Surgical site infection (SSI) involving the mediastinum after cardiac surgical procedures carried out through median sternotomy is associated with significant mortality and morbidity [1]. Up to now a few methods have been describe to treat such severe adverse events in the early postoperative period [2]. One of them is negative pressure wound therapy (NPWT) [3]. Since its introduction by Argenta and Morykwas, NPWT has been an efficacious method, in terms of improved early and long-term outcomes, of managing SSI after cardiac surgical procedures [4]. This method was also proved to be of paramount importance in assisting wound healing in subjects at the highest risk for developing SSI, such as obese, insulin-treated diabetic and chronic obstructive pulmonary disease (COPD) patients [3]. In some individuals it may enable the infected wound to be closed definitely by playing the role of the intermediate stage before either placing mattress adapting skin sutures or transferring different local free cutaneous flaps with/without muscle tissue.
Herein we describe a patient history that illustrates not only the occurrence of post-sternotomy SSI in a high-risk patient, but also the benefits of NPWT in particularly challenging extensive infection-related loss of the thoracic and abdominal wall. A 69-year-old man was admitted to the Department of Cardiac Surgery in early September 2020 complaining of retrosternal pain and easy fatigability. The patient’s past medical history was gathered and revealed severe aortic stenosis accompanied by disseminated coronary artery disease (CAD) with significant lesions in the left anterior descending (LAD) and right coronary arteries (RCA). The comorbidities such as obesity, COPD, arterial hypertension, and diabetes mellitus were diagnosed. He had a history of two percutaneous coronary interventions (PCIs) and two cerebrovascular accidents (in 2001 and 2006). Of note, he has been an active heavy smoker (at least one pack per day) for more than 40 years. Additionally, the preoperative computed tomography (CT) revealed severe calcifications in all segments of the aorta as well as in celiac trunk. Eventually having in mind all risk factors he was qualified by the Heart Team for aortic valve replacement and coronary artery bypass grafting. During primary surgery severe calcification in the ascending aorta prevented safe application of cardio-pulmonary bypass and only the left internal mammary artery (LIMA) was implanted to the left anterior descending artery (LAD). A week later, due to instability he had repeat sternal reosteosynthesis with stainless wires and active mediastinal drainage then the transcatheter aortic valve implantation (TAVI) procedure was successfully performed. Unfortunately, after the following few days he again developed severe infection with sternal dehiscence. Repeat surgery revealed extensive infection of the bone with mediastinum exposure (type IV according to the classification proposed by Anger et al. [5]). NPWT was initiated with several changes of the foam but due to skin loss, closure with direct skin mattress sutures was impossible. Many pathogens were detected to cause sternal infections in around the chest wounds, mainly Klebsiella pneumoniae, Pseudomonas aeruginosa, Proteus mirabilis and Stenotrophomonas maltophilia. Antibiotics were administered periodically usually with vancomycin and linezolid. Eventually, after consultation with the plastic surgeon, reconstruction with a reversed pedicled rectus abdominis flap with a skin island was performed (Figure 1 A). However, due to infection of the abdominal wall, NPWT was again applied, but this time predominantly on the abdominal wall (Figure 1 B). It took 6 weeks to prepare the tissue base for intermediate thickness skin grafting (Figure 1 C) that eventually enabled wound closure. The patient spent 5 months in our department.
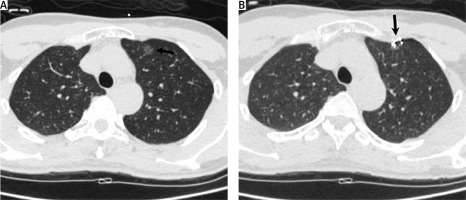
Figure 1
Stages of reconstruction of anterior thoracic wall defect with reversed pedicled rectus abdominis flap with a skin island. A pedicled rectus abdomens flap with a skin island (RAF) was harvested (A) but due to infection of subcutaneous tissue of the abdominal wall (*) (B), NPWT had to be applied to prepare (**) for intermediate partial-thickness skin grafting (C)
RAF – rectus abdominis flap, Th – thoracic wall.
SSI after cardiac surgical procedures leading to mediastinitis has been considered as one of the most serious complications. Although its incidence is not high, ranging between 1% and 3.4%, it is still associated with mortality rates of 10% to more than 30% and prolonged hospitalization [3, 4]. In our case, the patient had to be treated for approximately 5 months. However, the latest advances in surgical techniques and better understanding of the pathophysiology have led to better results in recent years [6, 7]. NPWT has made a major contribution to such recent outcomes even in high risk patients with well-known risk factors [7]. After reviewing both our patient’s medical history and these risk factors, we decided to initiate vacuum-assisted therapy early after failure of the only attempt of sternal bone re-stabilization.
This vacuum-assisted wound closure technique that uses subatmospheric pressure applied locally to a surgical site allows continuous, open drainage of exudate while maintaining sternal stability and wound isolation. It was also proven to increase dermal perfusion and granulation tissue formation, reduce edema and interstitial tissue fluid, reverse tissue expansion and reduce bacterial colonization [6]. We are sure that many aforementioned mechanisms of NPWT were of paramount importance in our patient. Due to infection-related skin damage, primary closure was not possible; therefore we treated the patient with NPWT to create optimal conditions for an intermediate skin transplant, which was successful.
Variability in NPWT application and general techniques for wound management and debridement among surgeons also present a challenge to standardized use of NPWT. The authors of this report hope to contribute and encourage further discussion and research for a systematic approach to NPWT as management after postoperative SSI.






