Stent fracture (SF) is a rare complication of coronary stenting; however, the real prevalence of this phenomenon is presumably underestimated [1]. It may lead to adverse clinical events associated with an in-stent thrombosis and in-stent restenosis (ISR). Herein, we present a patient who underwent several stenting procedures resulting in the so-called “full-metal jacket”. This caused multifocal type IV SF and ISR leading to an occlusion of the right coronary artery (RCA) and coronary aneurysm formation.
A 63-year-old female patient was scheduled for an elective coronary angiography due to stable angina symptoms. Prior to the present admission, she had undergone 5 percutaneous coronary interventions (PCI) of the RCA, including repeated procedures for ISR (Figure 1 A). All the procedures were finished with stent implantation without intravascular ultrasound(IVUS)/optical coherence tomography (OCT) guidance, and no drug-eluting balloon (DEB) was used. This resulted in the so-called “full-metal jacket” with multiple layers of overlapping stents. The present coronary angiography revealed a multifocal type IV SF (a complete transverse fracture with displacement), chronic total occlusion (CTO) of the RCA, and coronary aneurysm formation at the level of the fractured stent (Figures 1 B, C). Furthermore, it demonstrated a significant lesion of the left circumflex coronary artery (LCx) which was responsible for the patient’s symptoms. PCI of the LCx was performed, while for the vessel with SF the watch-and-wait strategy was chosen. The patient was scheduled for a follow-up evaluation after 6 months with multislice CT and/or coronary angiography, and in case of the progression of the aneurysm, a percutaneous (implantation of a covered stent or stent-assisted coil deployment) or surgical closure will be considered. In the case of refractory angina with evidence of viable myocardium in the RCA territory (last echo showed akinesis of the RCA regions), PCI of the CTO (e.g. DEB-only PCI) could be considered. The decision will be made after weighing the pros and cons of these strategies in a shared-decision making process with the patient and the Heart Team.
Figure 1
A – Angiography of the right coronary artery 13 months prior the present admission; B – Coronary angiography demonstrating an aneurysm of the right coronary artery with a chronic total occlusion of the vessel and 3 stent fractures (at the level of the aneurysm; on the border between second and third segment of the vessel; and in the distal portion of the vessel); C – The so-called “dry cine” image demonstrating stent fractures; D – Risk factors of stent fracture
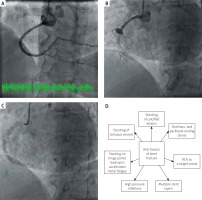
There are several risk factors of SF, i.e. stenting of RCA, longer stents, overlapping stents resulting in hinge movements, stenting of calcified lesions, high pressure deployment, and sirolimus- and paclitaxel-eluting stent implantation [1–3] (Figure 1 D). SF can be diagnosed with the use of intravascular imaging modalities, multislice CT, and sometimes by enhanced stent visualisation software tools (e.g. StentBoost or ClearStent) [4]. In the present case, SF was apparent on ordinary cine angiography without using high-resolution software protocols.
The case report highlights the shortcomings of the so-called “full-metal jacket” stenting, particularly with multiple overlapping stent layers in a patient with several risk factors of SF. Furthermore, it demonstrates that SF may translate into stent failure, ISR, CTO of a coronary artery, and aneurysm formation at the level of complete transverse SF. Available data suggest that in the worst case scenario this may lead to coronary rupture. The treatment strategy in such cases is yet to be defined, but probably an individualised approach should be considered. Given the presented case, interventional cardiologists should bear in mind potential negative consequences of the so-called “full-metal jacket” stenting. Furthermore, risk factors of SF should be taken into account when performing coronary interventions.








