A 45-year-old patient with COVID-19 infection was admitted to the cath lab due to ST-elevation myocardial infarction (STEMI). It was the 12th day of coronavirus disease 2019 (COVID-19) treated at home (2 preceding days of dyspnoea, recurring chest pain, and oxygen saturation of 90%). The patient had a history of arterial hypertension, type 2 diabetes, dyslipidaemia, and obesity. The ECG revealed ST-segment elevation in leads II, III, and aVF, with ST-segment depression in leads I and aVL. The patient received loading doses of acetylsalicylic acid and ticagrelor. Coronary angiography revealed a thrombus in the proximal right coronary artery (RCA) totally occluding the vessel lumen with no significant lesions in the left coronary artery (Figures 1 A, B). Percutaneous revascularization (PCI) was performed immediately. After advancement of a Pilot 50 guidewire and several predilatations (2.0 × 10 mm, 2.5 × 25 mm, 3.0 × 25 mm at 16 atm), aspiration thrombectomy was performed. Finally, 3 sirolimus-eluting stents were implanted (seg. 3: Orsiro 3.0 × 30 mm/12 atm; seg. 2/3: Orsiro 3.0 × 40 mm/18 atm; and seg. 1: Orsiro 3.5 × 22 mm/18 atm). Also, an intracoronary eptifibatide bolus was administered, followed by its intravenous infusion. At the end of the procedure, improved flow in RCA (TIMI 2) was achieved (Figure 1 C). The post-procedure echocardiography revealed akinesia of the apex, inferior wall, and lower part of the interventricular septum, with an ejection fraction of 40%. Moreover, a 20-mm thrombus was visible in the left ventricle’s lumen (Figure 1 D). Due to neurological abnormalities that appeared after PCI (Babinski’s symptom positive on both sides, strabismus divergent, wide, and non-responsive to light pupils, no reaction to pain), the suspicion of stroke was raised, and the eptifibatide infusion was discontinued. Head computed tomography (CT) revealed a hypodense lesion in the right and left thalamus, right cerebellar hemispheres, right occipital lobe, right midbrain, and the mass effect (Figure 1 E). The consulting neurologist diagnosed an extensive ischaemic stroke. Due to the CT image and exceeding the “time window”, the patient was disqualified from thrombolytic and endovascular treatment. The control echo confirmed the presence of a thrombus in the left ventricle. A control head CT revealed the progression and evolution of ischaemic lesions in the area of the basilar artery supply. Anti-oedema treatment (mannitol, furosemide) was initiated. On day 2, due to respiratory failure, the patient required mechanical ventilation. On day 3 cardiogenic shock occurred. Despite intensive pharmacological treatment including catecholamines, the patient’s condition deteriorated, and he died.
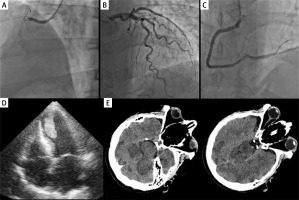
Figure 1
A – Totally occluded right coronary artery, B – non-obstructive left coronary artery, C – final view of the right coronary artery after PCI with three drug-eluting stents deployment, D – a large thrombus in the left ventricle, E – computed tomography showing massive ischaemic stroke
The COVID-19 has a tremendous impact on the management of STEMI patients [1]. As more than 2.5 years have passed since the pandemic’s beginning, our knowledge of this disease and its complications (both early and late) is more comprehensive. The SARS-CoV-2 infection causes many disturbances in the coagulation system, significantly increasing the risk of thromboembolic complications and causing damage to the endothelium, impairing its anticoagulant function [2]. We believe that our case presents a previously present thrombus in the left ventricle, which migrated and propagated to the right coronary artery (cardio-embolic source). Because stroke symptoms appeared after PCI, this suggest that during the procedure (e.g. with thrombectomy) the thrombus could have accidently migrated to the aorta and the brain. Unfortunately, thromboembolic events during COVID-19 worsen the prognosis and are also associated with increased mortality. Therefore, thromboembolic prophylaxis should be considered in patients with cardiovascular risk factors (in the discussed patient, 4 risk factors were present before STEMI) and severe infection [3–5].








