performed on 15 (25.4%) patients. In contrast, within the main group, only 1 (3.6%) patient underwent diagnostic laparotomy, while 5 (17.9%) patients had diagnostic laparoscopy performed (Figure 3).
Following the surgical procedures with abdominal injuries in the main group, complications were noted in 2 (7.1%) patients: 1 (3.6%) patient experienced suppuration of the postoperative wound, and another (3.6%) developed pneumonia. In the comparison group, complications included wound suppuration in 6 (10.1%) patients, peritonitis in 2 (3.4%) patients, pneumonia in 4 (6.8%) patients, reactive pleurisy in 4 patients (6.8%), and pleural empyema in 2 patients (3.4%).
Postoperative complications were addressed using both conservative and surgical interventions. Specifically, in the comparison group, 2 (3.4%) patients died on the first day after surgery due to hemorrhagic shock and multiple organ failure.
The average duration of surgery in the main group was 57.5 ±4.6 minutes, compared to 82.5 ±4.3 minutes in the comparison group. Patient activation times following surgery averaged 14.4 ±1.5 hours in the main group (t = 3.95; p < 0.001), while activation in the comparison group took an average of 24.3 ±0.7 hours (t = 5.95; p < 0.001). Additionally, the length of hospital stay was significantly shorter for patients in the main group, averaging 5.1 ±0.3 days compared to 8.7 ±0.7 days in the comparison group (t = 4.97; p < 0.001) (Table III).
Table III
Indicators of time spent on operations and postoperative patient activation and hospital stay for abdominal injures
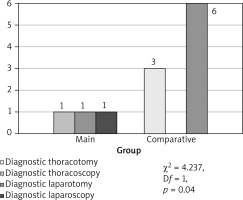
Combined thoracic and abdominal injuries. In the comparison group, diagnostic thoracotomy was performed on 3 patients (9.4%), while diagnostic laparotomy was conducted in 6 (18.8%) patients. Conversely, in the main group, diagnostic laparotomy was performed in only 1 (5.0%) patient, along with diagnostic videothoracoscopy in another patient (5.0%) and diagnostic laparoscopy in yet another patient (5.0%). These data indicate a significant reduction in the use of diagnostic open surgery, decreasing from 28.2% to 5.0% (χ2 = 4.237; Df = 1; p = 0.040) (Figure 4).
The implementation of endovideosurgical techniques and enhanced surgical strategies in the main group led to a notable reduction in the occurrence of postoperative complications. In this cohort, complications were recorded in only 2 patients: 1 (5.0%) patient experienced suppuration of the postoperative wound, and another (5.0%) developed reactive pleurisy in main group patients. In contrast, the comparison group exhibited a higher complication rate, with 12 (37.5%) patients affected. Among these, 4 (12.5%) patients had wound suppuration, 1 (3.1%) patient presented with a subdiaphragmatic abscess, 1 (3.1%) patientdeveloped peritonitis, 2 (6.3%) patients had pneumonia, 3 (9.4%) patients experienced reactive pleurisy, and 1 patient (3.1%) suffered from pulmonary embolism, all of which are typically associated with open surgical procedures. Additionally, in the main group, 1 (5.0%) patient succumbed to septic shock and multiple organ failure. In the comparison group, despite receiving medical intervention, 2 (9.4%) patients died due to multiple organ failure, while 1 (3.1%) patient died from pulmonary embolism and another (3.1%) from acute blood loss and hemorrhagic shock.
The average duration of surgical procedures for patients in the main group was 87.5 ±4.4 minutes, compared to 126.4 ±10.5 minutes in the comparison group (t = 3.46; p = 0.001). The postoperative activation period for patients in the main group averaged 18.0 ±1.7 hours, whereas it was 25.9 ±1.5 hours for those in the comparison group (t = 3.41; p = 0.001). An analysis of hospital stay duration indicates improved outcomes for the main group, which averaged 6.8 ±0.5 days, compared to 10.0 ±1.1 days in the comparison group (t = 2.69; p < 0.01) (Table IV).
Table IV
Time spent on surgery and patient activation, hospital treatment duration in patients with thoracic and abdominal injuries
Discussion
The analysis of diagnostic and treatment outcomes has shown that using the surgical tactics developed based on endovideosurgical methods in thoracoabdominal injuries offers significant advantages compared to standard surgical approaches. The primary reasons for this include the higher complication rates following open procedures, prolonged post-operative recovery time before patient mobilization, and an increase in hospital stays, leading to a more challenging recovery process after surgery.
Thorough analysis of the diagnostic and treatment outcomes reveals that the use of endovideosurgery techniques and enhanced surgical approaches has led to a significant reduction in postoperative complications for all characterized injured group patients. Postoperative complications decreased from 29.0% to 5.0% in patients with thoracic trauma (χ2 = 4.454; Df = 1; p = 0.035).
The mortality rate in the comparison group was 3.2%, while no fatalities were recorded in the main group (χ2 = 0.658; Df = 1; p = 0.42).
For patients with abdominal injuries, postoperative complications fell from 30.5% to 7.1% (χ2 = 5.856; Df = 1; p = 0.016), with a mortality rate of 3.39% in the comparison group and no deaths in the main group (χ2 = 0.971; Df = 1; p = 0.325).
In cases of combined thoracic and abdominal injuries, the rate of postoperative complications decreased from 37.5% to 10.0% (χ2 = 4.731; Df = 1; p = 0.03), while the mortality rate declined from 12.5% to 5.0% (χ2 = 0.797; Df = 1; p = 0.373).
The study demonstrated that implementing the proposed surgical tactics allows for rapid diagnosis of patients and facilitates the selection of optimal treatment methods by incorporating both traditional and modern minimally invasive techniques. As a result, the number of unnecessary open diagnostic operations decreases, disability rates are reduced, and patients are able to return to active lifestyles earlier.
Several studies have been conducted on the application of endovideosurgical procedures for thoracoabdominal injuries. Among them, Khat’kov [9] extensively utilized laparoscopy and thoracoscopy for patients with thoracic and abdominal trauma in emergency surgery. They noted that the use of endovideosurgical techniques significantly reduced postoperative complication and mortality rates in these patients. According to the results of their clinical studies, the rate of postoperative complications following endovideosurgical interventions was 15.6%, and the mortality rate was 5.6%. Furthermore, they highlighted that 13.3% to 19.6% of patients who underwent endovideosurgical operations showed no signs of internal organ damage to the thoracic and abdominal cavities, and the number of unnecessary diagnostic thoracotomies and laparotomies was significantly reduced.
Mjoli et al. (2015) described the difficulties in diagnosing and treating thoracoabdominal injuries. They reported that diaphragm injuries were observed in 40.3% of patients with left-sided thoracoabdominal trauma. They emphasized that diaphragm injuries could not be detected through radiological (X-ray) examination methods but were identified and resolved using endovideosurgical techniques [10].
Additionally, Puzanov et al. (2014) emphasized the effectiveness of using endovideosurgical methods in diagnosing and treating thoracoabdominal injuries, stating that video laparoscopy served as a diagnostic method in approximately 57% of cases involving such injuries. At the same time, he noted that endovideosurgical procedures involve complex techniques, with associated complications reaching up to 11.2% [11].
The studies conducted by the authors mentioned above have also demonstrated the advantages of endovideosurgical methods over traditional techniques in thoracoabdominal injuries. Nevertheless, our research revealed that utilizing a differentiated algorithm when employing endovideosurgical methods could further improve diagnostic and treatment outcomes.
It should be particularly noted that despite numerous studies and analyses, the use of endoscopic surgical methods in diagnosing and treating this category of injuries – especially the indications, contraindications, capabilities, and limitations of endovideosurgical techniques – remains insufficiently explored. The choice of an optimal surgical strategy for patients continues to be a topic of debate. Research indicates the need to further explore measures that allow the selection of appropriate surgical tactics for thoracoabdominal injury patients at all stages of diagnosis and treatment while ensuring that postoperative complications are not increased when using minimally invasive technology.
Conclusions
Endovideosurgical technique proves to be a safe and effective method for managing thoracoabdominal injuries. The adoption of minimally invasive and improved surgical strategies has resulted in shorter hospital stays, fewer exploratory operations, a decrease in postoperative complications, and thorough evaluations with no missed injuries.