Introduction
Cancer of the oral cavity most commonly affects the lateral border of the tongue and the floor of the mouth. These structures are vital to mastication and are often subject to displacement, gross resection, or modification during surgical management. This has significant consequences relating to the function and aesthetic properties of the mouth, and impaired masticatory function has previously been reported in approximately 40% of patients treated for head and neck cancer [1–9].
There are three components of mastication that allow for it to occur efficiently: manipulation, trituration, and consolidation. Mandibulectomies, partial or complete, have a variety of functional, sensory, and aesthetic consequences. Normal mastication involves the synchronous interaction of the hard and soft tissues to manipulate a food bolus prior to deglutition. The grinding and trituration phase in addition to sensory and soft tissue deficits following a mandibulectomy are what compromise the patient’s ability to manipulate a bolus to the occlusal table for trituration and the ability to retrieve and consolidate the bolus prior to deglutition [5, 6, 10].
The current standard for reconstruction of large mandibular defects is the use of free fibular flaps (FFF). This method has been assessed through comprehensive long-term follow-up studies assessing facial appearance, speech, food tolerance, and deglutition, which have been deemed to be satisfying. Advancements in surgical techniques and microvascular surgery have now enabled reconstructive outcomes to reach those of pre-surgery levels with good functional and aesthetic results. However, reconstructive options using bone grafts are not without complications. Plate exposure, soft tissue deficiency, and mandibular contour deformation of the lateral face have all been cited as major reasons for a further, second operation. In addition, extended operative and anaesthetic times, increased morbidity associated with vascularised bone containing free flaps (VBCFF), and increased postoperative complication rates associated with bone grafts have been reported [2, 3, 7, 9, 11–13].
The benefits of mandibular reconstruction to mastication remain unclear. Komisar compared the masticatory function in patients with composite resection versus no mandibular reconstruction and concluded that the reconstructed patients had lower scores. He also reported that prosthetic rehabilitation benefitted neither reconstructed nor non-reconstructed patients [6].
Other published literature suggests that there is a significant improvement in masticatory function, aesthetic appearance, and general quality of life after mandibular reconstruction. This has been objectively measured through increased electromyography (EMG) activity of the masseter and temporalis muscles in addition to an increased bite force. Urken et al. found that patients with dental implant-supported prostheses and mandibular reconstruction had significantly increased levels of bite force, a more vertical masticatory cycle, improved chewing performance, and better speech compared with non-reconstructed patients [1–3, 9, 13].
Prior to the introduction of VBCFF, segmental mandibulectomy defects were left unreconstructed. The consequences of such action included malocclusion, obvious aesthetic defects, speech impairments, mandibular swing, and a diet restricted to soft foods only [1, 6, 8].
Even with the current literature, the benefit of extensive mandibular reconstruction for patients with large oral cancer and multiple co-morbidities is unclear. The increased surgical and anaesthetic risk associated with bone harvesting and postoperative complications necessitating further surgical operations may deem reconstruction an inappropriate management option for a certain subset of patients [2, 3, 9, 13, 14].
Material and methods
Between January 2010 and July 2018 a total of 23 patients were included in the study, with a cT4 stage cancer of the oral cavity or of the floor of the mouth. Complete staging was undertaken for each patient, which included a panendoscopy with mapping biopsies and computed tomography (CT) imaging of the head, neck, thorax, and abdomen. Cases were fully discussed in the head and neck multidisciplinary team meeting (MDT) after complete staging.
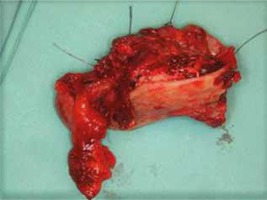
Where clinically feasible, complete tumour removal including parts of the mandible and a bony reconstructive option was offered to all patients. Reconstruction was not offered to: patients with multiple comorbidities, patients who were not considered to be fit enough for a longer anaesthesia, those with inappropriate anatomy, and those who were more suitable for a primary intensity-modulated radio-chemotherapy (IMRT). The cohort of patients was either not appropriate for reconstruction or declined this surgical option and also declined primary IMRT, and thus they underwent a partial mandibulectomy to excise the tumour (Fig. 1) without bony reconstruction but may have had soft tissue reconstruction. We performed the continuity resection of the mandible as described by Jewer et al., as follows: lateral continuity defect (n = 20) and hemimandibular continuity defect (n = 3) [15]. Figure 2 shows an orthopantomogram six months postoperatively. After surgical removal of the tumour (including an ipsi- or bilateral neck dissection and, if necessary, a tracheostomy placement) the histopathology confirmed a pT4 squamous cell carcinoma for all patients. Two patients had a pN0, three patients a pN1, 12 patients a pN2b, four patients a pN2c, and two patients a pN3 status. Six patients underwent soft tissue reconstruction for defect closure and bone coverage, using a pectoralis major flap. Although the use of a pedicle flap again exposes the patient to a slightly longer operation and anaesthesia time, soft tissue flaps tolerate active smoking, alcohol, and post-operative IMRT better than no reconstruction at all, and thus they can be used to simply obtain wound closure and avoid later complications. Care was taken with all soft tissue reconstructions to ensure that they were not performed under tension. All patients were re-discussed at the Head and Neck Cancer MDT and if indicated underwent IMRT for six weeks.
Regular patient follow-up appointments were undertaken, which included clinical examinations, panendoscopies with biopsies, and CT imaging of the head, neck, thorax, and abdomen. The postoperative follow-up period for the study was between 5 and 50 months (average of 27.3 months), and the results were evaluated in terms of local tumour control. Patients were asked to assess their ability to open their mouth, level of pain while masticating, mastication function pre and post-surgery, aesthetic outcome post-surgery, and photo documentation was carried out (Fig. 3), prior to surgery and four months after therapy completion.
Results
We included 23 patients, 6 female and 17 male, with an average age of 59.8 years (range 43–75 years). The patient population consisted of 19 oropharyngeal carcinomas and four floor of the mouth cancers, all of which had a stage of cT4. Of the 23 patients included in the study, there were 20 lateral defects (comprising a combination of defects in the body, ramus, and condyle of the mandible) and three anterolateral defects of the mandible. No difference in aesthetic outcome was noted between the lateral or anterolateral defects; however, the functional outcome was assessed to be better for the patients who had a lateral defect. Four patients showed minor wound healing complications postoperatively, which were successfully treated conservatively. IMRT was started in all patients after completed wound healing. There was no evidence of local tumour recurrence in the follow-up period for any patient. This was based on control-panendoscopy with biopsies and CT imaging. Eight patients developed regional or distant metastases and have since died (one base of the skull metastasis, two liver metastasis, two lung metastasis, one lung and liver combined metastasis, and two bone metastasis). These eight patients had at least a pN2b status. One patient was diagnosed with a metachronic secondary tumour 10 months after partial mandibulectomy at the contralateral oropharynx, which was consecutively resected in total.
All patients had the same or an improved level of jaw opening four months after therapy completion (seven patients with moderate and 10 with severe impairment of the jaw opening before therapy compared to six patients with either moderate or severe impairment of jaw opening after treatment). 17/23 patients deemed the cosmetic result to be satisfying and 4/23 patients scored the cosmetic results as “slightly worse” postoperatively but not severe enough to seek a second surgery for reconstruction. Seventeen of the 23 patients reported a slight or massive improvement of mastication function after therapy, and just one patient reported a massive worsening. Seven patients reported unbearable pain pre-treatment, and none reported unbearable pain post-treatment (Table 1).
Table 1
Pre- and postsurgical results after partial mandibulectomy without bony reconstruction
Discussion
Tumours (benign or malignant), osteoradionecrosis, osteomyelitis, or trauma sometimes lead to large segmental resections of the mandible. Resection of a significant portion of the mandible in patients with T4-stage cancer with or without bony reconstruction has previously been documented in the literature with varying results. Previous investigators have reported improvements to mastication function and aesthetic appearance with bony reconstruction; however, the extensive surgery and anaesthesia times are not without complications. On the other hand, in addition to the cosmetic deformity, failure to reconstruct the partial mandibulectomy defect can also result in malocclusion, mandibular swing, temporomandibular joint pain, and a diet restricted to soft foods [2–5, 7, 11, 12, 14, 16].
Reconstruction is possible with a VBCFF. The harvesting of ilium, scapula, radius, humerus, ulna, and fibula allow for transfer of bone, soft tissue, and skin as a single-stage procedure from a donor site. The current standard for reconstruction of large mandibular defects is the use of a free fibula flap. However, the use of free flaps is not possible in certain cases where there are a lack of recipient vessels or irradiated vessels, which could rupture at a later date. [17]. If the reconstruction is possible, however, there is often criticism over the increased operative time associated with the microvascular free tissue transfer, in addition to the increased length of hospital stay and increased morbidity associated with high-risk patients [2, 4, 18–22]. Holzle reported in 2007 on a study group of 54 patients, after mandibular reconstruction with free fibula flap more disturbances occurred at the recipient than at the donor site. In this same study cohort, 62% of female subjects and 34% of male subjects judged their postoperative aesthetic outcome as poor [4]. Previous clinician-rated assessments that evaluated the recipient region recorded excellent or good postoperative results in 58–75% of cases, acceptable or fair results in 15–38%, and poor results in only 4–10%. As a relatively new technology becomes more readily available, such as marked virtual surgical planning (VSP), the area of reconstructive surgery is gaining wider acceptance due to its many perceived benefits including increased accuracy, improved operative efficiency, and enhanced outcomes [9, 13, 18, 23].
Another alternative is to reconstruct the mandible using a titanium plate. Maurer et. al reported a complication rate of 37% after the use of reconstruction plates and Klotch et al. had a complication rate of 45% in 309 patients. Alloplastic mandibular reconstruction by titanium or steel plates appears to be associated with a high rate of complications in patients with tumours. Biological factors such as the age of the patient, smoking or alcohol intake, and use of radiotherapy are the main reasons for complications [7, 24].
Resection of the mandible without bony reconstruction is a valid management option in carefully selected patients with extensive tumour growth [21]. Elderly patients with multiple co-morbidities, heavy smoking histories, and alcohol dependence are often more suitable for resection without bony reconstruction, provided that it is an aesthetically acceptable option to the patient (Fig. 3) [5, 22]. It should also be mentioned that with the partial removal of the mandible without bony reconstruction, a long-term supply of dental implants is not possible. There is consensus that free-flap mandibular reconstruction and implant placement is worthwhile, but only a small percentage of patients will benefit from complete dental rehabilitation. Hundepool et al. reported this at a rate of 25% [5].
All our 23 patients had excellent local tumour control in the follow-up period. A reasonable opening of the mouth and chewing function is guaranteed and deemed acceptable by the majority of patients. The cosmetic result is satisfying and of secondary concern to the population cohort in this study. Furthermore, all patients showed an improvement of pain while opening the mouth after therapy. Finally, no complications during the IMRT occurred.
Conclusions
Our findings illustrate that partial mandibulectomy without bony reconstruction can be an appropriate and acceptable surgical option for patients who have extensive and large tumours and who would otherwise not be ideal candidates for reconstruction or long anaesthesia due to other comorbidities. A thorough preoperative work up is required, and discussion with a multidisciplinary team is a necessity. This treatment option is more acceptable to the patient than would be expected and provides a satisfying functional and aesthetic outcome.