For all the happiness mankind can gain is not in pleasure, but in rest from pain.
John Dryden
Introduction
Pain is one of the most common symptoms in the course of cancer. It is usually diagnosed at the somatic (functional) level of the advanced form of the disease; however, it occurs much earlier in the psychogenic form (so-called psychic pain). Pain as a psychosomatic phenomenon should be considered individually, multidimensionally, and taking into account the subjectivity of feelings of the patients experiencing it. According to the International Association for the Study of Pain and World Health Organisation (WHO), pain is defined as an “unpleasant sensory and emotional experience caused by actual or potential tissue damage”. This definition distinguishes between a sensory component, associated with the perception of pain, and an emotional component, associated with psychological reactions to perceived pain stimuli. The definition of pain distinguishes the following dimensions:
physical – associated with physiological symptoms,
functional – assessed on the basis of the patient’s daily functioning and performance of self-service activities,
psychosocial – taking into account the impact of the pain experience on mental processes (mainly emotional) and the impact on the quality and quantity of relationships,
spiritual – related to life attitudes, the meaning of suffering, and the purpose of life,
behavioural – focusing on past experiences of pain, the current impact of pain on psychophysical conditions, and adaptation to cancer [1–4].
Older people differ significantly in the dynamics and intensity of pain symptoms in the course of cancer. In some, the pain may be more intense due to psychogenic symptoms, while in others it may be the same as the current physical (somatic) condition. In both cases, it is necessary to implement therapies that can eliminate the experienced pain, which significantly reduces the negative consequences both physiologically and psychologically [3, 4].
The elderly often experience impaired absorption, metabolism, and elimination of analgesics from the system due to emerging physiological changes. The elderly are also at risk of polypharmacy due to comorbidities. Therefore, an individual patient approach is necessary to adequately monitor and treat pain in this population [4].
Causes of pain in cancer patients
Pain in cancer patients results from complex pathological mechanisms, including cellular, tissue, and systemic changes caused by growing tumour tissue, as well as changes associated with progressive, debilitating disease, e.g. bedsores, mucositis, mycoses, or muscle contractures.
The following distinctions can be made:
pain directly caused by cancer and its treatment,
breakthrough pain,
other pain syndromes accompanying cancer [5].
Pain caused by cancer and its treatment
The pathophysiology of pain involves 2 main mechanisms; mechanical and/or chemical irritation of pain receptors (nociceptors), i.e. receptor pain – in which somatic and visceral pain can be distinguished, and pain independent of pain receptor activation – caused by damage to the somatosensory nervous system, i.e. neuropathic pain [6].
The causes of somatic pain include infiltration of soft tissues, serous membranes, and occlusion of blood and/or lymphatic vessels by the tumour mass. In contrast, visceral pain is caused by, among other things, stretching of the sensory innervated capsule of an organ, ischaemia of tissues due to infiltration supplying blood vessels, or compression of ligaments, blood, or lymphatic vessels by tumour tissue [7].
Neuropathic pain occurs in approximately 20–25% of patients [8].
The pathophysiology of this pain involves damage to the nervous system through the following mechanisms:
direct compression and nerve infiltration by the tumour mass,
toxic effects of cytostatic drugs, molecular therapies, and radiotherapy,
the release of toxins by the tumour and autoimmune reactions (paraneoplastic syndromes) [9].
Patients with neuropathic pain, which is especially frequent in the elderly and multi-disease burden population, complain of burning, tingling, or numbness in a specific area of the skin surface, with attacks of sudden, very strong, piercing, wrenching pain along the limb. On neurological examination of such patients, significant hypersensitivity to touch and other delicate stimuli (so-called allodynia) and sensory disturbances in the form of hypersensitivity and paraesthesia are noted [10]. Compression or infiltration of peripheral nervous system structures by the neoplastic process may occur in the form of plexopathy or mononeuropathy. The most common causes of cervical plexopathy are head and neck tumours, and metastases in the cervical lymph nodes. Brachial plexopathy is common in the case of breast cancer metastases to axillary lymph nodes, in lymphomas and Pancoast tumours. On the other hand, lumbosacral plexopathy usually accompanies lymphoma, colorectal cancer, cervical cancer, and sarcomas. The most common cancer-associated mononeuropathy is intercostal nerve neuropathy secondary to rib metastases or chest wall infiltration [11].
Hand and foot pain in the form of ‘numbness’, paraesthesia, and burning sensations occur as side effects of cytostatic (taxans, oxaliplatin, thalidomide) [12]. They are characterized by low sensitivity to analgesic treatment, and in some patients they may develop into chronic pain [13].
Breakthrough pain
The definition of breakthrough cancer pain (BTcP) was developed by the Scientific Committee of the Association for Palliative Medicine of Great Britain and Ireland in 2009 and defined as a transient exacerbation of pain that occurs spontaneously or due to a specific predictable or unpredictable factor, despite a relatively stable and adequately controlled pain background [14]. It is characterized by an abrupt onset and short duration of the episode (30–60 minutes), which usually reaches a peak of severity over a period of 5 minutes [15–17]. Episodes of BTcP usually occur 2–3 times a day, and the most common trigger is physical activity. There are 2 categories of breakthrough pain:
incidental, triggered by a specific factor, and idiopathic,
unpredictable and usually lasts longer. Incident pain is further divided into subtypes: volitional (associated with will-dependent activity, e.g. movement), non- volitional (associated with activity independent of the will, e.g. contraction of intestinal smooth muscle), and procedural (associated with therapeutic interventions). End-of-dose pain, which occurs before the next dose of a regularly used analgesic and requires adjustment of the treatment of baseline pain, is not included as breakthrough pain [18].
Epidemiology of pain in older people
It is estimated that 40–80% of chronic patients under hospice care experience significant pain, which causes physical distresses, interferes with activities of daily living, increases the risk of adverse outcomes, and impairs quality of life [19–21]. The prevalence of pain in adult patients increases with age and rises significantly in the over-65-year-old population [22, 23].
A meta-analysis has shown that cancer pain is present in 55% of patients during cancer treatment, 39% of patients after treatment, and 66% of patients with disseminated cancer [24]. Although not all studies included in the analysis concerned patients over 65 years of age, the fact that the vast majority of cancers occur in this population makes it possible to extrapolate the results obtained to the elderly group. In this group of patients, the coexistence of complaints related to cancer and pain resulting from associated diseases is frequent [21]. Brunello et al. [25] have shown that almost half of cancer patients over 70 years of age suffer from non-cancer-related pain. Joint, back, and neck complaints are the most common [23, 26].
Assessment of pain intensity
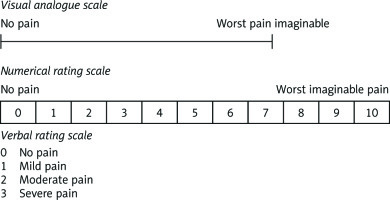
The assessment of pain in elderly patients is particularly difficult because, despite the more frequent experience of pain, they report it less frequently than younger patients [27]. This is because they show greater tolerance to pain, recognizing that it is an inherent part of the ageing process, and deny its existence. Negation may also result from fear of disease progression, of which increasing pain is a symptom, or lack of confidence in the effectiveness of therapy [22, 28]. This assessment may also be hindered by concomitant diseases, which make contact with the patient difficult and often significantly affect the self-assessment of pain. These include visual and auditory impairment, memory loss, disorientation, and dementia [28, 29]. Pain is a subjective symptom so self-reporting is the golden standard. The comprehensive assessment should include its localization, intensity, character, radiation, duration, exacerbation, and relieving factors as well as pain severity [19, 21]. It is standard practice to use pain scales: single-dimensional – the simplest (Table 1) – or multidimensional in the form of complex questionnaires, serving simultaneously to assess the severity and impact of pain on different aspects of a patient’s functioning. This multidimensional design allows for the selection of an appropriate therapeutic method while providing a better assessment of treatment efficacy compared with single-dimensional scales. A comparison of available pain assessment tools optimized for different patient populations was recently presented in 2 independent review papers [30, 31].
One of the most widely used multidimensional questionnaires designed for older people is the Brief Pain Inventory, which assesses cancer pain-induced changes in the performance of daily activities. These changes can lead to deterioration in performance status, treatment tolerance, and ultimately quality of life [19, 30].
When addressing pain assessment in the elderly, special attention should be paid to patients with cognitive impairment (i.e. dementia or delirium). When pain estimation based on self-assessment is questionable or impossible, it is necessary to observe symptoms that may be suggestive of the patient’s complaints (changes in mood or behaviour, changes in daily activities). Particularly useful in such patients are also the observations of caregivers who have regular contact with the patient and can most effectively observe these symptoms [20, 21, 28, 32].
To be able to express pain intensity in a quantifiable way, unifying pain assessment tools have been developed based on observations of patient behaviour. These include the Critical Care Pain Observation Tool (CPOT) [33], the Multi-dimensional Objective Pain Assessment Tool (MOPAT), and the Pain Assessment in Advanced Dementia (PAINAD) [34, 35]. Wiegand et al. [36] believe that the MOPAT questionnaire is applicable in patients unable to communicate verbally as a suitable tool for pain assessment. The inclusion of a geriatric examination allows for a multidimensional determination of the patient’s condition – assessing the impact of pain on the patient’s daily activities or detecting other factors that worsen the patient’s condition, such as comorbidities, depression, and lack of social support, and identifying those disorders whose treatment can most effectively improve the patient’s quality of life [19, 21, 23]. The most widely used tool for this purpose, with proven effectiveness in cancer patients, is currently the Comprehensive Geriatric Assessment Tool [37, 38] (Fig. 1).
Pharmacotherapy
World Health Organisation analgesic ladder step I
With pain intensity on the numerical rating scale (NRS) of values 1–4, non-opioid analgesics are used. In this group of drugs, we distinguish non-steroidal anti-inflammatory drugs, effective especially in nociceptive pain, and paracetamol and metamizole, effective in visceral colicky pain. The use of these drugs combined results in an additive analgesic effect. When choosing a drug from this group in the elderly, contraindications and the risk of cardiovascular, gastrointestinal, and renal complications must be taken into account. In addition, non-opioid analgesics are recommended to be administered orally or intravenously because of reduced pain on administration, short latency period, and variable analgesic effect profile. For all drugs, in this group, a so-called ‘ceiling dose’ has been defined, above which, in the absence of increasing analgesic effect, the risk of adverse reactions increases. The doses differ in elderly patients [40].
Ceiling doses:
metamizole (maximum daily dose 5 g) – in the elderly, in poor general condition, and with reduced creatinine clearance, lower doses should be used [41],
paracetamol – 15 mg/kg body weight, in elderly patients the maximum daily dose is 2 g/day [42],
non-steroidal anti-inflammatory drugs: short duration of use is recommended in the elderly due to the side-effect profile. The risk of gastrointestinal bleeding increases with age and the duration of treatment. NSAIDs increase the risk of cardiovascular incidents in the elderly [43].
World Health Organisation analgesic ladder step II
This group of drugs is used for moderate pain 4–7 on the NRS scale or in case of persistence of NRS > 3 pain despite treatment with WHO step I drugs. These analgesics are used alone or in combination with non-opioid drugs and show a ceiling effect of analgesia.
Ceiling doses:
tramadol – 400 mg in the elderly < 75 years of age with clinical signs of hepatic and renal failure or over 75 years of age without symptoms, elimination of the product from the body may be delayed, and therefore the interval between successive doses should be extended depending on the patient’s needs [44],
codeine – 240 mg, in the elderly there is an increased risk of side effects especially respiratory insufficiency, and therefore it is recommended that the lowest effective dose be used for as long as possible,
dihydrocodeine – 240 mg, usually better tolerated than codeine,
morphine – up to 30 mg per day, oxycodone up to 20 mg per day, administered orally.
World Health Organisation analgesic ladder step III
Drugs used in NRS 7–10 pain intensity, when NRS > 3 pain intensity despite the use of step II drugs, and as a continuation of low-dose morphine and oxycodone therapy on the WHO analgesic ladder step II. The principle of opioid titration applies.
Morphine – in patients treated with step II opioids, start with 2.5–5 mg immediate-release (IR). Every 6–8 hours, the dose before going to bed should be increased by 50% or 10 mg every 12 hours as SR (slow release). The equivalent dose of the orally administered drug is approximately 3 times higher than the subcutaneous or intravenous route. It is the first-line drug in patients with pain and dyspnoea. Morphine given to patients with renal colic or biliary disorders may exacerbate pain. Other opioids (methadone, fentanyl, buprenorphine) should be used in patients with abnormal renal function; oral morphine should be strongly avoided. In elderly patients, combined use of morphine with benzodiazepines and other CNS depressants should be avoided (risk of hypotonia, respiratory depression). Anticholinergic drugs and serotonin receptor antagonists used together may aggravate constipation [45].
Oxycodone – (in the elderly, start with a dose of 2.5–5 mgevery 4–6 hours). The equivalent oral dose is about 2 times higher than the dose administered parenterally. It is particularly effective in the treatment of visceral, neuropathic, and bone pain. In elderly patients the lowest dose is used, increasing carefully until the pain is controlled.
Fentanyl – (start treatment at 12.5 mcg/h). The transdermal system is applied every 72 hours, with the first analgesic effect observed after 12 hours, and full analgesic efficacy is achieved in a week. The treatment should be started in the morning to minimize the risk of side effects at night. Dose escalation is performed after the application of 1–2 patches.
Buprenorphine – a patch applied every 72–96 hours. The analgesic effect occurs after 12–24 hours. It is the opioid of the first choice in patients with renal failure, hepatic failure, and in the elderly. There is no need to change the dosage in these patient groups.
Tapentadol (maximum daily dose 2 × 250 mg/day, in elderly patients’ treatment, should be started with 50 mg twice a day). This opioid is particularly recommended for neuropathic pain; dose modification is not necessary for the elderly.
Coanalgesics
These are drugs that complement the action of analgesics and have an additive effect in certain types of pain or prevent the occurrence of side effects of analgesics:
the anti-epileptic drugs gabapentin and pregabalin are recommended for the treatment of neuropathic pain. In elderly patients, side effects such as asthenia, drowsiness, and peripheral oedema are more common [46];
antidepressants – in particular duloxetine and venlafaxine, are recommended for the treatment of neuropathic pain in elderly patients with cancer due to their lower cardiotoxicity. In addition, they are used in chronic pain syndromes with depression, and relief of additional symptoms such as itching, insomnia, and anxiety. In the elderly, the risk of hyponatraemia and spasticity is significantly increased [47];
surface applied drugs (Lidocaine, Capsaicin) are useful in the treatment of peripheral, localized neuropathic pain in patients with hemiplegic neuralgia, persistent postoperative pain, or neuropathy following chemotherapy;
cannabinoids are not effective in the treatment of nausea, vomiting, and neuropathic pain. In addition, a high risk of adverse effects in the form of cardiovascular events has been demonstrated in older people, including those without a history of cardiovascular disease [48];
zoledronic acid and Denosumab are used for bone pain caused by bone metastases, treatment of hypercalcemia, and reduction of the risk of bone incidents [49];
glucocorticosteroids are used in neuropathic pain, bone pain, visceral pain, pain caused by intracranial tumour growth, or pain associated with lymphoedema. However, their prolonged use, especially in the elderly, can lead to serious side effects such as osteoporosis, hypertension, hypokalaemia, diabetes, susceptibility to infection, and skin thinning. However, in geriatric patients, the treatments used are not specified [50].
Surgical methods of pain treatment
Postoperative and cancer pain in the elderly is often not recognized and properly treated. Its occurrence may be underestimated and inadequately assessed due to cognitive impairment in the elderly, the presence of additional age- related or non-age-related disorders, or atypical pain symptoms resulting from pathophysiological processes [51, 52].
Surgical treatments used to relieve chronic pain include restorative and nerve destruction procedures. These can be divided into 3 groups:
corrective treatments – to improve anatomical conditions,
augmentation techniques – neuromodulation,
ablative procedures.
The choice of the appropriate type of intervention depends on the aetiology, distribution, and type of pain (receptor-neuropathic), as well as the expected survival time, and psychical and socioeconomic conditions [53, 54].
Damaging techniques continue to be the method of choice for drug-resistant pain syndromes, especially in patients with advanced cancer [54–57]. These include procedures to interrupt pain transmission to the spinal cord (neurectomy, ganglionectomy, rhizotomy), performed at the level of the spinal cord (DREZotomy, cordotomy, myelotomy), and at the level of the brain (mesencephalotomy, thalamotomy), and procedures to reduce pain sensation (cingulotomy). Ablations are more effective in nociceptive pain. Sympathectomy is currently used for visceral cancer pain. Dorsal rhizotomy and ganglionectomy are mainly used in visceral cancer pains of the trunk and neck. A dorsal rhizotomy of the spinal nucleus of the trigeminal nerve is used in localized pain of the trunk, limbs, and face. DREZotomy of the spinal cord and the tricuspid nucleus is used in localized pain in the trunk, limbs, and face. Indications include, but are not limited to, cancer pain (e.g. arm pain in Pancoast tumour). Cordotomy has remained a treatment for cancer pain in the absence of intrathecal analgesic administration. Myelotomy, like cordotomy, is mainly used when treatment with intrathecal analgesics is not effective. Classically, it involves cutting the anterior commissure of the spinal cord, in order to spare the anterior funiculus. A modification of this method has now been introduced following the discovery of pathways that conduct visceral pain in the posterior funiculus of the spinal cord. These procedures, which are safer than bilateral cordotomy, are used in cancer pain, especially nociceptive pain, of the abdomen, pelvis, perineum, and lower limbs, especially in the presence of sphincter disorders. Brain-damaging procedures are nowadays carried out very rarely. Mesencephalotomy, which is the equivalent of a cordotomy at the midbrain level and is used for cancerous headaches, neck, and upper limb pain in patients where intraventricular opioid administration is not possible. Thalamotomy using stereotactic radiofrequency thermoablation or stereotaxic radiosurgery is used for widely distributed cancer pain in the systemic spread and for bilateral, axial, or head and neck pain in which other procedures are less effective [58–63]. Removal of the pituitary gland (surgical, chemical, or stereotaxic radiosurgery) is used in multifocal pain caused by tumours, especially hormone-dependent ones (prostate cancer, breast cancer) in dissemination. The mechanism of action is not known, and the analgesic effect is not due to the regression of tumour lesions [64–66]. The most widely used in clinical practice at present are denervation of intervertebral joints in the lumbar-sacral and cervical spine performed by thermoablation, Gasser ganglion thermolysis and less frequently DREZotomy for the treatment of pain or spasticity, sympathectomies performed mainly by surgeons, neurectomies for intercostal neuralgia, and rare neuroablative procedures on the spinal cord and peripheral nerves in cancer. The most recent reports leading to a better understanding of the pathophysiology of pain indicate that pain described as paroxysmal/acute is more responsive to damaging treatments than continuous pain, indicating a different mechanism of onset and thus the need for different methods of treatment [67, 68].
The role of radiotherapy in pain management
Radiotherapy is an effective and recognized method of non-pharmacological treatment of pain. It is used in a wide range of clinical situations; treatment with analgesic intent is mainly palliative. The most common indications for analgesic radiotherapy are pain caused by solid tumours (e.g. lung cancer, metastatic lymph nodes, bladder cancer, gynaecological cancers), pain caused by pressure on nerve structures (spinal cord compression syndrome, root and plexus compression), and pain caused by increased intracranial pressure in secondary (more common) and primary brain tumours and bone metastases.
Palliative radiotherapy usually does not require hospitalization and can be performed as a one-day procedure, fulfilling the expectations of the palliative patient (short treatment time, low risk of serious complications, fast treatment delivery time). The most common regimens used for palliative treatment are a dose of 8 Gy given in one fraction, or 20 Gy given in 5 fractions on 5 consecutive working days.
The mechanism of the analgesic effect of radiotherapy is complex. The components of the analgesic effect include primarily cytotoxic effects (reduction of the number of tumour cells, reduction of tumour volume, and pressure on surrounding tissues) and change of cell environment conditions through modulation of chemical pain mediators, and inflammatory mediators (e.g. inhibition of osteoclast activation).
The most common indication for radiotherapy is pain caused by bone metastases, and it is the most common type of cancer pain. Its pathomechanism is complex; therefore, pharmacological control of pain is often difficult. Bone metastases occur in the course of the most common cancers: breast cancer, lung cancer, prostate cancer, colorectal cancer, thyroid cancer, kidney cancer, and myeloma. Radiotherapy causes pain relief in 60–90% of patients, with complete pain relief achieved in 25–50% of patients [69, 70].
The analgesic effect of irradiation treatment may appear with a delay of up to 3–4 weeks. In some patients (2–40%) a transient intensification of pain lasting 2–3 days may be observed [70].
The duration of the analgesic effect is on average 3–4 months. After this time, about half of the patients experience pain progression at the irradiated site. Repeat radiotherapy is effective in 50–60% of patients, and 16–28% of patients experience complete pain relief [69, 70]. Additional effects of radiotherapy in the treatment of bone metastases include a reduction in the incidence of pathological fractures (bone calcification effect in 30–40% of patients), a reduction in the risk of hypercalcaemia, prevention of core compression, and a reduction in the incidence of hospitalization [69, 71, 72].
In selected clinical situations, in the case of a small volume of single bone metastases (oligometastatic disease), treatment with irradiation may take the form of stereotactic radiotherapy, consisting of a high dose of 15–25 Gy, usually in a single fraction, to increase the possibility of local control of the metastatic focus. This type of radiotherapy produces an approximately 86% long-term analgesic effect [69].
Another type of radiotherapy for multiple bone metastases is systemic radiotherapy. It consists of intravenous administration of radioactive isotopes that selectively accumulate in the bone. The most commonly used radioisotopes are strontium 89, samarium 153, and radium 223. The analgesic effect is achieved in about 70% of patients and may persist for several months [69]. The prerequisite for qualification for radioisotope treatment is normal renal and bone marrow function parameters.
Radiotherapy used with analgesic intention is an effective and valuable method. It allows good pain control, reduces the doses of analgesics used, leads to an improvement in quality of life (QOL), improvement in an emotional state, improvement in sleep quality, and reduces the risk of constipation [69, 71–73]. It may lead to a prolongation of the patients’ overall survival (OS) [69]. The indication to radiation therapy of elderly cancer patients should take into account their performance status as well as the extent and the severity of comorbidities. Age per se is seldom a contraindication for radiation therapy.
Psychotherapeutic methods
Psychotherapy is not only exotherapeutic but also endotherapeutic, because its effects influence the functioning of the central nervous system, as well as subordinate systems. Considering the situation of the oncological patient, it is not uncommon to depart from classical therapeutic methods in favour of alleviating symptoms, providing emotional and instrumental support, as well as motivating for treatment, open communication with the treatment team, or adherence to medical recommendations [3].
In the treatment of the mentioned mental dysfunctions, both psychopharmacological treatment and psychotherapeutic treatment are distinguished [3].
Psychological factors influence both the experience of pain, and the response to its treatment in cancer patients. Fear of pain and untreated pain strongly influence stress and unpleasant psychopathological symptoms. Pain can occur from the time of cancer diagnosis and at any subsequent stage. It is usually psychological pain, experienced as an unpleasant, prolonged state affecting psychosocial functioning. It may be associated with mood disorders, anxiety, phobias, eating disorders, sleep problems, and psychosomatic phenomena (tension headaches, constipation, diarrhoea, abdominal pain, feeling of breathlessness, etc.) [3, 74].
The main problem seems to be inadequate communication, and often a lack of it. Patients are reluctant to mention their discomfort because they do not want to appear hypochondriacal or attention-seeking. Some patients dissimulate because they fear that the severity of their pain symptoms is linked to disease progression and may disqualify them from further oncological treatment. Implicit psychological distress can amplify pain expression and trigger a vicious cycle of increased pain expression and anxiety, and escalate opioid and benzodiazepine doses, which consequently also impairs cognitive function. It is therefore important to consider psychological factors as a core component of pain in patients with cancer at every stage of diagnosis and treatment. Psychotherapeutic and behavioural methods of treating cancer pain in the elderly should be considered not as complementary but combined with pharmacological methods for better and longer-lasting effects [2, 74–77].
The mental component of pain associated with oncological diagnosis and treatment can be influenced by many factors, including how doctors communicate the diagnosis, previous history of pain or mental disorders, support from caregivers and family, and personality traits such as how they think about pain and cancer, a sense of hope and optimism, and personality. Data show that older cancer patients report the highest levels of stress, depression, and anxiety symptoms at various stages of the disease [74].
The main goal of psychotherapeutic interventions is to ease mental symptoms that affect the perception of mental and physical pain by reducing tension and stress, improving sleep, and increasing the level of physical activity. The basic psychotherapeutic methods include the following: clinical diagnosis with emotional support, hypnosis, mental relaxation, respiratory relaxation, and psychoeducation. Research shows that skill-based interventions are slightly more effective than pain-reducing educational approaches [76].
Conclusions
Given the holistic view of health, defined as somatic, mental, and sexual health, contemporary oncological treatment should be multidisciplinary and should view health in much wider terms than those limited to the diagnosis and treatment of cancer. Multidisciplinary treatment has better and longer-lasting effects, both on the underlying disease and on adverse symptoms including cancer- related pain (Fig. 2).