Introduction
Transurethral cystoscopy (CS) is a common urologic procedure, performed mostly for diagnosis of bladder cancer [1]. General indications for this procedure include hematuria (micro- and macroscopic), morphologic abnormalities of the bladder, trauma, foreign body removal, urinary incontinence, lower urinary tract symptoms, chronic urinary tract infections, hematospermia and azoospermia [1, 2].
There are two main types of instruments used for CS – rigid and flexible. The latter is considered to be generally less burdensome for the patient, while maintaining the comparable efficacy with rigid CS in the majority of purely diagnostic procedures [3]. However, rigid CS offers a wider working channel lumen and is essential in more demanding inpatient procedures [4, 5].
Cystoscopy is performed after standard physical examination, disinfection of external genitalia and intraurethral instillation of some form of lubricant [6]. In the majority of cases, no general anesthesia is required.
Even though CS is considered safe, complications such as hematuria (19%), dysuria (50%), frequency (37%), and urinary tract infection (2–3%) may occur [1, 7]. These problems are usually short-term, self-limiting and mild [6]. The risk of more serious complications, such as urethral damage and further stricture, severe infections and acute urinary retention, is extremely low [1, 6].
Cystoscopy, like any other invasive procedure, may cause pain, discomfort and stress in both men and women [8]. Greenstein et al. used a Visual Analog Pain Scale (VAS, 0–10 cm) in order to measure patients’ discomfort during CS. They analyzed 1320 procedures and found that rigid CS caused significantly more pain in men (3.4 ± 1.6) and women (2.5 ± 1.6) than flexible CS (2.5 ± 1.4 and 1.1 ± 1.9 respectively) [9]. Other studies also showed that rigid CS was less likely to be pain-free and could be even two times more painful than flexible CS [3, 4, 10]. It is worth emphasizing that undergoing first CS is a strong predictive factor for significant pain, probably because of increased preprocedural stress, anxiety and fear [9]. Also, preprocedural fear causes that patients who are listed for CS anticipate much worse pain compared to the pain they actually experience during the further procedure [2, 8].
In the majority of studies, males report significantly higher levels of perioperative pain than women. This is mainly caused by evident anatomical differences between the two sexes, as well as possible psychological and sociological issues. It should also be remembered that although CS is generally well tolerated, some patients describe pain related to the procedure as “unbearable” [4]. In consequence, many patients fear and avoid primary and/or follow-up cystoscopies. This may lead to uncontrolled progression of the disease. Providing the patients with appropriate care during CS can encourage them to comply with diagnostic schedules and improve their prognosis.
Evidence acquisition
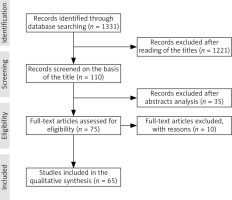
The PubMed electronic database limited to English articles published until January 2021 was used in the process. Search terms included: “cystoscopy pain”, “cystoscopy pain reduction”, “rigid cystoscopy pain reduction”, “flexible cystoscopy pain reduction”, “cystoscopy analgesia”, along with free text, related, derivative and exploded terms. Meta-analyses, systematic reviews, randomized controlled trials, clinical trials, prospective randomized studies, multicenter comparisons, reviews and retrospective comparisons were used. As a result, 65 articles were included in this review (Fig. 1].
Lidocaine gel
Topical lidocaine gel is the most popular form of anesthesia during CS. In theory, lidocaine gel lubricates and provides local analgesia in the urethra by inhibiting membrane voltage-gated sodium channels, thus blocking neurotransmission. However, despite many years of clinical implementation, there is still no consensus whether it reduces pain more than plain lubricating gel (Table 1).
Table 1
Lidocaine gel in pain reduction during cystoscopy compared to plain lubricant
| Name of first author | Year of publication | Type of article | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|
| Aaronson [11] | 2009 | Meta-analysis | 411 | Men | Flexible | Yes |
| Raskolnikov [12] | 2019 | Meta-analysis | 1549 | Men | Flexible | Yes |
| Patel [13] | 2008 | Meta-analysis | 817 | Men | Flexible | No |
| Chitale [14] | 2008 | Randomized controlled trial | 51 | Men | Flexible | No |
| Akkoç [15] | 2016 | Retrospective comparison | 220 | Men | Flexible | No |
| Cano-Garcia [16] | 2015 | Observational study | 72 | Both | Flexible | No |
| Dougher [17] | 2019 | Randomized controlled trial | 116 | Women | Flexible | Yes |
| Rappaport [18] | 2020 | Prospective randomized study | 120 | Women | Both | No |
| Goldfischer [20] | 1997 | Clinical trial | 179 | Both | Rigid | Men – Yes Women – No |
| Goktug [21] | 2014 | Randomized controlled trial | 320 | Men | Rigid | Yes |
| Vasudeva [22] | 2014 | Randomized controlled trial | 400 | Men | Rigid | Yes |
Lidocaine gel in flexible cystoscopy
A meta-analysis that included 14 studies published by Aaronson et al. in 2009 stated that intraurethral lidocaine gel injection increased comfort in men undergoing flexible CS [11]. This result was supported by Raskolnikov et al. in the most recent meta-analysis from 2019 [12]. On the other hand, after implementing slightly different inclusion criteria and statistical methods, Patel, Jones and Babineau stated that there was no difference in pain levels between lidocaine gel and plain lubricating gel during the procedure in men [13]. All of these meta-analyses used VAS scores if they were given. A variety of papers also proved that lidocaine gel does not reduce pain perception [14–16]. In women, Dougher et al. stated that lidocaine gel provided pain relief, while Rappaport et al. did not observe any beneficial influence (based on VAS scores) [17, 18]. What is more, Carrion et al. stated that the procedures performed only with irrigation solution as a lubricant were not more uncomfortable for the patients [19] (Table 2).
Table 2
Lubricant characteristics in pain reduction during cystoscopy
| Method | Compared to | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|---|
| Lubrication of the urethra | Saline solution | Carrion [19] | 2016 | 100 | Men | Flexible | No |
| Lidocaine spray | Aqueous lubricating gel | Choe [23] | 2008 | 144 | Women | Rigid | Yes |
| Lidocaine spray | Lidocaine gel | Choe [23] | 2008 | 144 | Women | Rigid | No |
| Dimethyl sulfoxide + lidocaine gel | Lidocaine gel | Demir [24] | 2008 | 140 | Men | Rigid | Yes |
| NaHCO3 buffered lidocaine gel | Lidocaine gel | Li [25] | 2016 | 60 | Men | Rigid | Yes |
| 20 ml of lidocaine gel | 10 ml of lidocaine gel | Holmes [27] | 2001 | 147 | Men | Flexible | Yes |
| 20 ml of lidocaine gel | 10 ml of lidocaine gel | McFarlane [31] | 2001 | 60 | Men | Flexible | No |
| 4 degrees C lidocaine gel | 22 degrees C lidocaine gel | Thompson [33] | 1999 | 60 | Men | No data | Yes |
| 4 degrees C lidocaine gel | 22 degrees C lidocaine gel | Goel [34] | 2003 | 40 | Men | No data | Yes |
| 10 seconds instillation of lidocaine gel | 2 seconds instillation of lidocaine gel | Khan [35] | 2002 | 100 | Men | No data | Yes |
Lidocaine gel in rigid cystoscopy
Data regarding lidocaine gel use in rigid CS is scarce. Nonetheless, most of the available papers suggest that its instillation before the procedure may decrease pain in men, but has no effect in women (based on VAS scores) [18, 20–22]. In women, intraurethral instillation of lidocaine gel was compared with direct application of lidocaine spray. Both agents lowered pain levels, but the delivery of lidocaine spray caused a mild discomfort [23] (Table 2). Other authors stated that adding dimethyl sulfoxide to lidocaine provided better anesthesia in men than lidocaine alone [24] (Table 2). Moreover, male patients might benefit from intraurethral instillation of lidocaine gel alkalized with NaHCO3 solution (Table 2). Alkalized lidocaine improves neural blockade and speeds up its onset time by facilitating the diffusion of lidocaine [25].
Dwell time of lidocaine gel
It was hypothesized that lidocaine gel is only helpful in decreasing pain in men if there is enough time between the administration of the gel and the onset of the procedure (Table 3). Studies showed that allowing the gel to dwell for 10 to 20 minutes before CS may be enough for lidocaine to diffuse through the mucosa [20, 22, 26, 27]. According to Vasudeva et al. and Choong et al., 15 minutes was the most favorable time of lidocaine dwell time [22, 26]. Importantly, starting the CS only 5 minutes or less after the instillation of the gel did not provide sufficient pain relief [28, 29]. However, some articles suggest that there was no difference whatsoever between instant and delayed cystoscopies [30].
Table 3
Influence of dwell time of lidocaine gel in pain reduction during cystoscopy
| Retention time | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|
| 15 minutes | Vasudeva [22] | 2014 | 400 | Men | Rigid | Yes |
| 15 minutes | Choong [26] | 1997 | 90 | Men | Flexible | Yes |
| 5 minutes | Panach-Navarette [28] | 2015 | 242 | Men | Flexible | No |
| 3 minutes | Losco [29] | 2011 | 50 | Men | Flexible | No |
| No data | Herr [30] | 2001 | 288 | Men | Flexible | No |
Other properties of lidocaine gel
There is no consensus whether the volume of lidocaine gel has an influence on patients’ comfort. Holmes et al. found that 20 ml is more advantageous than 10 ml, while McFarlane et al. did not observe any difference in pain perception between 10 ml and 20 ml of lidocaine gel (based on VAS scores) [27, 31] (Table 2). Moreover, Ho et al. suggested that the intraurethral injection of lidocaine gel can actually be more painful than the injection of plain gel, due to the chemical composition of lidocaine-based lubricant [32]. Regardless, it has been proven that in order to maximize the patient’s comfort during the administration of the gel, it should be cold (ideally 4 degrees Celsius) and instilled slowly (over 10 seconds) [33–35] (Table 2).
In conclusion, lidocaine gel efficacy remains controversial, but it should be used as long as it is undoubtedly proven ineffective. In order to increase the chances of pain reduction NaHCO3 or dimethyl sulfoxide can be added to the gel. It is crucial to slowly inject 10–20 ml of cold gel and wait some time before commencing the procedure.
Urination and high irrigation pressure
The time of the highest discomfort in men is when the cystoscope is passing through the external urethral sphincter [36–38]. It was hypothesized that micturition during cystoscope passage and/or increased hydrostatic pressure of the irrigation solution might serve a major role in reducing the discomfort associated with this part of the procedure in male patients (Table 4).
Table 4
Urination and high irrigation pressure in pain reduction during cystoscopy
| Method | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|
| Urination | Xie [36] | 2020 | 96 | Men | Flexible | Yes |
| Urination | Sarkar [37] | 2019 | 100 | Men | Rigid | Yes |
| Bag squeeze | Gunendran [38] | 2008 | 151 | Men | Flexible | Yes |
| High irrigation pressure | Zhang [39] | 2015 | 168 | Men | Flexible | Yes |
| Bag squeeze | Berajoui [40] | 2020 | 200 | Men | Flexible | Yes |
It has been proven that instructing the patient to urinate causes the external urethral sphincter to relax, thus opening the membranous urethra and facilitating scope passage [36]. The male patients who micturated during the insertion of the scope reported lower pain levels (VAS score and Hamilton Anxiety Rating Scale) [36, 37].
Another method of pain reduction for male patients may be the “bag squeeze” technique, which aims to create high irrigation pressure while passing the cystoscope [38]. Essentially, increased hydrostatic pressure of the irrigation solution serves to widen the urethra and to relax the external urethral sphincter. Again, this facilitates cystoscope insertion, which significantly reduces the discomfort (based on the VAS score) [38]. Independent studies from 2008, 2015 and 2020 unanimously confirmed that increased irrigation pressure during flexible CS was associated with lower pain levels in male patients [38–40]. Zhang et al. suggested that placing the irrigation solution bag 150 cm over the patient’s bed was more advantageous than squeezing the bag, because it maintained high and more consistent pressure, as well as eliminating the need for an additional assistant [39]. In conclusion, urination and “bag squeeze” are simple, free and effective ways that increase male patients’ comfort during CS.
Nitrous oxide
Nitrous oxide (N2O) is a fast-acting anesthetic and sedative known for its short-term action with few adverse effects. Nitrous oxide inhalation is often used in simple dental and pediatric procedures, but it can also be used in a variety of outpatient procedures [41]. There are, however, some contraindications to its use, such as intoxication resulting in hemodynamic instability, high intracranial pressure, bowel obstruction and pneumothorax [41].
Calleary et al. recruited 69 men into a study on the effect of Entonox (50% nitrous oxide and 50% oxygen) inhalation for 3 minutes before flexible CS. The Entonox group showed lower VAS scores, as well as a decreased pulse rate [42]. In other studies, N2O has been proven to provide a significant decrease of pain levels during CS, as well as during other outpatient urological procedures, such as prostate biopsy, ureteral stent placement and extracorporeal shockwave lithotripsy [41–43].
Distractions
Distracting the patients might be beneficial in lowering pain perception during CS [44]. Numerous methods can be used to shift patients’ focus away from the procedure. The most commonly used ones include real-time visualization of endoscopic view, music, movies, virtual reality and use of a “stress ball” [44–46] (Table 5).
Table 5
Distractions in pain reduction during cystoscopy
| Method | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|
| Real-time visualization and music | Gupta [44] | 2019 | 200 | Both | Rigid | Yes |
| Video, music, stress ball | Gezginci [45] | 2018 | 120 | Men | Rigid | Yes |
| Virtual reality | Walker [46] | 2014 | 45 | Men | Flexible | No |
| Real-time visualization | González-Padilla [47] | 2019 | 404 | Both | Men – Flexible Women – Rigid | Men – No Women – Yes |
| Real-time visualization | Patel [48] | 2008 | 100 | Women | Rigid | No |
| Real-time visualization | Zhang [49] | 2011 | 86 | Men | Flexible | Yes |
| Real-time visualization | Soomro [50] | 2011 | 76 | Men | Flexible | Yes |
| Real-time visualization | Patel [51] | 2007 | 100 | Men | Flexible | Yes |
| Real-time visualization | Cornel [52] | 2008 | 154 | Men | Flexible | No |
| Real-time visualization | Kesari [53] | 2003 | 51 | Both | Rigid | No |
| Music | García-Perdomo [54] | 2018 | No data | No data | Both | Yes |
| Music | Kyriakides [55] | 2018 | 331 | No data | Both | Yes |
| Binaural beats | Ölçücü [56] | 2021 | 252 | Men | Flexible | Yes |
| Video | Gezginci [57] | 2020 | 60 | Women | Rigid | Yes |
According to González-Padilla et al., allowing patients to watch their flexible CS on the screen was beneficial in women [47]. On the other hand, Patel, Jones and Bubineau claimed that there was no significant pain relief in women viewing their rigid CS [48]. Both research groups used VAS scores to assess the pain. Many articles showed divergent results – majority of them claimed that self-visualization significantly reduced discomfort [44, 49–51], while a few studies proved the method to be inefficient [52, 53]. Even though no definite conclusion about the efficacy of real-time self-visualization during CS can be made, it still should be implemented as a free and easy method that may reduce pain perception.
Listening to music is another well-researched method that can increase patients’ comfort. Two recent meta-analyses proved that listening to classical/folk/popular music could be beneficial in urological outpatient procedures, including CS [54, 55]. Listening to pure binaural beats (exposing each ear to two sounds of different frequencies, but steady intensity) might have a positive influence too. According to Ölçücü et al., binaural beats cause the brain’s dominant wave frequency to synchronize with these sounds, which might reduce patients’ anxiety during CS [56].
A few articles focused on movies and one study used VR as a distraction. The studies showed that watching a relaxing movie reduced the pain in rigid CS in both men and women [45, 57]. On the other hand, VR did not alleviate the pain in men undergoing flexible CS [46]. These studies used VAS scores, State-Trait Anxiety Inventory (STAI) and hemodynamic parameters.
Lastly, the direct comparison of different distraction methods favored the video as the one with the most positive influence on patients’ comfort [45].
It is worth noting that combining different distractions at the same time provided greater pain reduction than using only a single distraction [44].
Pharmacotherapy
Despite the existence of numerous efficient analgesic drugs, their administration prior to CS is not common. Many studies have been conducted on a variety of drugs and their influence on pain reduction during CS (Table 6).
Table 6
Drugs in pain reduction during or after cystoscopy
| Drug | Way of administration | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|---|
| Parecoxib | Intramuscular | Sun [58] | 2019 | 101 | Men | Rigid | Yes |
| Diclofenac | Intrarectal | Nadeem [59] | 2016 | 60 | Men | Flexible | Yes |
| Zaltoprofen | Oral | Komiya [60] | 2009 | 40 | Men | Rigid | Yes |
| Pipemidic acid | Oral | Yuri [61] | 2016 | 80 | Both | No data | Yes |
| Phenazopyridine | Oral | Yuri [61] | 2016 | 80 | Both | No data | Yes |
| Diclofenac | Oral | Yuri [61] | 2016 | 80 | Both | No data | Yes |
| Alprazolam | Oral | Ozkan [62] | 2017 | 86 | Men | Flexible | Yes |
| Midazolam | Intravenous | Song [63] | 2007 | 80 | Both | Both | Yes |
| Remifentanil-dexmedetomidine | Intravenous | Arpaci [64] | 2013 | 40 | Both | No data | Yes |
| Remifentanil-midazolam | Intravenous | Arpaci [64] | 2013 | 40 | Both | No data | Yes |
| Ketamine | Intraurethral (possible cystitis) | Moharari [65] | 2010 | 60 | Men | Rigid | Yes |
| Dexmedetomidine-ketamine | Intravenous | Modir [67] | 2020 | 60 | Both | No data | Yes |
| Acetaminophen | Oral/Intravenous | Kor [68] | 2020 | 3566 | Both | No data | Yes |
| Sodium bicarbonate (Ural) | Oral | Wong [69] | 2011 | 300 | Both | Flexible | No |
It has been proven that premedication of different non-steroidal anti-inflammatory drugs (NSAIDs) is effective in CS. For example, oral and intrarectal diclofenac, oral zaltoprofen and intramuscular parecoxib administration before the procedure all decreased pain associated with CS (based on VAS scores) [58–61]. That is why it is safe to assume that the majority of NSAIDs, regardless of the way of administration, can increase patients’ comfort during CS. Anti-inflammatory drugs, however, can cause various adverse effects, including gastrointestinal ulceration and higher risk of bleeding [58]. Therefore, NSAIDs are contraindicated in patients with peptic ulcer disease, bleeding diatheses, renal insufficiencies and aspirin hypersensitivity.
Benzodiazepines are the second group of medications that can be used in order to lower the pain levels during CS. Pre-operative midazolam and alprazolam are highly effective not only in pain management but also in anxiety reduction (based on VAS and STAI) [62, 63]. Generally, these benzodiazepines are safe and well tolerated by the patients, but possible side effects include respiratory depression [62–64]. That is why midazolam and alprazolam should not be used in patients with myasthenia gravis, chronic obstructive pulmonary disease, bronchitis and sleep apnea. Arpaci and Bozkirli used a combination of midazolam and remifentanil, achieving sufficient pain reduction, while suggesting that dexmedetomidine-remifentanil is a superior drug combination [64]. Dexmedetomidine does not cause respiratory depression in therapeutic doses, while the same adverse effect is the most dangerous in remifentanil use [64]. Therefore, remifentanil cannot be administered in patients with respiratory instability.
Ketamine can also be used in order to manage the pain during CS. Moharari et al. proposed an interesting approach of intraurethral injection of 100 mg of ketamine mixed with 10 ml of 2% lidocaine gel before the CS [65]. The results of the study were satisfactory, but the technique was criticized, due to possible ketamine related cystitis [66]. That is why intraurethral injection of ketamine remains controversial and intravenous administration of dexmedetomidine-ketamine is a recommended method providing efficient anesthesia and sedation [67]. Ketamine is mainly contraindicated in patients with heart diseases, due to hypertension caused by the drug.
Moreover, other drugs can also be used successfully, such as pipemidic acid, phenazopyridine and paracetamol [61, 68]. A comparison between the oral administration of pipemidic acid, phenazopyridine and diclofenac indicated that pipemidic acid was superior to the other two drugs (based on the VAS score) [61]. Pipemidic acid and phenazopyridine are contraindicated in patients with severe renal and hepatic insufficiencies.
Finally, a study comparing oral and intravenous paracetamol use in ambulatory CS showed no difference in pain levels, with more complications after intravenous administration of acetaminophen [68]. This leads to the conclusion that parenteral administration of analgesics should be avoided unless necessary.
Unfortunately, the research concerning sodium bicarbonate proved that it does not lower the pain associated with urination after CS [69].
Other methods
Despite the abundance of previously described ways of pain management, there are still a few that do not fall directly into any of the previously mentioned categories (Table 7).
Table 7
Other methods of pain reduction during cystoscopy
| Method | Name of first author | Year of publication | Number of patients | Gender | Type of cystoscopy | Significant pain reduction |
|---|---|---|---|---|---|---|
| Hypnosis | Tezcan [70] | 2021 | 90 | Men | Rigid | Yes |
| Heating pad | Kim [71] | 2019 | 74 | Women | Rigid | Yes |
| Glandular lidocaine injection | Gooran [72] | 2017 | 156 | Men | Rigid | Yes |
| Hand-holding | Kwon [73] | 2018 | 86 | Men | Flexible | Yes |
| Transcutaneous electrical nerve stimulation | Hruby [74] | 2006 | 148 | Both | Flexible | No |
| Anesthesia of posterior urethra | Poletajew [75] | 2017 | 127 | Men | Rigid | No |
One of the most recent studies published in 2021 legitimated hypnosis as helpful in reducing pain and anxiety caused by rigid CS (based on VAS, STAI and hemodynamic parameters) [70]. Application of heating pads to the women’s sacra was proved effective in rigid CS as well (based on VAS, STAI and hemodynamic parameters) [71]. In men, the additional injection of lidocaine into the glans penis before the procedure served a major role in pain level reduction (based on VAS score) [72]. Lastly, even holding the patient’s hand during CS played a significant role in lowering the pain and improving the patient’s comfort (based on VAS and STAI scores) [73].
On the other hand, transcutaneous electrical nerve stimulation and additional anesthesia of the posterior urethra did not provide any benefit in pain reduction (based on VAS score, overall pain intensity assessed on a Likert scale and the need for analgesics during 6 h after the procedure) [74, 75].
The diversity of these methods and their effectiveness prove that CS is connected not only with physical pain, but also with psychological discomfort.
Conclusions
This review focused on a variety of possible methods of pain reduction during CS. Lidocaine gel should be used until it is undoubtedly proven ineffective. In order to increase patients’ comfort it needs to be cold and instilled slowly 15 minutes before the procedure. Micturition and provision of high irrigation pressure during the insertion of the scope may be also helpfull in males. Analgesic drugs benefit patients undergoing CS. Distractions, such as video, music, stress ball or self-visualization might alleviate the pain. Additionally, nitrous oxide, heating pads, hand holding, hypnosis or lidocaine injection into the glans have been proven effective. Sodium bicarbonate, transcutaneous nerve stimulation and additional anesthesia of the posterior urethra do not lower pain levels during CS.