The neck is a complex anatomical area that occupies unique vital structures. They can be severely damaged in any perforating neck trauma, leading to considerable morbidity and mortality. Non-iatrogenic internal jugular vein (IJV) injuries are rare, and no specific guidelines exist regarding their optimal treatment [1]. We present a rare case of an extended IJV transaction and massive exsanguination through a perforating neck trauma. External digital compression at the scene of the accident and urgent surgical exploration in our tertiary hospital saved the patient’s life. A 50-year-old male patient after a car accident presented to a local hospital with confusion, hypotension (systolic blood pressure (SBP) = 50 mm Hg), and massive bleeding from a zone II neck trauma at the left side. He was a motorcycle driver who crashed into a car and the mirror of the car injured his neck. At the accident scene, hemorrhage was controlled with digital compression by a medical practitioner, who happened to be there, and the patient was transferred to the local hospital. The penetrating wound was filled with gauzes and the hemorrhage was controlled with continued digital pressure. He was intubated and a splint was placed in the right leg due to a ligament contusion causing knee instability. The patient was transferred to our tertiary hospital (40 km away from the local hospital) and underwent urgent surgical exploration. Skin scrubbing was performed keeping the digital pressure in the wound continuously. Skin incision had a curved lateral extension to include the wound, but the following approach was the standard vascular exposure for carotid endarterectomy (Figure 1). The common carotid artery and internal jugular vein were circumferentially looped proximally and distally, but the in-between segments were not dissected (Figure 2 A). Traction of IJV vessel-loops seemed to control the hemorrhage and no external compression was needed at the injury site. Exploration continued posteriorly to the sternocleidomastoid muscle, where the injury path was directed, and an extended internal jugular vein transection was revealed (Figure 2 B). Primary suturing was performed, leading to stenosis (Figures 2 C, D). A drain was secured in place. Postoperatively the patient underwent bone X-rays, brain, chest, and abdominal computed tomography (CT), carotid computed tomography angiography (CTA), and brain computed tomography phlebography (CTV). The findings were a brain contusion and an obstruction of the left internal jugular vein but with a patent lumen distally. The patient was then extubated and 2 days later underwent a normal barium-swallow study. He was discharged on the 5th postoperative day with anticoagulants for 3 months and instructions for his mild knee injury. Internal jugular vein injuries after blunt or penetrating neck trauma may occur in conjunction with injuries to carotids or the nearby structures of the aerodigestive and musculoskeletal systems. They have been reported to occur in 10–20% of penetrating neck trauma cases [1, 2]. They may present as an arteriovenous fistula, IJV thrombosis, airway compromise due to compressing neck and/or mediastinal hematomas, or exsanguinating hemorrhage from an open neck wound [1]. The most frequent cause of IJV injury is the placement of central venous catheters, where concomitant injuries to the nearby carotids and vertebral arteries, brachiocephalic veins, trachea, brachial plexus, thoracic duct, lymph vessels, and lung have been reported. Surgical oncology procedures in the neck represent another cause of iatrogenic IJV injuries. Non-iatrogenic IJV penetrating injuries may occur after stab or gunshot trauma with concomitant injuries to nearby structures or may be isolated. Rare causes of IJV injury such as fishbone ingestion and a rare complication of lung embolism from a piece of iron that migrated via the IJV lumen have been reported [3, 4]. In a recent publication from our department, only 5 isolated IJV injuries were identified among 109 isolated venous injuries [5]. Moreover, there are limited publications and data in the literature regarding the presentation and management of non-iatrogenic IVG injuries. Penetrating IJV injury usually affects young men in their 30s and 40s [1]. Two-thirds are due to stabbings and one-third due to gunshot injuries. Firearms cause greater local damage leading to higher morbidity and mortality than stab wounds. In the absence of injuries of the nearby structures, isolated venous injuries may present with hard or soft signs of a vascular injury [5]. Patients are usually normotensive, in contrast with our patients. A minority of them (about 20%) may present with coma due to massive exsanguination [1]. In a recent series of 271 IJV penetrating injuries, hypotension (SBP < 90 mm Hg) was noted in only 15% of patients [1]. In unstable patients or with active bleeding, the venous injury is typically recognized in the operative field [6]. Traditionally, bleeding from the maxillofacial region is commonly controlled by gauze packing, external digital compression, and balloon tamponade, especially in deep wounds [5, 6]. The balloon (a Foley catheter) is removed after 24–72 hours and at least in 50–70% of cases bleeding stops and no exploration is required [7]. Symptomatic penetrating zone II injuries traditionally undergo neck exploration. This is the largest zone and the most injured in the neck. It has easy access for clinical examination and surgical exploration in comparison with zones I and III, where access is difficult and endovascular treatment is usually more suitable [7]. After the evolution of CTA, selected patients with soft signs of an isolated IJV injury may be treated conservatively. This policy led to a reduction in negative neck explorations from 40–60% to 7% [1]. Consequently, in the absence of hard signs, patients with penetrating zone II injuries may be treated with either obligatory exploration or directed evaluation and serial examinations. A difference in mortality was observed between these two groups according to a recent publication (4.7% vs. 4.8%) [1]. The frequency of non-operative management varies between 18.2% and 48.7%. Zone ll injuries have the best prognosis, compared with zones I and III [1, 2]. When less than 50% of the wall is lacerated, the vein can be repaired with lateral venorrhaphy. The neck veins can be ligated in extended injuries and/or unstable patients with no major complications [1, 5]. In a recent publication, 73.2% of neck vein injuries were treated with ligation [5]. Cerebral edema is rare after internal jugular vein ligation, even bilaterally [2, 3]. Extensive vein repairs (end-to-end, venous interposition, or spiral/panel grafts) typically do not have a role in penetrating neck injuries when time is critical. All repairs are at risk of thrombosis and thus thromboprophylaxis should be prescribed. Endovascular venous repair with covered stents has been rarely described with good technical results and perhaps will be progressively used more for isolated venous injuries on stable patients in the future [4]. Non-iatrogenic IJV injuries usually present with injuries to other neck structures. Even isolated, they are life-threatening due to exsanguination or airway compromise. The best management includes digital pressure or balloon occlusion to control exsanguination, intubation in a threatened airway from a potential expanding hematoma, fluid resuscitation, and transfer to a specialized center with vascular capabilities.
Figure 1
Skin incision was performed along the sternocleidomastoid muscle but with a curved lateral extension to include the stab wound (green arrow: sternal notch, red arrow: ear lobe, blue line: anterior border of the sternocleidomastoid muscle)
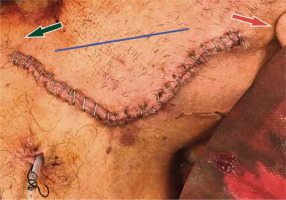
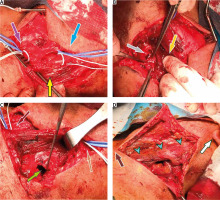
Figure 2
A – The common carotid artery and internal jugular vein were circumferentially looped proximally (purple arrow) and distally (blue arrow), but the in-between segments were not dissected (yellow arrow). Digital pressure remained at the injured area (yellow arrow). B – Internal jugular vein (IJV) extended transection (gray arrow). Digital pressure at the cephalic portion of the IJV was performed to aid hemostasis, in addition to vessel loop traction (orange arrow). C – Primary IJV suturing led to stenosis (light green arrow). Proximal vessel loops (maroon arrow), distal vessel loops (brown arrow). D – Operative field after repair (light blue arrows: sternocleidomastoid muscle, white arrow: ear lobe, dark brown arrow: sternal notch).