Introduction
Chronic kidney disease (CKD) is a progressive condition affecting more than 10% of the world’s population [1]. Vascular access is among the most critical issues impacting the quality of life in dialysis-dependent chronic kidney failure patients. The primary problems associated with arteriovenous fistulas (AVF) and permanent tunneled catheters (PTC) include stenosis, thrombosis, fibrin formation, infection, bleeding, and aneurysm [2–4]. Nephrology guidelines recommend starting with the most distal arteriovenous fistula site using Doppler ultrasonography for vessel mapping. In cases where an arteriovenous fistula cannot be established, an algorithm for the use of arteriovenous grafts is suggested [5].
Aim
The aim of this study was to examine the epidemiological data on the use of arteriovenous fistulas in different forearm regions of dialysis-dependent chronic kidney disease patients. It also aimed to identify the factors that affect vascular access maturation and patency. In addition, the study evaluated the rates of tunneled catheter use and related infections.
Material and methods
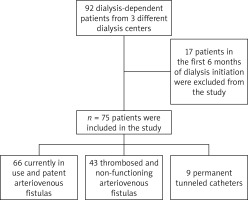
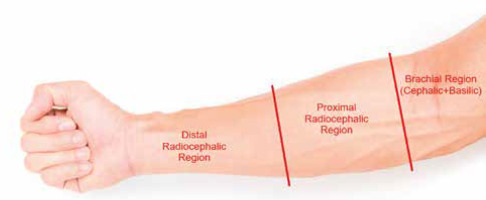
A total of 75 end-stage renal disease patients over the age of 18, who had been on routine dialysis for at least 6 months between January 2023 and January 2024 at three different dialysis centers, were included in the study. Patients with arteriovenous fistulas and permanent catheters were included in the study. Seventeen patients who had started dialysis within the last 6 months were excluded from the study. Data collection involved file reviews from the archives of hospital and face-to-face interviews with patients in the dialysis centers. Among these 75 patients, there were 66 actively used patent arteriovenous fistulas, 43 thrombosed or nonfunctional arteriovenous fistulas, and 9 actively used permanent tunneled catheters (Figure 1). AVFs were created in nine different surgical centers. There were no patients with arteriovenous grafts among the study participants. AVFs were examined in three groups according to their forearm locations: distal radiocephalic AVF, proximal radiocephalic AVF, and brachial region AVF (brachiocephalic + brachiobasilic AVF) (Figure 2). Distal AVFs were defined as those created in the distal half of the forearm, proximal AVFs as those in the proximal half of the forearm, and brachial region AVFs as those created using the brachial artery.
Figure 2
In our study, arteriovenous fistulas were grouped according to their location on the forearm
The primary endpoints of the study were the maturation times of arteriovenous fistulas according to their forearm locations, failure rates, factors affecting failure, rates of permanent catheter use, and permanent catheter infection rates. The secondary endpoint was to determine the demographic characteristics of dialysis patients.
Statistical analysis
The data obtained from the study were evaluated using the SPSS Statistics 21.0 (IBM Corp.) program. The Shapiro-Wilk test was performed to assess the normality of the data distribution. Descriptive statistics were presented as numbers and percentages; median values were presented with minimum and maximum values; mean values were presented with standard deviations. The Mann-Whitney U test was used to evaluate the relationship between numerical values of binary independent variables; the Kruskal-Wallis test was used to evaluate the relationship between numerical values of more than two independent variables. After the Kruskal-Wallis test, Bonferroni correction was made for pairwise comparisons of multiple groups. The c2 test was used to evaluate the relationship between categorical variables. The Type 1 error level was accepted as α = 0.05.
Results
Of the patients, 66.7% were male, and the average age was 61.1 ±12.2 years. The demographic information and medical histories of the patients are provided in Table I.
Table I
General characteristics of patients
The average duration of dialysis for the patients was 58.9 ±72.2 months. The average frequency of weekly dialysis sessions was 2.8 ±0.4. The average maturation time of arteriovenous fistulas was 39.3 ±19.8 days, and the average patency time of vascular access was 39.0 ±42.4 months. The most frequently used patent arteriovenous fistulas for dialysis access were brachial region AVFs at 38.7%. Additionally, 36.0% had distal radiocephalic fistulas, 13.3% had proximal radiocephalic fistulas, and 12.0% were dialyzed using permanent catheters. There was no significant difference in the average maturation times between distal fistulas (37.4 (20.0–60.0) days), proximal fistulas (39.0 (30.0–60.0) days), and brachial fistulas (38.1 (10.0–132.0) days) (p = 0.88). Patients using permanent catheters had fewer dialysis sessions per week compared to those using distal, proximal, or brachial fistulas (p = 0.001). The current dialysis-related data of the participants are provided in Table II.
Table II
Current dialysis access and dialysis characteristics of patients
The patency durations and maturation times of the currently used arteriovenous fistulas and the factors associated with them are provided in Table III.
Table III
Factors associated with AVF patency and maturation times
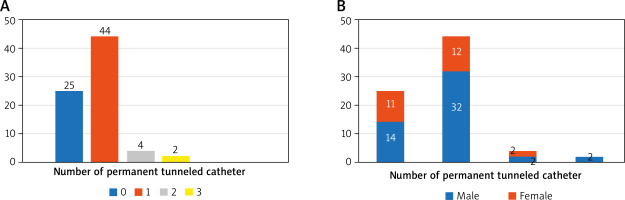
Patients with diabetes had shorter median maturation times than those without diabetes. Similarly, patients under 65 years of age had shorter median maturation times than those over 65 (p < 0.05). Patients over 65 had shorter median primary patency than younger patients, and obese patients had shorter median primary patency than non-obese patients (p < 0.05). Of the participants, 12.0% were undergoing dialysis with a permanent catheter at the time of the study. Among those using permanent catheters (n = 9), 77.8% (n = 7) used it by personal preference, and 22.2% (n = 2) used it due to heart failure. Additionally, 66.7% of the participants had used at least one permanent catheter in their lifetime (Figure 3). The average number of permanent catheters used by those who had used at least one permanent catheter (n = 50) was 1.2 ±0.5, with a minimum of one and a maximum of three permanent catheter uses. Among these individuals, 12.0% (n = 6) had used more than one permanent catheter.
Of the participants who had used at least one permanent catheter in their lifetime (n = 50), 4.0% (n = 3) experienced a permanent catheter infection. Catheter infections were more common in the presence of hyperlipidemia and coronary artery disease (p < 0.05).
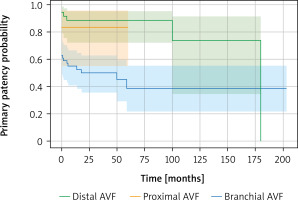
Among the 75 end-stage renal disease patients participating in the study, there were a total of 109 AVFs, 43 of which were thrombosed/nonfunctional and 66 were actively used. Considering all AVFs, the AVF failure rate was 39.4%. When all AVFs were compared in terms of primary patency using the log-rank test, the results were as follows: distal vs. brachial: p < 0.001, proximal vs. brachial: p = 0.572, distal vs. proximal: p = 0.042. A statistically significant difference was observed between distal and brachial AVFs (p < 0.001), as well as between distal and proximal AVFs (p = 0.042). However, no significant difference was found between proximal and brachial AVFs (p = 0.572) (Figure 4). Among the patients, 41.3% had thrombosed distal fistulas, 2.7% had proximal fistulas, and 8.0% had brachial fistulas. There was no association between the number of thrombosed fistulas and smoking, obesity, gender, or chronic diseases (Table IV). When considering thrombosed/nonfunctional AVFs, there was no significant difference in the median primary patency durations between distal fistulas, proximal fistulas, and brachial fistulas (p = 0.51). Similarly, there was no significant difference in the median maturation times between distal fistulas, proximal fistulas, and brachial fistulas (p = 0.72). There was no association between gender, age, smoking, obesity, or chronic diseases and the primary patency duration or maturation time of thrombosed fistulas (p > 0.05).
Table IV
Factors associated with the number of thrombosed/non-functional fistulas
Discussion
Although AVFs are generally created starting distally, the fact that the active access site for dialysis at the time of the study was the brachial region and that 41.3% of the patients had non-functional distal radiocephalic AVFs provides significant insights into how frequently and early distal region AVFs become occluded. Farber and colleagues, in a 2014 study of 602 end-stage renal disease patients, reported significantly higher early thrombosis rates in forearm fistulas compared to upper arm fistulas [6]. Weale et al., in a study of 658 patients comparing patency rates of brachial and radial arteriovenous fistulas by age, found that brachial region arteriovenous fistulas had significantly higher patency rates at 2 years, with this difference increasing with age [7]. In our study, the brachial region was the most frequently used access site for dialysis. We also observed that maximum patency durations decreased with age above 65.
In our study, the average AVF maturation time was found to be 39.3 days, similar to current studies. Khavanin Zadeh et al. found an average maturation time of 38.6 days, while Eroglu et al. reported an average maturation time of 40 days [8, 9]. In our study, there was no significant difference in maturation times between proximal radiocephalic, distal radiocephalic, and brachial regions. Supporting our study, there are studies showing that AVF localization and thus vein diameter do not affect fistula maturation time [10]. However, there are also studies suggesting that vein diameter is a factor affecting fistula maturation [11].
In line with current studies, our study found that patients under 65 years had significantly shorter average maturation times and significantly higher average patency durations compared to those over 65 years. A study of 941 fistulas, by Misskey et al., demonstrated that advanced age negatively affected both patency and maturation [12]. This may be due to poorer vessel quality or a predisposition to thrombosis in older patients. On the other hand, some studies did not identify any factors associated with patency durations [13].
In our study, 12% of the patients were undergoing dialysis with a permanent catheter for various reasons. The rate of catheter infections among those who had used at least one permanent catheter in their lifetime was found to be 4%. Karkar et al., in a 2014 study, reported a similar infection rate of 6.1% for permanent catheters [14]. Develter et al., on the other hand, found a catheter infection rate of 0.6% over a 1000-day period [15]. The lower infection rate in Develter’s study compared to our study may be due to the 1000-day limit set for the infection rate in their study.
Keser et al. conducted a study in 2021 on dialysis patients in Istanbul. They reported an 18.9% failure rate for newly created AVFs within the last 1.5 years. They also examined the relationship between AVF failure and factors such as diabetes, hypertension, and peripheral vascular disease, but found no statistically significant association [16]. In our study, we also investigated the relationship between the number of thrombosed fistulas and conditions such as diabetes, hypertension, peripheral vascular disease, and obesity, but found no significant results. On the other hand, the AVF failure rate in our study was 39.4%. The higher failure rate in our study compared to the 18.9% failure rate found by Keser et al. in Istanbul may be due to our study including all AVFs in dialysis centers, while Keser et al.’ study included only AVFs established in the last 1.5 years.
Our study has several limitations. Firstly, no patients with arteriovenous grafts were included in the study. Additionally, the number of patients was relatively limited for an epidemiological study.
Conclusions
The most frequently used dialysis access route during the study period among the participating patients was brachial region arteriovenous fistulas at 38.7%. There was no significant difference in maturation times between distal radiocephalic, proximal radiocephalic, and brachial region arteriovenous fistulas. Advanced age negatively affects both fistula maturation and patency. The rate of permanent catheter infection among patients who had used at least one permanent catheter in their lifetime was found to be 4%. Approximately half of dialysis-dependent patients (41.3%) have a thrombosed/nonfunctional distal radiocephalic fistula. Considering all arteriovenous fistulas, the AVF failure/thrombosis rate was 39.4% at a median follow-up period of 36.0 months (IQR: 12.0–72.0). To obtain better epidemiological results in dialysis access, more studies with higher patient numbers are needed.